Severe acute respiratory syndrome coronavirus 2
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)[3] is the strain of coronavirus that causes coronavirus disease 2019 (COVID-19), the respiratory illness responsible for the COVID-19 pandemic. Colloquially known as simply the coronavirus, it was previously referred to by its provisional name, 2019 novel coronavirus (2019-nCoV),[4][5][6][7] and has also been called human coronavirus 2019 (HCoV-19 or hCoV-19).[8][9][10][11] The World Health Organization declared the outbreak a Public Health Emergency of International Concern on 30 January 2020, and a pandemic on 11 March 2020.[12][13]
| Severe acute respiratory syndrome coronavirus 2 | |
|---|---|
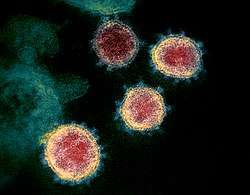 | |
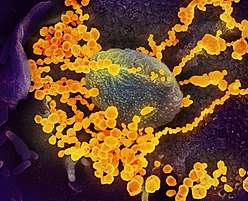
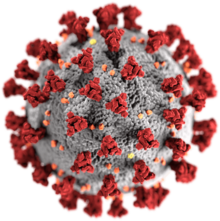
| Transmission electron micrograph of SARS-CoV-2 virions with visible coronae | |
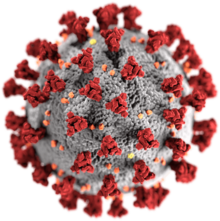 | |
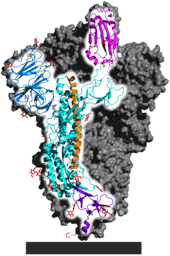
| Illustration of a SARS-CoV-2 virion[1] Red protrusions: spike proteins (S)[1] Grey coating: the envelope, composed mainly of lipids, which can be destroyed with alcohol or soap[1] Yellow deposits: envelope proteins (E)[1] Orange deposits: membrane proteins (M)[1] | |
| Virus classification | |
| (unranked): | Virus |
| Realm: | Riboviria |
| Kingdom: | Orthornavirae |
| Phylum: | Pisuviricota |
| Class: | Pisoniviricetes |
| Order: | Nidovirales |
| Family: | Coronaviridae |
| Genus: | Betacoronavirus |
| Subgenus: | Sarbecovirus |
| Species: | Severe acute respiratory syndrome-related coronavirus |
| Strain: | Severe acute respiratory syndrome coronavirus 2 |
| Synonyms | |
| |
SARS-CoV-2 is a positive-sense single-stranded RNA virus[14] that is contagious in humans.[15] As described by the U.S. National Institutes of Health, it is the successor to SARS-CoV-1,[10][16] the strain that caused the 2002–2004 SARS outbreak.
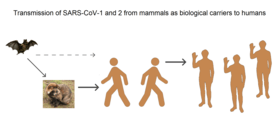
Taxonomically, SARS-CoV-2 is a strain of severe acute respiratory syndrome-related coronavirus (SARSr-CoV). It is believed to have zoonotic origins and has close genetic similarity to bat coronaviruses, suggesting it emerged from a bat-borne virus.[17][18][19][9] There is no evidence yet to link an intermediate animal reservoir, such as a pangolin, to its introduction to humans.[20][21] The virus shows little genetic diversity, indicating that the spillover event introducing SARS-CoV-2 to humans is likely to have occurred in late 2019.[22]
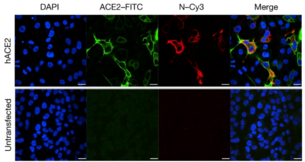
Epidemiological studies estimate each infection results in 1.4 to 3.9 new ones when no members of the community are immune and no preventive measures taken. The virus primarily spreads between people through close contact and via respiratory droplets produced from coughs or sneezes.[23][24] It mainly enters human cells by binding to the receptor angiotensin converting enzyme 2 (ACE2).[17][25][26][27]
Terminology

During the initial outbreak in Wuhan, China, the virus was commonly referred to as the "coronavirus" or "Wuhan coronavirus",[28][29][30] or "Wuhan virus".[31] In January 2020, the World Health Organisation recommended "2019 novel coronavirus" (2019-nCov)[32][5] as the provisional name for the virus. This was in accordance with WHO's 2015 guidance[33] against using geographical locations, animal species, or groups of people in disease and virus names.[34][35] On 11 February 2020, the International Committee on Taxonomy of Viruses adopted the official name "severe acute respiratory syndrome coronavirus 2" (SARS-CoV-2).[20] To avoid confusion with the disease SARS, the WHO sometimes refers to SARS-CoV-2 as "the COVID-19 virus" in public health communications[36][37] and the name HCoV-19 was included in some research articles.[8][9][10] The general public often call both SARS-CoV-2 and the disease it causes "coronavirus". U.S. President Donald Trump referred to the virus as the "Chinese virus" in tweets, interviews, and White House press briefings.[38][39][40]
Virology
Infection and transmission
| Part of a series on the |
| COVID-19 pandemic |
|---|
 |
|
|
|
International response |
|
Medical response |
|
|
|
Human-to-human transmission of SARS-CoV-2 was confirmed on 20 January 2020, during the COVID-19 pandemic.[15][41][42][43] Transmission was initially assumed to occur primarily via respiratory droplets from coughs and sneezes within a range of about 1.8 metres (6 ft).[24][44] Laser light scattering experiments suggest speaking as an additional mode of transmission.[45][46] Indirect contact via contaminated surfaces is another possible cause of infection.[47] Preliminary research indicates that the virus may remain viable on plastic (polypropylene) and stainless steel (AISI 304) for up to three days, but does not survive on cardboard for more than one day or on copper for more than four hours;[10] the virus is inactivated by soap, which destabilises its lipid bilayer.[48][49] Viral RNA has also been found in stool samples and semen from infected individuals.[50][51]
The degree to which the virus is infectious during the incubation period is uncertain, but research has indicated that the pharynx reaches peak viral load approximately four days after infection[52][53] or the first week of symptoms, and declines after.[54] On 1 February 2020, the World Health Organization (WHO) indicated that "transmission from asymptomatic cases is likely not a major driver of transmission".[55] However, an epidemiological model of the beginning of the outbreak in China suggested that "pre-symptomatic shedding may be typical among documented infections" and that subclinical infections may have been the source of a majority of infections.[56] That may explain how out of 217 on board a cruise liner that docked at Montevideo, only 24 of 128 who tested positive for viral RNA showed symptoms.[57] Similarly, a study of ninety-four patients hospitalized in January and February 2020 estimated patients shed the greatest amount of virus two to three days before symptoms appear and that "a substantial proportion of transmission probably occurred before first symptoms in the index case".[58]
There is some evidence of human-to-animal transmission of SARS-CoV-2, including examples in felids.[59][60] Some institutions have advised those infected with SARS-CoV-2 to restrict contact with animals.[61][62]
Reservoir and zoonotic origin
The first known infections from the SARS-CoV-2 strain were discovered in Wuhan, China.[17] The original source of viral transmission to humans remains unclear, as does whether the strain became pathogenic before or after the spillover event.[22][63][9] Because many of the first individuals found to be infected by the virus were workers at the Huanan Seafood Market,[64][65] it has been suggested that the strain might have originated from the market.[9][66] However, other research indicates that visitors may have introduced the virus to the market, which then facilitated rapid expansion of the infections.[22][67] A phylogenetic network analysis of 160 early coronavirus genomes sampled from December 2019 to February 2020 revealed that the virus type most closely related to the bat coronavirus was most abundant in Guangdong, China, and designated type "A". The predominant type among samples from Wuhan, "B", is more distantly related to the bat coronavirus than the ancestral type "A".[68][69]
Research into the natural reservoir of the virus strain that caused the 2002–2004 SARS outbreak has resulted in the discovery of many SARS-like bat coronaviruses, most originating in the Rhinolophus genus of horseshoe bats. Phylogenetic analysis indicates that samples taken from Rhinolophus sinicus show a resemblance of 80% to SARS-CoV-2.[19][70][71] Phylogenetic analysis also indicates that a virus from Rhinolophus affinis, collected in Yunnan province and designated RaTG13, has a 96% resemblance to SARS-CoV-2.[17][72]

Bats were initially considered to be the most likely natural reservoir of SARS-CoV-2,[73][74] but differences between the bat coronavirus sampled at the time and SARS-CoV-2 suggested that humans were infected via an intermediate host. Arinjay Banerjee, a virologist at McMaster University, notes that "the SARS virus shared 99.8% of its genome with a civet coronavirus, which is why civets were considered the source."[66] Although studies had suggested some likely candidates, the number and identities of intermediate hosts remains uncertain.[75] Nearly half of the strain's genome had a phylogenetic lineage distinct from known relatives.[76]
A phylogenetics study published in 2020 indicates that pangolins are a reservoir host of SARS-CoV-2-like coronaviruses.[78] However, there is no evidence to link pangolins as an intermediate host of SARS-CoV-2 at this moment. While there is scientific consensus that bats are the ultimate source of coronaviruses, it is hypothesized that a SARS-CoV-2-like coronavirus originated in pangolins, jumped back to bats, and then jumped to humans, resulting in SARS-CoV-2. Based on whole genome sequence similarity, a pangolin coronavirus candidate strain was found to be less similar than RaTG13, but more similar than other bat coronaviruses to SARS-CoV-2.[77] Therefore, based on maximum parsimony, a specific population of bats is more likely to have directly transmitted SARS-CoV-2 to humans than a pangolin, while an evolutionary ancestor to bats was the source of general coronaviruses.[79]
A metagenomics study published in 2019 had previously revealed that SARS-CoV, the strain of the virus that causes SARS, was the most widely distributed coronavirus among a sample of Sunda pangolins.[80] On 7 February 2020, South China Agricultural University in Guangzhou announced that researchers discovered a pangolin sample with a particular coronavirus – a single nucleic acid sequence of the virus was "99% similar" to that of a protein-coding RNA of SARS-CoV-2.[81] The authors state that "the receptor-binding domain of the S protein [that binds to the cell surface receptor during infection] of the newly discovered Pangolin-CoV is virtually identical to that of 2019-nCoV, with one amino acid difference."[82]
Microbiologists and geneticists in Texas have independently found evidence of reassortment in coronaviruses suggesting involvement of pangolins in the origin of SARS-CoV-2.[83] The majority of the viral RNA is related to a variation of bat coronaviruses. The spike protein appears to be a notable exception, however, possibly acquired through a more recent recombination event with a pangolin coronavirus.[84] Structural analysis of the receptor binding domain (RBD) and human angiotensin-converting enzyme 2 (ACE2) complex[85] revealed key mutations on the RBD, such as F486 and N501, which form contacts with ACE2.[86] These residues are found in the pangolin coronavirus.[86]
Pangolins are protected under Chinese law, but their poaching and trading for use in traditional Chinese medicine remains common.[87][88] Deforestation, wildlife farming and trade in unsanitary conditions increases the risk of new zoonotic diseases, biodiversity experts have warned.[89][90][91]
It is unlikely that SARS-CoV-2 was genetically engineered. According to computational simulations on protein folding, the RBD of the spike protein of SARS-CoV-2 should have unremarkable binding affinity. In actuality, however, it has very efficient binding to the human ACE2 receptor. To expose the RBD for fusion, furin proteases must first cleave the S protein. Furin proteases are abundant in the respiratory tract and lung epithelial cells. Additionally, the backbone of the virus does not resemble any previously described in scientific literature used for genetic modification. The possibility that the virus could have gained the necessary adaptations through cell culture in a laboratory setting is challenged by scientists who assert that "the generation of the predicted O-linked glycans... suggest[s] the involvement of an immune system."[92][93]
Phylogenetics and taxonomy
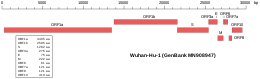 Genomic organisation of isolate Wuhan-Hu-1, the earliest sequenced sample of SARS-CoV-2 | |
| NCBI genome ID | 86693 |
|---|---|
| Genome size | 29,903 bases |
| Year of completion | 2020 |
| Genome browser (UCSC) | |
SARS-CoV-2 belongs to the broad family of viruses known as coronaviruses.[29] It is a positive-sense single-stranded RNA (+ssRNA) virus, with a single linear RNA segment. Other coronaviruses are capable of causing illnesses ranging from the common cold to more severe diseases such as Middle East respiratory syndrome (MERS, fatality rate ~34%). It is the seventh known coronavirus to infect people, after 229E, NL63, OC43, HKU1, MERS-CoV, and the original SARS-CoV.[94]
Like the SARS-related coronavirus strain implicated in the 2003 SARS outbreak, SARS-CoV-2 is a member of the subgenus Sarbecovirus (beta-CoV lineage B).[95][96] Its RNA sequence is approximately 30,000 bases in length.[14] SARS-CoV-2 is unique among known betacoronaviruses in its incorporation of a polybasic cleavage site, a characteristic known to increase pathogenicity and transmissibility in other viruses.[9][97][98]
With a sufficient number of sequenced genomes, it is possible to reconstruct a phylogenetic tree of the mutation history of a family of viruses. By 12 January 2020, five genomes of SARS-CoV-2 had been isolated from Wuhan and reported by the Chinese Center for Disease Control and Prevention (CCDC) and other institutions;[14][99] the number of genomes increased to 42 by 30 January 2020.[100] A phylogenetic analysis of those samples showed they were "highly related with at most seven mutations relative to a common ancestor", implying that the first human infection occurred in November or December 2019.[100] As of 7 May 2020, 4,690 SARS-CoV-2 genomes sampled on six continents were publicly available.[101]
On 11 February 2020, the International Committee on Taxonomy of Viruses announced that according to existing rules that compute hierarchical relationships among coronaviruses on the basis of five conserved sequences of nucleic acids, the differences between what was then called 2019-nCoV and the virus strain from the 2003 SARS outbreak were insufficient to make them separate viral species. Therefore, they identified 2019-nCoV as a strain of Severe acute respiratory syndrome-related coronavirus.
Structural biology
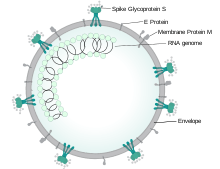
Each SARS-CoV-2 virion is 50–200 nanometres in diameter.[65] Like other coronaviruses, SARS-CoV-2 has four structural proteins, known as the S (spike), E (envelope), M (membrane), and N (nucleocapsid) proteins; the N protein holds the RNA genome, and the S, E, and M proteins together create the viral envelope.[102] The spike protein, which has been imaged at the atomic level using cryogenic electron microscopy,[103][104] is the protein responsible for allowing the virus to attach to and fuse with the membrane of a host cell;[102] specifically, its S1 subunit catalyzes attachment, the S2 subunit fusion.
Protein modeling experiments on the spike protein of the virus soon suggested that SARS-CoV-2 has sufficient affinity to the receptor angiotensin converting enzyme 2 (ACE2) on human cells to use them as a mechanism of cell entry.[106] By 22 January 2020, a group in China working with the full virus genome and a group in the United States using reverse genetics methods independently and experimentally demonstrated that ACE2 could act as the receptor for SARS-CoV-2.[17][107][25][108] Studies have shown that SARS-CoV-2 has a higher affinity to human ACE2 than the original SARS virus strain.[103][109] SARS-CoV-2 may also use basigin to assist in cell entry.[110]
Initial spike protein priming by transmembrane protease, serine 2 (TMPRSS2) is essential for entry of SARS-CoV-2.[26] After a SARS-CoV-2 virion attaches to a target cell, the cell's protease TMPRSS2 cuts open the spike protein of the virus, exposing a fusion peptide in the S2 subunit, and the host receptor ACE2. After fusion, an endosome forms around the virion, separating it from the rest of the host cell. The virion escapes when the pH of the endosome drops or when cathepsin, a host cysteine protease, cleaves it. The virion then releases RNA into the cell and forces the cell to produce and disseminate copies of the virus, which infect more cells.[111]
SARS-CoV-2 produces at least three virulence factors that promote shedding of new virions from host cells and inhibit immune response.[102] Whether they include downregulation of ACE2, as seen in similar coronaviruses, remains under investigation (as of May 2020).[78]
Epidemiology
.jpg)
Based on the low variability exhibited among known SARS-CoV-2 genomic sequences, the strain is thought to have been detected by health authorities within weeks of its emergence among the human population in late 2019.[22][112] The earliest case of infection currently known is dated back to 17 November 2019 or possibly 1 December 2019.[113] The virus subsequently spread to all provinces of China and to more than 150 other countries in Asia, Europe, North America, South America, Africa, and Oceania.[114] Human-to-human transmission of the virus has been confirmed in all these regions.[115] On 30 January 2020, SARS-CoV-2 was designated a Public Health Emergency of International Concern by the WHO,[116][12] and on 11 March 2020 the WHO declared it a pandemic.[13][117]
The basic reproduction number () of the virus has been estimated to be between 1.4 and 3.9.[118][119] This means each infection from the virus is expected to result in 1.4 to 3.9 new infections when no members of the community are immune and no preventive measures are taken. The reproduction number may be higher in densely populated conditions such as those found on cruise ships.[120] Many forms of preventive efforts may be employed in specific circumstances in order to reduce the propagation of the virus.
There have been about 82,000 confirmed cases of infection in mainland China.[114] While the proportion of infections that result in confirmed cases or progress to diagnosable disease remains unclear,[121] one mathematical model estimated that 75,815 people were infected on 25 January 2020 in Wuhan alone, at a time when the number of confirmed cases worldwide was only 2,015.[122] Before 24 February 2020, over 95% of all deaths from COVID-19 worldwide had occurred in Hubei province, where Wuhan is located.[123][124] As of 27 June 2020, the percentage had decreased to 0.65%.[114]
As of 27 June 2020, there have been 9,835,807 total confirmed cases of SARS-CoV-2 infection in the ongoing pandemic.[114] The total number of deaths attributed to the virus is 495,020.[114] Many recoveries from confirmed infections go unreported, but at least 4,972,750 people have recovered from confirmed infections.[114]
See also
- Decoding COVID-19 – 2020 PBS film documentary about the 2019-2020 COVID-19 pandemic
References
- Giaimo C (1 April 2020). "The Spiky Blob Seen Around the World". The New York Times. Archived from the original on 2 April 2020. Retrieved 6 April 2020.
- "Coronavirus disease named Covid-19". BBC News Online. 11 February 2020. Archived from the original on 15 February 2020. Retrieved 15 February 2020.
- Surveillance case definitions for human infection with novel coronavirus (nCoV): interim guidance v1, January 2020 (Report). World Health Organization. January 2020. hdl:10665/330376. WHO/2019-nCoV/Surveillance/v2020.1.
- "Healthcare Professionals: Frequently Asked Questions and Answers". United States Centers for Disease Control and Prevention (CDC). 11 February 2020. Archived from the original on 14 February 2020. Retrieved 15 February 2020.CS1 maint: unfit url (link)
- "About Novel Coronavirus (2019-nCoV)". United States Centers for Disease Control and Prevention (CDC). 11 February 2020. Archived from the original on 11 February 2020. Retrieved 25 February 2020.CS1 maint: unfit url (link)
- Harmon A (4 March 2020). "We Spoke to Six Americans with Coronavirus". The New York Times. Archived from the original on 13 March 2020. Retrieved 16 March 2020.
- Wong, G.; Bi, Y. H.; Wang, Q. H.; Chen, X. W.; Zhang, Z. G.; Yao, Y. G. (2020). "Zoonotic origins of human coronavirus 2019 (HCoV-19 / SARS-CoV-2): Why is this work important?". Zoological Research. 41 (3): 213–219. doi:10.24272/j.issn.2095-8137.2020.031. PMC 7231470. PMID 32314559.CS1 maint: display-authors (link)
- Andersen KG, Rambaut A, Lipkin WI, Holmes EC, Garry RF (17 March 2020). "Correspondence: The proximal origin of SARS-CoV-2". Nature Medicine. 26 (4): 450–452. doi:10.1038/s41591-020-0820-9. PMC 7095063. PMID 32284615.
- van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. (17 March 2020). "Correspondence: Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1". The New England Journal of Medicine. 382 (16): 1564–1567. doi:10.1056/NEJMc2004973. PMC 7121658. PMID 32182409.
- "Archived copy". Archived from the original on 17 June 2020. Retrieved 2 June 2020.CS1 maint: archived copy as title (link)
- "Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV)". World Health Organization (WHO) (Press release). 30 January 2020. Archived from the original on 31 January 2020. Retrieved 30 January 2020.
- "WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020". World Health Organization (WHO) (Press release). 11 March 2020. Archived from the original on 11 March 2020. Retrieved 12 March 2020.
- "CoV2020". GISAID EpifluDB. Archived from the original on 12 January 2020. Retrieved 12 January 2020.
- Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. (February 2020). "A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster". The Lancet. 395 (10223): 514–523. doi:10.1016/S0140-6736(20)30154-9. PMC 7159286. PMID 31986261.
- "New coronavirus stable for hours on surfaces". National Institutes of Health (NIH). NIH.gov. 17 March 2020. Archived from the original on 23 March 2020. Retrieved 4 May 2020.
- Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. (February 2020). "A pneumonia outbreak associated with a new coronavirus of probable bat origin". Nature. 579 (7798): 270–273. doi:10.1038/s41586-020-2012-7. PMC 7095418. PMID 32015507.
- Perlman S (February 2020). "Another Decade, Another Coronavirus". The New England Journal of Medicine. 382 (8): 760–762. doi:10.1056/NEJMe2001126. PMC 7121143. PMID 31978944.
- Benvenuto D, Giovanetti M, Ciccozzi A, Spoto S, Angeletti S, Ciccozzi M (April 2020). "The 2019-new coronavirus epidemic: Evidence for virus evolution". Journal of Medical Virology. 92 (4): 455–459. doi:10.1002/jmv.25688. PMC 7166400. PMID 31994738.
- Novel Coronavirus (2019-nCoV): situation report, 22 (Report). World Health Organization. 11 February 2020. hdl:10665/330991.
- Shield C (7 February 2020). "Coronavirus: From bats to pangolins, how do viruses reach us?". Deutsche Welle. Archived from the original on 4 June 2020. Retrieved 13 March 2020.
- Cohen J (January 2020). "Wuhan seafood market may not be source of novel virus spreading globally". Science. doi:10.1126/science.abb0611.
- "Q&A on coronaviruses (COVID-19)". World Health Organization (WHO). 11 February 2020. Archived from the original on 20 January 2020. Retrieved 24 February 2020.
- "How COVID-19 Spreads". U.S. Centers for Disease Control and Prevention (CDC). 27 January 2020. Archived from the original on 28 January 2020. Retrieved 29 January 2020.
- Letko M, Marzi A, Munster V (February 2020). "Functional assessment of cell entry and receptor usage for SARS-CoV-2 and other lineage B betacoronaviruses". Nature Microbiology. 5 (4): 562–569. doi:10.1038/s41564-020-0688-y. PMC 7095430. PMID 32094589.
- Hoffman M, Kliene-Weber H, Krüger N, Herrler T, Erichsen S, Schiergens TS, et al. (16 April 2020). "SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor". Cell. 181 (2): 271–280.e8. doi:10.1016/j.cell.2020.02.052. PMC 7102627. PMID 32142651.
- Wu, Katherine J. (15 April 2020). "There are more viruses than stars in the universe. Why do only some infect us? - More than a quadrillion quadrillion individual viruses exist on Earth, but most are not poised to hop into humans. Can we find the ones that are?". National Geographic Society. Archived from the original on 23 April 2020. Retrieved 18 May 2020.
- Huang P (22 January 2020). "How Does Wuhan Coronavirus Compare with MERS, SARS and the Common Cold?". NPR. Archived from the original on 2 February 2020. Retrieved 3 February 2020.
- Fox D (24 January 2020). "What you need to know about the Wuhan coronavirus". Nature. doi:10.1038/d41586-020-00209-y.
- Yam K (12 March 2020). "GOP lawmakers continue to use 'Wuhan virus' or 'Chinese coronavirus'". NBC News. Archived from the original on 14 March 2020. Retrieved 19 March 2020.
- Marquardt A, Hansler J (26 March 2020). "US push to include 'Wuhan virus' language in G7 joint statement fractures alliance". CNN. Archived from the original on 1 April 2020. Retrieved 2 April 2020.
- World Health Organization (30 January 2020). Novel Coronavirus (2019-nCoV): situation report, 10 (Report). World Health Organization. hdl:10665/330775.
- "World Health Organization Best Practices for the Naming of New Human Infectious Diseases" (PDF). WHO. May 2015. Archived (PDF) from the original on 12 February 2020.
- "Novel coronavirus named 'Covid-19': WHO". TODAYonline. Archived from the original on 21 March 2020. Retrieved 11 February 2020.
- "The coronavirus spreads racism against—and among—ethnic Chinese". The Economist. 17 February 2020. Archived from the original on 17 February 2020. Retrieved 17 February 2020.
- Hui M (18 March 2020). "Why won't the WHO call the coronavirus by its name, SARS-CoV-2?". Quartz. Archived from the original on 25 March 2020. Retrieved 26 March 2020.
- "Naming the coronavirus disease (COVID-2019) and the virus that causes it". World Health Organization. Archived from the original on 28 February 2020. Retrieved 24 February 2020.
From a risk communications perspective, using the name SARS can have unintended consequences in terms of creating unnecessary fear for some populations. ... For that reason and others, WHO has begun referring to the virus as "the virus responsible for COVID-19" or "the COVID-19 virus" when communicating with the public. Neither of these designations are [sic] intended as replacements for the official name of the virus as agreed by the ICTV.
- Gstalter, Morgan (19 March 2020). "WHO official warns against calling it 'Chinese virus', says 'there is no blame in this'". The Hill. Archived from the original on 18 April 2020. Retrieved 21 March 2020.
- Shinkman, Paul (17 March 2020). "Trump Fires Back at Complaints He's Stigmatizing China Over Coronavirus". US News. Archived from the original on 29 March 2020. Retrieved 21 March 2020.
- title "Archived copy" Check
|url=value (help). 20 June 2020. Archived from the original on 20 June 2020. Retrieved 20 June 2020. Unknown parameter|=ignored (help)CS1 maint: archived copy as title (link) - Li J, You Z, Wang Q, Zhou Z, Qiu Y, Luo R, et al. (March 2020). "The epidemic of 2019-novel-coronavirus (2019-nCoV) pneumonia and insights for emerging infectious diseases in the future". Microbes and Infection. 22 (2): 80–85. doi:10.1016/j.micinf.2020.02.002. PMC 7079563. PMID 32087334. Archived from the original on 14 April 2020. Retrieved 19 April 2020.
- Kessler, Glenn (17 April 2020). "Trump's false claim that the WHO said the coronavirus was 'not communicable'". The Washington Post. Archived from the original on 17 April 2020. Retrieved 17 April 2020.
- Kuo, Lily (21 January 2020). "China confirms human-to-human transmission of coronavirus". The Guardian. Archived from the original on 22 March 2020. Retrieved 18 April 2020.
- Edwards E (25 January 2020). "How does coronavirus spread?". NBC News. Archived from the original on 28 January 2020. Retrieved 13 March 2020.
- Anfinrud P, Stadnytskyi V, Bax CE, Bax A (May 2020). "Visualizing Speech-Generated Oral Fluid Droplets with Laser Light Scattering". The New England Journal of Medicine. 382 (21): 2061–2063. doi:10.1056/NEJMc2007800. PMC 7179962. PMID 32294341. Archived from the original on 8 June 2020. Retrieved 19 June 2020.
- Stadnytskyi V, Bax CE, Bax A, Anfinrud P (June 2020). "The airborne lifetime of small speech droplets and their potential importance in SARS-CoV-2 transmission". Proceedings of the National Academy of Sciences of the United States of America. 117 (22): 11875–11877. doi:10.1073/pnas.2006874117. PMC 7275719. PMID 32404416. Archived from the original on 17 June 2020. Retrieved 19 June 2020.
- "Getting your workplace ready for COVID-19" (PDF). World Health Organization. 27 February 2020. Archived (PDF) from the original on 2 March 2020. Retrieved 3 March 2020.
- Yong E (20 March 2020). "Why the Coronavirus Has Been So Successful". The Atlantic. Archived from the original on 20 March 2020. Retrieved 20 March 2020.
- Gibbens S (18 March 2020). "Why soap is preferable to bleach in the fight against coronavirus". National Geographic. Archived from the original on 2 April 2020. Retrieved 2 April 2020.
- Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. (March 2020). "First Case of 2019 Novel Coronavirus in the United States". The New England Journal of Medicine. 382 (10): 929–936. doi:10.1056/NEJMoa2001191. PMC 7092802. PMID 32004427.
- Li D, Jin M, Bao P, Zhao W, Zhang S (7 May 2020). "Clinical Characteristics and Results of Semen Tests Among Men With Coronavirus Disease 2019". JAMA Network Open. 3 (5): e208292. doi:10.1001/jamanetworkopen.2020.8292. PMC 7206502. PMID 32379329.
- Wölfel R, Corman VM, Guggemos W, Seilmaier M, Zange S, Müller MA, et al. (April 2020). "Virological assessment of hospitalized patients with COVID-2019". Nature. 581 (7809): 465–469. doi:10.1038/s41586-020-2196-x. PMID 32235945.
- Kupferschmidt K (February 2020). "Study claiming new coronavirus can be transmitted by people without symptoms was flawed". Science. doi:10.1126/science.abb1524.
- To KK, Tsang OT, Leung W, Tam AR, Wu T, Lung DC, et al. (March 2020). "Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study". The Lancet Infectious Diseases. 20 (5): 565–574. doi:10.1016/S1473-3099(20)30196-1. PMC 7158907. PMID 32213337. Archived from the original on 17 April 2020. Retrieved 21 April 2020.
- World Health Organization (1 February 2020). Novel Coronavirus (2019-nCoV): situation report, 12 (Report). World Health Organization. hdl:10665/330777.
- Li R, Pei S, Chen B, Song Y, Zhang T, Yang W, et al. (16 March 2020). "Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV2)". Science. 368 (6490): 489–493. doi:10.1126/science.abb3221. PMC 7164387. PMID 32179701.
- Daily Telegraph, Thursday 28 May 2020, page 2 column 1, which refers to the medical journal Thorax; Thorax May 2020 article COVID-19: in the footsteps of Ernest Shackleton Archived 30 May 2020 at the Wayback Machine
- He X, Lau EH, Wu P, Deng X, Wang J, Hao X, et al. (15 April 2020). "Temporal dynamics in viral shedding and transmissibility of COVID-19". Nature Medicine. 26 (5): 672–675. doi:10.1038/s41591-020-0869-5. PMID 32296168. Archived from the original on 19 April 2020. Retrieved 21 April 2020.
- "Questions and Answers on the COVID-19: OIE - World Organisation for Animal Health". www.oie.int. Archived from the original on 31 March 2020. Retrieved 16 April 2020.
- Goldstein J (6 April 2020). "Bronx Zoo Tiger Is Sick with the Coronavirus". The New York Times. Archived from the original on 9 April 2020. Retrieved 10 April 2020.
- "USDA Statement on the Confirmation of COVID-19 in a Tiger in New York". United States Department of Agriculture. 5 April 2020. Archived from the original on 15 April 2020. Retrieved 16 April 2020.
- "If You Have Animals—Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention (CDC). 13 April 2020. Archived from the original on 1 April 2020. Retrieved 16 April 2020.
- Eschner K (28 January 2020). "We're still not sure where the Wuhan coronavirus really came from". Popular Science. Archived from the original on 30 January 2020. Retrieved 30 January 2020.
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. (15 February 2020). "Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China". The Lancet. 395 (10223): 497–506. doi:10.1016/S0140-6736(20)30183-5. PMC 7159299. PMID 31986264. Archived from the original on 31 January 2020. Retrieved 26 March 2020.
- Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. (15 February 2020). "Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study". The Lancet. 395 (10223): 507–513. doi:10.1016/S0140-6736(20)30211-7. PMC 7135076. PMID 32007143. Archived from the original on 31 January 2020. Retrieved 9 March 2020.
- Cyranoski D (26 February 2020). "Mystery deepens over animal source of coronavirus". Nature. 579 (7797): 18–19. Bibcode:2020Natur.579...18C. doi:10.1038/d41586-020-00548-w. PMID 32127703.
- Yu WB, Tang GD, Zhang L, Corlett RT (21 February 2020). "Decoding evolution and transmissions of novel pneumonia coronavirus using the whole genomic data". ChinaXiv. doi:10.12074/202002.00033 (inactive 3 June 2020). Archived from the original on 23 February 2020. Retrieved 25 February 2020.
- Forster P, Forster L, Renfrew C, Forster M (8 April 2020). "Phylogenetic network analysis of SARS-CoV-2 genomes" (PDF). PNAS. 117 (17): 9241–9243. doi:10.1073/pnas.2004999117. PMC 7196762. PMID 32269081. Archived (PDF) from the original on 16 April 2020. Retrieved 17 April 2020.
- "COVID-19: genetic network analysis provides 'snapshot' of pandemic origins". Cambridge University. 9 April 2020. Archived from the original on 16 April 2020. Retrieved 17 April 2020.
- "Bat SARS-like coronavirus isolate bat-SL-CoVZC45, complete genome". National Center for Biotechnology Information (NCBI). 15 February 2020. Archived from the original on 4 June 2020. Retrieved 15 February 2020.
- "Bat SARS-like coronavirus isolate bat-SL-CoVZXC21, complete genome". National Center for Biotechnology Information (NCBI). 15 February 2020. Archived from the original on 4 June 2020. Retrieved 15 February 2020.
- "Bat coronavirus isolate RaTG13, complete genome". National Center for Biotechnology Information (NCBI). 10 February 2020. Archived from the original on 15 May 2020. Retrieved 5 March 2020.
- Report of the WHO-China Joint Mission on Coronavirus Disease 2019 (COVID-19) (PDF) (Report). World Health Organization (WHO). 24 February 2020. Archived (PDF) from the original on 29 February 2020. Retrieved 5 March 2020.
- Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. (February 2020). "Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding". The Lancet. 395 (10224): 565–574. doi:10.1016/S0140-6736(20)30251-8. PMC 7159086. PMID 32007145.
- Wu D, Wu T, Liu Q, Yang Z (12 March 2020). "The SARS-CoV-2 outbreak: what we know". International Journal of Infectious Diseases. 94: 44–48. doi:10.1016/j.ijid.2020.03.004. ISSN 1201-9712. PMC 7102543. PMID 32171952. Archived from the original on 9 April 2020. Retrieved 16 April 2020.
- Paraskevis D, Kostaki EG, Magiorkinis G, Panayiotakopoulos G, Sourvinos G, Tsiodras S (April 2020). "Full-genome evolutionary analysis of the novel corona virus (2019-nCoV) rejects the hypothesis of emergence as a result of a recent recombination event". Infection, Genetics and Evolution. 79: 104212. doi:10.1016/j.meegid.2020.104212. PMC 7106301. PMID 32004758. Retrieved 9 April 2020.
- Zhang T, Wu Q, Zhang Z (19 March 2020). "Probable Pangolin Origin of SARS-CoV-2 Associated with the COVID-19 Outbreak". Current Biology. 30 (7): 1346–1351.e2. doi:10.1016/j.cub.2020.03.022. PMC 7156161. PMID 32197085.
- Beeching NJ, Fletcher TE, Fowler R (22 May 2020). "BMJ Best Practice: Coronavirus Disease 2019 (COVID-19)" (PDF). BMJ. Archived (PDF) from the original on 13 June 2020. Retrieved 25 May 2020.
- Kindrachuk J, Coronavirus Frontlines (17 April 2020). "A Virologist Explains Why It Is Unlikely COVID-19 Escaped From A Lab". Forbes. Archived from the original on 21 April 2020. Retrieved 22 April 2020.
- Liu P, Chen W, Chen JP (October 2019). "Viral Metagenomics Revealed Sendai Virus and Coronavirus Infection of Malayan Pangolins (Manis javanica)". Viruses. 11 (11): 979. doi:10.3390/v11110979. PMC 6893680. PMID 31652964.
- Cyranoski D (7 February 2020). "Did pangolins spread the China coronavirus to people?". Nature. doi:10.1038/d41586-020-00364-2. S2CID 212825975. Archived from the original on 7 February 2020. Retrieved 12 February 2020.
- Xiao K, Zhai J, Feng Y (February 2020). "Isolation and Characterization of 2019-nCoV-like Coronavirus from Malayan Pangolins" (PDF). bioRxiv (preprint). doi:10.1101/2020.02.17.951335. S2CID 213920763. Archived (PDF) from the original on 22 April 2020. Retrieved 5 May 2020.
- Wong MC, Cregeen SJ, Ajami NJ, Petrosino JF (February 2020). "Evidence of recombination in coronaviruses implicating pangolin origins of nCoV-2019" (PDF). bioRxiv (preprint). doi:10.1101/2020.02.07.939207. PMC 7217297. PMID 32511310. Archived (PDF) from the original on 22 April 2020. Retrieved 5 May 2020.
- Timmer, John (1 June 2020). "SARS-CoV-2 looks like a hybrid of viruses from two different species". Ars Technica. Archived from the original on 5 June 2020. Retrieved 6 June 2020.
- Yan, Renhong; Zhang, Yuanyuan; Li, Yaning; Xia, Lu; Guo, Yingying; Zhou, Qiang (27 March 2020). "Structural basis for the recognition of SARS-CoV-2 by full-length human ACE2". Science (New York, N.Y.). 367 (6485): 1444–1448. doi:10.1126/science.abb2762. ISSN 1095-9203. PMC 7164635. PMID 32132184.
- Ho, Mitchell (30 April 2020). "Perspectives on the development of neutralizing antibodies against SARS-CoV-2". Antibody Therapeutics. 3 (2): 109–114. doi:10.1093/abt/tbaa009. S2CID 219476100. Archived from the original on 14 June 2020. Retrieved 14 June 2020.
- Kelly G (1 January 2015). "Pangolins: 13 facts about the world's most hunted animal". The Telegraph. Archived from the original on 24 December 2019. Retrieved 9 March 2020.
- Gorman J (27 February 2020). "China's Ban on Wildlife Trade a Big Step, but Has Loopholes, Conservationists Say". The New York Times. Archived from the original on 13 March 2020. Retrieved 23 March 2020.
- Carrington, Damian (27 April 2020). "Halt destruction of nature or suffer even worse pandemics, say world's top scientists". The Guardian. ISSN 0261-3077. Archived from the original on 15 May 2020. Retrieved 31 May 2020.
- Pontes, Nadia (29 April 2020). "How deforestation can lead to more infectious diseases". DW.COM. Archived from the original on 5 May 2020. Retrieved 31 May 2020.
- Cheng, Vincent C. C.; Lau, Susanna K. P.; Woo, Patrick C. Y.; Yuen, Kwok Yung (October 2007). "Severe Acute Respiratory Syndrome Coronavirus as an Agent of Emerging and Reemerging Infection". Clinical Microbiology Reviews. 20 (4): 660–694. doi:10.1128/CMR.00023-07. ISSN 0893-8512. PMC 2176051. PMID 17934078.
- "The COVID-19 coronavirus epidemic has a natural origin, scientists say—Scripps Research's analysis of public genome sequence data from SARS‑CoV‑2 and related viruses found no evidence that the virus was made in a laboratory or otherwise engineered". EurekAlert!. Scripps Research Institute. 17 March 2020. Archived from the original on 3 April 2020. Retrieved 15 April 2020.
- Andersen, Kristian G.; et al. (17 March 2020). "The proximal origin of SARS‑CoV‑2". Nature Medicine. 26 (4): 450–452. doi:10.1038/s41591-020-0820-9. PMC 7095063. PMID 32284615.
- Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. (February 2020). "A Novel Coronavirus from Patients with Pneumonia in China, 2019". The New England Journal of Medicine. 382 (8): 727–733. doi:10.1056/NEJMoa2001017. PMC 7092803. PMID 31978945.
- "Phylogeny of SARS-like betacoronaviruses". nextstrain. Archived from the original on 20 January 2020. Retrieved 18 January 2020.
- Wong AC, Li X, Lau SK, Woo PC (February 2019). "Global Epidemiology of Bat Coronaviruses". Viruses. 11 (2): 174. doi:10.3390/v11020174. PMC 6409556. PMID 30791586.
- Walls AC, Park YJ, Tortorici MA, Wall A, McGuire AT, Veesler D (9 March 2020). "Structure, function and antigenicity of the SARS-CoV-2 spike glycoprotein". Cell. 181 (2): 281–292.e6. doi:10.1016/j.cell.2020.02.058. PMC 7102599. PMID 32155444.
- "Initial genome release of novel coronavirus". Virological. 11 January 2020. Archived from the original on 12 January 2020. Retrieved 12 January 2020.
- Bedford T, Neher R, Hadfield N, Hodcroft E, Ilcisin M, Müller N. "Genomic analysis of nCoV spread: Situation report 2020-01-30". nextstrain.org. Archived from the original on 15 March 2020. Retrieved 18 March 2020.
- "Genomic epidemiology of novel coronavirus - Global subsampling". Nextstrain. Archived from the original on 20 April 2020. Retrieved 7 May 2020.
- Wu C, Liu Y, Yang Y, Zhang P, Zhong W, Wang Y, et al. (February 2020). "Analysis of therapeutic targets for SARS-CoV-2 and discovery of potential drugs by computational methods". Acta Pharmaceutica Sinica B. 10 (5): 766–788. doi:10.1016/j.apsb.2020.02.008. PMC 7102550. PMID 32292689.
- Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O, et al. (February 2020). "Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation". Science. 367 (6483): 1260–1263. Bibcode:2020Sci...367.1260W. doi:10.1126/science.abb2507. PMC 7164637. PMID 32075877.
- Mandelbaum RF (19 February 2020). "Scientists Create Atomic-Level Image of the New Coronavirus's Potential Achilles Heel". Gizmodo. Archived from the original on 8 March 2020. Retrieved 13 March 2020.
- Xu X, Chen P, Wang J, Feng J, Zhou H, Li X, et al. (March 2020). "Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission". Science China Life Sciences. 63 (3): 457–460. doi:10.1007/s11427-020-1637-5. PMC 7089049. PMID 32009228.
- Letko M, Munster V (January 2020). "Functional assessment of cell entry and receptor usage for lineage B β-coronaviruses, including 2019-nCoV" (PDF). bioRxiv (preprint). doi:10.1101/2020.01.22.915660. PMC 7217099. PMID 32511294. Archived (PDF) from the original on 22 April 2020. Retrieved 5 May 2020.
- El Sahly HM. "Genomic Characterization of the 2019 Novel Coronavirus". The New England Journal of Medicine. Archived from the original on 17 February 2020. Retrieved 9 February 2020.
- "Novel coronavirus structure reveals targets for vaccines and treatments". National Institutes of Health (NIH). 2 March 2020. Archived from the original on 1 April 2020. Retrieved 3 April 2020.
- Wang K, Chen W, Zhou YS, Lian JQ, Zhang Z, Du P, et al. (14 March 2020). "SARS-CoV-2 invades host cells via a novel route: CD147-spike protein" (PDF). bioRxiv (preprint). doi:10.1101/2020.03.14.988345. S2CID 214725955. Archived (PDF) from the original on 11 May 2020. Retrieved 5 May 2020.
- "Anatomy of a Killer: Understanding SARS-CoV-2 and the drugs that might lessen its power". The Economist. 12 March 2020. Archived from the original on 14 March 2020. Retrieved 14 March 2020.
- Oberholzer M, Febbo P (19 February 2020). "What We Know Today about Coronavirus SARS-CoV-2 and Where Do We Go from Here". Genetic Engineering and Biotechnology News. Archived from the original on 14 March 2020. Retrieved 13 March 2020.
- Ma J (13 March 2020). "Coronavirus: China's first confirmed Covid-19 case traced back to November 17". South China Morning Post. Archived from the original on 13 March 2020. Retrieved 16 March 2020.
- "COVID-19 Dashboard by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University (JHU)". ArcGIS. Johns Hopkins University. Retrieved 27 June 2020.
- Coronavirus disease 2019 (COVID-19) Situation Report – 69 (Report). World Health Organization. 29 March 2020. hdl:10665/331615.
- Wee SL, McNeil Jr. DG, Hernández JC (30 January 2020). "W.H.O. Declares Global Emergency as Wuhan Coronavirus Spreads". The New York Times. Archived from the original on 30 January 2020. Retrieved 30 January 2020.
- McKay B, Calfas J, Ansari T (11 March 2020). "Coronavirus Declared Pandemic by World Health Organization". The Wall Street Journal. Archived from the original on 11 March 2020. Retrieved 12 March 2020.
- Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. (January 2020). "Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus-Infected Pneumonia". The New England Journal of Medicine. 382 (13): 1199–1207. doi:10.1056/NEJMoa2001316. PMC 7121484. PMID 31995857.
- Riou J, Althaus CL (January 2020). "Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019-nCoV), December 2019 to January 2020". Eurosurveillance. 25 (4). doi:10.2807/1560-7917.ES.2020.25.4.2000058. PMC 7001239. PMID 32019669.
- Rocklöv J, Sjödin H, Wilder-Smith A (February 2020). "COVID-19 outbreak on the Diamond Princess cruise ship: estimating the epidemic potential and effectiveness of public health countermeasures". Journal of Travel Medicine. 27 (3). doi:10.1093/jtm/taaa030. PMC 7107563. PMID 32109273.
- Branswell H (30 January 2020). "Limited data on coronavirus may be skewing assumptions about severity". STAT. Archived from the original on 1 February 2020. Retrieved 13 March 2020.
- Wu JT, Leung K, Leung GM (February 2020). "Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study". The Lancet. 395 (10225): 689–697. doi:10.1016/S0140-6736(20)30260-9. PMC 7159271. PMID 32014114.
- Boseley S, McCurry J (30 January 2020). "Coronavirus deaths leap in China as countries struggle to evacuate citizens". The Guardian. Archived from the original on 6 February 2020. Retrieved 10 March 2020.
- Paulinus A (25 February 2020). "Coronavirus: China to repay Africa in safeguarding public health". The Sun. Archived from the original on 9 March 2020. Retrieved 10 March 2020.
- Leigh, Karen (24 March 2020). "Trump Says He'll Stop Using the Term 'Chinese Virus'". Bloomberg. Archived from the original on 1 April 2020. Retrieved 7 May 2020.
- "Donald Trump drops 'Chinese virus' terminology in White House briefing, calls for protecting Asian-Americans" Archived 21 April 2020 at the Wayback Machine, South China Morning Post, 24 March 2020
Further reading
- Bar-On YM, Flamholz A, Phillips R, Milo R (31 March 2020). "SARS-CoV-2 (COVID-19) by the numbers". eLife. 9. arXiv:2003.12886. Bibcode:2020arXiv200312886B. doi:10.7554/eLife.57309. PMC 7224694. PMID 32228860.
- Brüssow H (March 2020). "The Novel Coronavirus – A Snapshot of Current Knowledge". Microbial Biotechnology. 2020 (3): 607–612. doi:10.1111/1751-7915.13557. PMC 7111068. PMID 32144890.
- Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R (January 2020). "Features, Evaluation and Treatment Coronavirus (COVID-19)". StatPearls. PMID 32150360. Archived from the original on 6 April 2020. Retrieved 4 April 2020. Cite journal requires
|journal=(help) - Habibzadeh P, Stoneman EK (February 2020). "The Novel Coronavirus: A Bird's Eye View". The International Journal of Occupational and Environmental Medicine. 11 (2): 65–71. doi:10.15171/ijoem.2020.1921. PMC 7205509. PMID 32020915.
- Laboratory testing for coronavirus disease 2019 (COVID-19) in suspected human cases (Report). World Health Organization. 2 March 2020. hdl:10665/331329.
External links
- "Coronavirus Disease 2019 (COVID-19)". Centers for Disease Control and Prevention (CDC). 11 February 2020.
- "Coronavirus disease (COVID-19) Pandemic". World Health Organization (WHO).
- "SARS-CoV-2 (Severe acute respiratory syndrome coronavirus 2) Sequences". National Center for Biotechnology Information (NCBI).
- "COVID-19 Resource Centre". The Lancet.
- "Coronavirus (Covid-19)". The New England Journal of Medicine.
- "Covid-19: Novel Coronavirus Outbreak". Wiley.
- "SARS-CoV-2". Virus Pathogen Database and Analysis Resource.
- "SARS-CoV-2 related protein structures". Protein Data Bank.
| Classification |
|---|

.jpg)