Shortages related to the COVID-19 pandemic
Medical materials and other goods shortages caused by the COVID-19 pandemic quickly became a major issue of the pandemic. The matter of pandemic-related shortage has been studied in the past and has been documented in recent events. On the medical side, shortages of personal protective equipment such as medical masks, gloves, face shields, gear,[1] sanitising products, are also joined by potential shortage of more advanced devices such as hospital beds, ICU beds, oxygen therapy, ventilators and ECMO devices. Human resources, especially in terms of medical staff, may be drained by the overwhelming extent of the epidemic and associated workload, together with losses by contamination, isolation, sickness[1] or mortality among health care workers. Territories are differently equipped to face the pandemic. Various emergency measures have been taken to ramp up equipment levels such as purchases, while calls for donations, local 3D makers,[1] volunteer staffing, mandatory draft, or seizure of stocks and factory lines have also occurred. Bidding wars between different countries and states over these items are reported to be a major issue,[3][4] with price increases,[3] orders seized by local government, or cancelled by selling company to be redirected to higher bidder.[3][4] In some cases, medical workers have been ordered to not speak about these shortages of resources.[5]
While public health advocates and officials have encouraged to flatten the curve by social distancing, the unmitigated ICU needs would be about 50 times[6] the available ICU beds and ventilators capacity of most developed countries. Also, there is an imperious need and calls to increase healthcare capacity[7] despite shortages.
Background
Long term and structural
Following warnings and increased preparedness in the 2000s,[8] the 2009 swine flu pandemic led to rapid anti-pandemic reactions among Western countries. The H1N1/09 virus strain, with mild symptoms and low lethality, eventually led to a backlash over public sector over-reactiveness, spending, and the high cost/benefice of the 2009 flu vaccine. In the following years, national strategic stockpiles of medical equipment were not systematically renewed. In France[9], a €382 million spindings for H1N1 vacines and masks was widely criticised.[10][11] French health authorities decided in 2011 to not replete their stocks, to reduce acquisitions and storage costs, and to rely more on supplies from China and just-in-time logistics, and to distribute the responsibility to private companies on an optional basis.[10] In 2013, order to save cost, a law move PPE stockpile to every private enterprises which had to plan the security of their workers, without any verification mechanisms in place.[9] National manufacturers could not compete with Chinese manufacturers' prices on this new open market. The former strategic masks producer closed in 2018[9] while French strategic stockpile dropped in this period from one billion surgical masks and 600 million FFP2 masks in 2010 to 150 million and zero, respectively, in early 2020.[10] France has been called a case study of Juan Branco, author of a critical book on French President Emmanuel Macron's raise to power, argued that selfish quest of power and loyalty in leadership lead young and unexperimented people in charge of nation-wide health care reforms via blind accounting analysis and management.[12] France has been cited as a case study for countries now considering a U-turn over past 2 decades globalisation of health supplies to gain lower immediate costs.[9] The same approach was taken in the United States. The U.S. Strategic National Stockpile's stock of masks used against the 2009 flu pandemic was not replenished, neither by the Obama administration nor by the Trump administration.[13] American masks manufacturer Mike Bowen of Prestige Ameritech had been warning for years that the USA mask supply chain was too dependent on China.[14][15] As Juan Branco for France, Former US President Obama denounced short-term individualistic mindset as negatively affecting public decision making and preparedness.[16]
According to a report in the New York Times, Russian agents spent decades promoting debunked public health scares to increase mistrust toward the Federal government of the United States and its officials at home and abroad, but also to damage American science, a foundation of US national prosperity. These efforts have been linked to lower support for public health programs, anti-vaccines scares and illnesses spread, and weaker global pandemic preparedness prior to the 2020 pandemic.[17]
Several public (WHO, World Bank, Global Preparedness Monitoring Board)[18] and private initiatives raised awareness about pandemic threats and needs for better preparedness. Since 2015, Bill Gates has been warning about needing to prepare for a global pandemic.[19][20] International divisions and lack of suitable collaboration limited preparedness.[18] WHO's pandemic influenza preparedness project had a US$39 million two-year budget, out of WHO's 2020–2021 budget of US$4.8 billion. While WHO gives recommendations, there is no sustained mechanism to review countries' preparedness for epidemics and their rapid response abilities.[18] According to international economist Roland Rajah, while there are guidelines, local action depends on local governance.[18] Andy Xie, writing in the South China Morning Post, argued that ruling elites, obsessed with economic metrics, failed to prepare their communities against well-known pandemic risks.[21]
Tax systems in the early twenty-first century, by favouring the largest corporations with anti-competitive practices and lower investment rates into innovation and productions, favoured corporate actors and corporate profits, increasing the risk of shortages and weakening the society ability to respond to a pandemic.[22]
Early outbreaks in Hubei, Italy, and Spain showed that several wealthy countries' health care systems were overwhelmed.[23] In developing countries with weaker medical infrastructure, oxygen therapy, equipment for intensive care beds and other medical needs, shortages were expected to occur earlier.[23]
Immediate
First signs and warnings were due to an abnormal viral pneumonia of unknown cause in December 2019.[24][25] That month, Taiwan sent several of their Centers for Disease Control doctors to Wuhan to inspect the local situation.[25] Following confirmation of an emerging crisis and as soon as 31 December 2019,[26] Taiwan started to implement non-pharmaceutical measures such as travellers temperature checks, GPS tracking, connecting past-15 days travel history into its universal universal national healthcare database, closing travel lines to/from Wuhan and stockpiling personal protection equipment such as medical masks.[25] While well informed and later lauded for its extremly efficient virus containment, Taiwan could not weigh into the World Health Organization's reactions due to mainland Chinas long-standing policy of preventing Taiwan from joining the WHO and other global organisations. Germany, another role model in the crisis, also anticipated as soon as January 2020.[27] The United States federal government response, on the other hand, remained passive for 2 months, up to mid-March 2020, without initiating changes in their Strategic National Stockpile of medical supplies.[24]
In 2019, the Global Preparedness Monitoring Board reported the WHO's pandemic emergency fund was still depleted due to the 2018-19 Kivu Ebola epidemic.[18] Populism, nationalism and protectionism affects geopolitics, most notably setting the two major economies on confrontational courses, leaving a leadership vacuum on the world stage.[18]
In early 2020, accounts and medias linked to Russian secret services have actively spread misinformation about the 2020 pandemic to weaken trust into the American government.[17]
As the Wuhan outbreak spread in January 2020, China began blocking exports of N95 masks, booties, gloves and other supplies produced by factories on its territory;[28] organisations close to the Chinese government scoured foreign markets for PPE as late as February.[29][30] This created an unanticipated supply collapse for most other countries relying on it.
Overstretched health services often divert resources away from services women need, including pre- and post-natal health care and contraceptives, and exacerbate a lack of access to sexual and reproductive health services.[31][32][33]
Tests
Testing shortage is a key element preventing authorities from measuring the true extent of current epidemic spread. Germany and Korea's anticipative and aggressive testing strategies has helped to reduce the measured fatality rate.[27] Germany started to produce and stockpile COVID-19 tests as soon as January 2020.[27]
Diagnostic tests
Reagents
In Ireland and the UK, in late March and early April, reagent shortages limited the number of tests.[35] By March, insufficient amounts of reagent has become a bottleneck for mass testing in the EU and UK and the US.[37][38] This has led some authors to explore sample preparation protocols that involve heating samples at 98 °C (208 °F) for 5 minutes to release RNA genomes for further testing.[39][40]
In UK, on 1 April, the government confirmed that a total of 2,000 NHS staff had been tested for coronavirus since the outbreak began, but Cabinet Office Minister Michael Gove said a shortage of chemicals needed for the test meant it was not possible to screen the NHS's 1.2 million workforce.[41] Gove's statement was contradicted by the Chemical Industries Association, which said there was not a shortage of the relevant chemicals and that at a meeting with a business minister the week before the government had not tried to find out about potential supply problems.[42]
Swabs
A feared shortage of swabs in Iceland was averted when stocks were found to bridge the gap until more arrived from China.[43] Shortages arose in the US, though one manufacturer increased production to 1 million swabs per day.[44] Shortages also arose in the UK, but were resolved by 2 April.[45]
Personal protective equipment
Generalities
Although the vast majority of PPE is produced in China, domestic supplies were insufficient. The Chinese government took control of stocks from foreign enterprises whose factories produced these goods. Medicon, whose three factories produced such supplies in China, saw their stocks seized by the Communist Party-led government.[46] Figures from China Customs show that some 2.46 billion pieces of epidemic prevention and control materials had been imported between 24 January and 29 February, including 2.02 billion masks and 25.38 million items of protective clothing valued at 8.2 billion yuan ($1 billion).[29][30] Press reported that the China Poly Group, together with other Chinese companies and state-owned enterprises, had an important role in scouring markets abroad to procure essential medical supplies and equipment for China.[29] Risland (formerly Country Garden) sourced 82 tonnes of supplies, which were subsequently airlifted to Wuhan.[47] Greenland Holdings also sourced bulk supplies of medical consumables such as surgical masks, thermometers, antibacterial wipes, hand sanitisers, gloves and paracetomol for shipping to China. The mass procurement of supplies at wholesale and retail levels by Chinese companies to help their compatriots back home have contributed to shortages of products in western countries where these Chinese companies operate.[48][49] On 24 March the Australian Prime Minister Scott Morrison announced restrictions on such activities.[50][51]
Given that the global supply of PPE is insufficient, and following these Chinese measures, the World Health Organization (WHO) recommended in February 2020 minimising the need for PPE through telemedicine; physical barriers, such as clear windows; allowing only those involved in direct care to enter a room with a COVID-19 patient; using only the PPE necessary for the specific task; continuing use of the same respirator without removing it while caring for multiple patients with the same diagnosis; monitoring and coordinating the PPE supply chain; and discouraging the use of masks for asymptomatic individuals.[52]
Quality issues exacerbating shortages
In late-March/early-April 2020, as Western countries were in turn dependent on China for supplies of masks and other equipment, European politicians e.g. the EU chief diplomat Josep Borrell accused China of a soft-power play to influence world opinion.[53][54] Also, some of the supplies sent to Spain, Turkey, and the Netherlands were rejected as being faulty. Dutch health ministry issued a recall of 600,000 face masks from a Chinese supplier on 21 March that did not fit properly and whose filters did not work as intended despite them having a quality certificate;[53][54][54] The Spanish government discovered that 60,000 out of 340,000 test kits from a Chinese manufacturer did not accurately test for COVID-19.[54] The Chinese Ministry of Foreign Affairs responded that the customer should "double-check the instructions to make sure that you ordered, paid for and distributed the right ones. Do not use non-surgical masks for surgical purposes".[54] In mid-May, the European Commission suspended an order of 10 million Chinese masks destined for member states and the UK after two countries reported having received sub-standard products. The masks had been ordered by the EU's executive arm and was set to be distributed in six weekly instalments. After a first batch of 1.5 million masks was distributed to 17 of the 27 member states and Britain, Poland said the 600,000 items they received did not have European certificates nor did they comply with the necessary standard. Commission health spokesman Stefan De Keersmaecker vowed to investigate and take the necessary action.[55]
By April 2020, studies revealed that a significant percentage of those with coronavirus were asymptomatic, allowing the virus to spread undetected. Therefore, the CDC recommended "wearing cloth face coverings in public settings where other social distancing measures are difficult to maintain".[56]
Sanitising products
Hand sanitiser was largely out of stock in many areas,[57][58] causing price gouging.[59]
Protective gear
In the United States, shortages were such that some nurses at one New York City hospital resorted to wearing garbage bags as an alternative to unavailable protective clothing.[60] In light of the shortages of traditional protective gear, small businesses throughout the United States have been retooling to produce makeshift protective devices, often created through open source design initiatives in which manufacturers donate the gear to hospitals. An example is the COVID-19 Intubation Safety Box, first used by hospitals in Taiwan, which is an acrylic cube placed over an infected patient's torso, with openings that allow ventilator intubation and extubation while minimising contaminated droplet risk to healthcare workers.[61]
_produced_by_Ascalon_Studios%2C_Inc.jpg)
Facial masks
Early epidemic in China

.jpg)
As the epidemic accelerated, the mainland market saw a shortage of face masks due to increased public demand.[62] In Shanghai, customers had to queue for nearly an hour to buy a pack of face masks; stocks were sold out in another half an hour.[63] Hoarding and price gouging drove up prices, so the market regulator said it would crack down on such acts.[64][65] In January 2020, price controls were imposed on all face masks on Taobao and Tmall.[66] Other Chinese e-commerce platform – JD.com,[67] Suning.com,[68] Pinduoduo[69] – did likewise; third-party vendors would be subject to price caps, with violators subject to sanctions.
National stocks and shortages
In 2006, 156 million masks were added to the U.S. Strategic National Stockpile in anticipation of a flu pandemic.[13] After they were used against the 2009 flu pandemic, neither the Obama administration nor the Trump administration renewed the stocks.[13] By 1 April, U.S.'s Strategic National Stockpile was nearly emptied.[70]
In France, 2009 H1N1-related spending rose to €382 million, mainly on supplies and vaccines, which was later criticised.[10][11] It was decided in 2011 to not replete its stocks and rely more on supply from China and just-in-time logistics.[10] In 2010, its stock included 1 billion surgical masks and 600 million FFP2 masks; in early 2020 it was 150 million and zero, respectively.[10] While stocks were progressively reduced, a 2013 rational stated the aim to reduce costs of acquisition and storage, now distributing this effort to all private enterprises as an optional best practice to ensure their workers' protection.[10] This was especially relevant to FFP2 masks, more costly to acquire and store.[10][71] As the COVID-19 pandemic in France took an increasing toll on medical supplies, masks and PPE supplies ran low and caused national outrage. France needs 40 million masks per week, according to French president Emmanuel Macron.[72] France instructed its few remaining mask-producing factories to work 24/7 shifts, and to ramp up national production to 40 million masks per month.[72] French lawmakers have opened an inquiry on the past management of these strategic stocks.[73]
.png)
In the wake of the 2020 COVID-19 pandemic and widespread complaints by nurses and other health care workers about lack of N95 masks and proper protocols, National Nurses United, the largest organization of registered nurses in the United States, filed over 125 complaints with Occupational Safety and Health Administration (OSHA) offices in 16 states charging hospitals with failing to comply with laws mandating safe workplaces in which COVID-19 nurses should be provided N-95 masks.[74]
Competition for supplies
Countries such as Britain, France, Germany, South Korea, Taiwan, China, India, and others initially responded to the outbreak by limiting or banning exports of medical supplies to protect their citizens, including rescinding orders that other nations already secured.[75][76] Germany blocked exports of 240,000 masks bound for Switzerland[77][78] and also stopped similar shipments to the Central Bohemian Region as well.[79] One French company, Valmy SAS, was forced to block an order for PPE to be sent to the UK, after the company's UK representative told CNN that the order had been blocked by customs officials at the French coast. Turkey blocked a shipment of ventilators bought by two regional Spanish governments from a Turkish company, citing the risk of a shortage at home in holding onto the ventilators;[80] 116 of the ventilators were later released.[81]
As the pandemic began to worsen, governments began employing strong-arm tactics including even surreptitious means to obtain medical supplies necessary to fight the coronavirus, either through paying more cash to reroute or seizing such equipment.[80] Slovakian prime minister Peter Pellegrini said the government was preparing cash worth 1.2 million euros ($1.3 million) to purchase masks from a contracted Chinese supplier. He then said "However, a dealer from Germany came there first, paid more for the shipment, and bought it."[82][83] Ukraine lawmaker Andriy Motovylovets also stated that "Our consuls who go to factories find their colleagues from other countries (Russia, USA, France, Germany, Italy, etc) who are trying to obtain our orders. We have paid upfront by wire transfer and have signed contracts. But they have more money, in cash. We have to fight for each shipment."[82] San Marino authorities said they arranged a bank transfer to a supplier in Lugano, Switzerland, to pay for a half-million masks to be shared with Italian neighbours. However, the truck came in empty, because one or several unidentified foreign buyers offered more instead.[84]
Germany snatched 830,000 surgical masks that were arriving from China and destined for Italy. Although Italian authorities managed to persuade Germany to release them, no one in Germany, however, found the masks they seized at all.[85][86] 1.5 million face masks that were supposed to be delivered from Spain to Slovenia were seized by German agents.[87] French guards confiscated lorries filled with 130,000 face masks and boxes of sanitisers bound for the UK in what was described as a "despicable act" by the British government.[88] Italian customs police hijacked some 800,000 imported masks and disposable gloves that were about to be sent to Switzerland.[84]
On 22 March, an Italian newspaper said that the 680,000 face masks and ventilators it ordered from China were confiscated by the Czech Republic's police. They carried out an anti-trafficking operation in which they seized equipment from a warehouse of a private company in northern town of Lovosice. According to Czech authorities, the donation from China represented only just over 100,000 masks. Czech government sent 110,000 items to Italy as compensation. It's unclear how the masks ended up in Lovosice. Czech Foreign Minister Tomáš Petříček told AFP: "Lovosice is not quite en route from China to Italy."[89][90][80][82]
Valérie Pécresse, regional counselor of Île-de-France, alleged that some Americans, in their aggressive search for stocks, had made tarmac bids for stocks of masks – sight unseen – awaiting loading onto transporters, paying 3 times the price in cash.[91][4] However, Politico Europe reported the French claim as "unsubstantiated"[92] and the U.S. Embassy in Paris stated that "The United States government has not purchased any masks intended for delivery from China to France. Reports to the contrary are completely false."[80]
On 3 April, Berlin politician Andreas Geisel accused U.S. agents of appropriating a shipment of 200,000 3M-made face masks meant for Berlin police from the airport in Bangkok.[93][94] However, these claims were proven false, as 3M revealed it "has no records of an order for respiratory masks from China for the Berlin police" and Berlin police later confirmed that the shipment was not seized by U.S. authorities, but was said to have simply been bought at a better price, widely believed to be from a German dealer or China. This revelation outraged the Berlin opposition, whose CDU parliamentary group leader Burkard Dregger accused Geisel of "deliberately misleading Berliners" in order "to cover up its own inability to obtain protective equipment". FDP interior expert Marcel Luthe said "Big names in international politics like Berlin's senator Geisel are blaming others and telling US piracy to serve anti-American clichés."[95][96] Politico Europe reported that "the Berliners are taking a page straight out of the Trump playbook and not letting facts get in the way of a good story."[92] The Guardian also reported that "There is no solid proof Trump [nor any other American official] approved the [German] heist".[97]
On 3 April, Jared Moskowitz, head of Florida Division of Emergency Management, accused the American company 3M of selling N95 masks directly to foreign countries for cash instead of the United States. Moskowitz stated that 3M agreed to authorise distributors and brokers to represent they were selling the masks to Florida, but instead his team for the last several weeks "get to warehouses that are completely empty." He then said the 3M authorised U.S. distributors later told him the masks Florida contracted for never showed up because the company instead prioritised orders that come in later, for higher prices, from foreign countries (including Germany, Russia, and France). As a result, Moskowitz highlighted the issue on Twitter, saying he decided to "troll" 3M.[98][99][100] Forbes reported that "roughly 280 million masks from warehouses around the U.S. had been purchased by foreign buyers [on 30 March 2020] and were earmarked to leave the country, according to the broker – and that was in one day", causing massive critical shortages of masks in the U.S.[101][102]
On 3 April, the Swedish health care company Mölnlycke announced that France had seized millions of face masks and gloves that the company imported from China to Spain and Italy. The company's general manager, Richard Twomey, denounced France for "confiscat[ing] masks and gloves even though it was not [its] own. This is an extremely disturbing, unbecoming act." Mölnlycke estimated a total of "six million masks was seized by the French. All had been contracted for, including a million masks each for France, Italy and Spain. The rest were destined for Belgium, the Netherlands, Portugal and Switzerland, which has special trading status with the EU."[103] Sweden's foreign ministry stated to Agence France-Presse that "We expect France to promptly cease the requisition of medical equipment and do what it can to ensure that supply chains and the transportation of goods are secured. The common market has to function, particularly in times of crisis."[104][105][82]
On 24 April, San Francisco Mayor London Breed complained that her city's orders for PPE were diverted to other cities and countries. She said "We’ve had issues of our orders being relocated by our suppliers in China. For example, we had isolation gowns on their way to San Francisco and they were diverted to France. We’ve had situations when things we’ve ordered that have gone through Customs were confiscated by FEMA to be diverted to other locations."[106]
Trade in medical supplies between the United States and China has also become politically complicated. Exports of face masks and other medical equipment to China from the United States (and many other countries) spiked in February, according to statistics from Trade Data Monitor, prompting criticism from the Washington Post that the United States government failed to anticipate the domestic needs for that equipment.[107] Similarly, The Wall Street Journal, citing Trade Data Monitor to show that China is the leading source of many key medical supplies, raised concerns that US tariffs on imports from China threaten imports of medical supplies into the United States.[108]
Masks reuses
| Can facial masks be disinfected for re-use?[109] | |||||
|---|---|---|---|---|---|
| Cleaning method | Meltblown fibre filtration media | Static-charged cotton | E. coli.
Disinfection | ||
| Filtration (%) | Pressure drop (Pa) | Filtration (%) | Pressure drop (Pa) | ||
| Masks before treatment | 96.76 | 8.33 | 78.01 | 5.33 | (no E.coli) |
| 70 °C hot air in oven, 30 min. | 96.60 | 8.00 | 70.16 | 4.67 | >99% |
| Ultraviolet light, 30 min. | 95.50 | 7.00 | 77.72 | 6.00 | >99% |
| 5% alcohol soaking, drying | 56.33 | 7.67 | 29.24 | 5.33 | >99% |
| Chlorine-based, 5 min. | 73.11 | 9.00 | 57.33 | 7.00 | >99% |
| Vapor from boiling water, 10 min. | 94.74 | 8.00 | 77.65 | 7.00 | >99% |
Shortage in single-use medical mask and field reports of reuse lead to the question of which process could properly sanitise these PPE without altering their filtering capacity.[109]
FFP2 masks can be sanitised by 70 °C vapour allowing reuses.[109] Use of alcohol is discouraged since it alters N95 mask microfibres' static charge which helps filtration.[109] Chlorine is also discouraged since its fumes may be harmful.[109] Authors are warning against reuses by non-professionals, pointing out that even the best scored methods can degrade the mask if not performed properly.[109][110]
A Singaporean study found no contamination on mask after brief care to COVID19 patients, suggesting masks could be reused for multiple patients cares.[111] A portion of SARS-CoV-2 virus can survive long exposure to 60 °C.[112]
Makers have designed Arduino-controlled disinfection boxes, with temperature controls, to safely reuse surgical and N95 masks.[113]
Gas disinfection allows 10 reuse.[114]
DIY masks
Following N95 masks shortages, volunteers created 3D printed "NanoHack" alternative.[115] This printed mask allows to use hand-cut surgical mask as fine-particle filters.[115]
Given the scarcity of masks and ambiguity on their efficiency, individuals and volunteers have started to produce cloth masks for themselves or for others.[116] Various designs are shared online to ease creation.[116]
Medical face shield
Reacting to shortage of face shield, volunteers from the maker community with 3D printing abilities initiated an effort to produce face-shields for hospital staff.[115]
3D printer manufacturers
At the early stage, a few 3D printer manufacturers published their designs.
On 14 March, Budmen Industries, a custom 3D printer maker in New York, created a face shield design and produced their first 50 shields with a plan to donate to the Onondaga County to use in a COVID-19 testing site.[117] The company published their design and it had more than 3,000 downloads within a week.[118] By the end of the month, the company and its partner made 5,000 face shields with global requests for 260,000 units.[119]
On 16 March, Prusa Research, a Czech 3D printer manufacturer, started working on a face shield design for medical use . The design was approved by the Czech Ministry of Health and went to a field test and a large scale production within 3 days. The company published the design for people to make face shields to support local efforts. The design was downloaded in a large number by makers around the world.[120] By the end of March, the company employed 500 employees to work on the 10,000 shields order. Their design was downloaded 40,000 times.[121]
Local volunteers
As the shortage of personal protective equipment in New York City hospitals got into a critical stage, volunteers started making face shields using the Budmen design on 20 March. More efforts were started by various groups from hobbyists, academics, to experts.[122] Many designs had been created and groups were formed to supply face shields to local hospitals.[123]
On 24 March, while the epidemic was expanding, popular French 3D maker and YouTuber Heliox announced on 24 March that she would produce face shields for free, building upon another maker's design.[124] She was quickly contacted by local hospitals, health centres and other medical professionals asking for rapid delivery of face shields.[124] The visible popularity of her initiative caused other 3D makers to join the effort and offer their help in other regions to connect health facilities with nearby makers.[124]
On 30 March, The New York Times published a video on COVID-19-related shortages and healthcare workers' DIY solutions.[1]
Government agencies
On 23 March 2020, United States Food and Drug Administration (FDA), United States Department of Veterans Affairs (VA), and National Institutes of Health (NIH) entered into a memorandum of understanding to form a public-private partnership with America Makes, a non-profit organization, to test designs of 3D printed personal protective equipment including face shields. The agreement was to have NIH to provide the 3D Print Exchange system to solicit open designs, VA to perform testing in clinical settings, FDA to participate in the review process and America Makes to coordinate with makers to produce the approved designs for healthcare facilities.[125] As of 18 June, 13 face shields have been reviewed as appropriate for clinical use.[126]
On 9 April 2020, FDA issued an emergency use authorization that included an authorization for the use of face shields by health care personnel. FDA laid out the details of the conditions, and waiver of requirements for face shield makers in a letter on 13 April 2020.[127]
Companies
Apple Inc. announced on 5 April they would produce 1 million face shields per week to be sent to U.S. hospitals.[128] By mid April, many large companies such as Hewlett-Packard, Ford Motor Company, and Blue Origin had joined the efforts to make face shields.[129]
3D printed medical face shield created in response to COVID19's medical shortage
Medical care devices
The availability of critical care beds or ICU beds,[130] mechanical ventilation[132] and ECMO devices[133] generally closely associated with hospital beds has been described as a critical bottleneck in responding to the ongoing COVID-19 pandemic. The lack of such devices dramatically raises the mortality rate of COVID-19.
Oxygenation mask

Popular snorkelling masks have been adapted into oxygen dispensing emergency respiratory masks via the usage of 3D printed adapters and minimal modifications to the original mask.[115][134][135] According to Italian laws relative to medical cares where the project has occurs, usage by the patient requires a signed declaration of acceptance of use of an uncertified biomedical device.[135] The project provides the 3D files for free, as well as 2 forms to register hospitals in need and 3D makers willing to produces adapters.[135] In France, the main sportswear and snorkelling masks producer Decathlon has locked down its mask sales to redirect them toward medical staff, patients and 3D makers.[136] An international collaboration including Decathlon, BIC, Stanford, and other actors is on track to scale up production for international needs.[137]
Intensive care beds
Both rich countries and developing countries have or will face intensive care beds shortages, but the situation is expected to be more intense in developing countries due to lower equipment levels.[138]
In early March, the UK government supported a strategy to develop natural herd immunity, drawing sharp criticism from medical personnel and researchers.[139] Various forecasts by Imperial College COVID-19 Response Team, made public on 16 March, suggested that the peak number of cases in the UK would require between 100 and 225 CCBs / 100,000 inhabitants,[6] if proper mitigation or no mitigation strategies are put into force, respectively. These requirements would both exceed the UK's current capacities of 6.6[140]–14[6] CCB / 100,000 inhabitants. In the best case scenario, the peak caseload would require 7.5 times the current number of available ICU beds.[141] Around 16 March, the UK government changed trajectory toward a more standard mitigation/suppression strategy.[139]
In France, around 15 March, the Grand Est region was the first to express the scarcity of CCB limiting its handling of the crisis.[142] Assistance-publique Hôpitaux de Paris (AP-HP), which manages most hospitals in the French capital area (~10 million inhabitants), reported the need for 3,000–4,000 ICUs.[143] Current capacity is reported to be between 1500[143] and 350,[144] depending on the source.
In France, given shortages of ICU hospital beds in Grand Est and Ile-de-France regions, severe but stable patients with ARS and breathing assistance have been moved toward other regional medical centers within France, Germany, Austria, Luxembourg or Switzerland.[145]
Mechanical ventilation
Mechanical ventilation has been called "the device that becomes the decider between life and death"[146] for COVID-19 patients because 3.2% of detected cases need ventilation during treatment. Ventilators shortage is endemic in the developing world.[147] In case of shortage, some triage strategies have been previously discussed. One strategy is to grade the patient on dimensions such as: prospects for short-term survival; prospects for long-term survival; stage of life-related considerations; pregnancy and fair chance.[132] The frequent 15 to 20 day duration of the intubation to recover is an important factor in the ventilator's shortage.[148]
An important way of reducing demand for ventilators is the use of CPAP devices as a first resort. For this reason CPAP devices themselves have become a scarce item.
Official assessments
In the 2000s, the U.S. CDC estimated a national shortage of 40–70,000 ventilators in case of pandemic influenza.[149] From this assessment resulted Project Aura, a public-private initiative to design a frugal, $3,000 mechanical ventilator, simple to mass-produce, and able to supply the Strategic National Stockpile.[149] Newport Medical Instruments was granted the contract, designing and prototyping (2011) the frugal ventilators to CDC officials, and expecting to later profit from the product by moving into the private market where competing devices were sold for $10,000.[149] On April 2012, US Health and Human Services officials confirmed to the US Congress that the project was on schedule to file for market approval in late 2013, after which the device would go into mass-production.[149] In May 2012, US$12 billion medical conglomerate Covidien, a top actor of the mechanical ventilation market, acquired Newport for $100 million.[149] Covidien soon asked to cancel the Project Aura contract since it wasn't profitable enough.[149] Former Newport executives, government officials and executives at rival ventilator companies suspect Covidien acquired Newport to prevent the frugal $3,000 ventilator design from disturbing its profitable ventilation operation.[149] Covidien merged in 2015 into Medtronic.[149] Project Aura looked for and then signed a new contract with Philips healthcare. In July 2019, the FDA signed for 10,000 units of their Trilogy Evo portable ventilator, to be delivered to the SNS by mid-2020.[149]
On 25 March 2020, Andrew Cuomo made a detailed 1-hour COVID-19 press conference,[150][151] emphasising an expectation of a severe shortage of ventilators, and their importance in sustaining life in severe COVID-19 cases.[152] Cuomo said New York state would ultimately need about 30,000 ventilators to handle the influx, while having only 4,000 as of 25 March; on the 27th, President Trump expressed doubt about the need, saying "I don't believe you need 40,000 or 30,000 ventilators," and resisted calls to force businesses to produce them.[153][152] Later on the 27th, the President acceded to calls to assist states in ventilator procurement, using the Defense Production Act, although fears remain that procurement will not happen in time to prevent severe shortages.
Industrial suppliers
In Europe, the company Löwenstein Medical producing 1500 ICU-level ventilators and 20,000 home-level ventilator per year for France alone, pointed out of the current high demand and production shortage.[155] Based in Europe, all their components are European and not relying on the Chinese supply chain.[155] As for production ramp-up, it was suggested to increase the production of home-level ventilators, more basic and which can be assembled in half an hour, yet able to support patients through acute respiratory distress syndrome.[155] The current bottleneck is mainly a question of qualified human resources.[155] In business as usual, ICU-level ventilators are to be renewed every 10 to 15 years.[155] Due to the coronavirus pandemic, Germany and other European countries have started to take control over the company's supply.[155]
In China, local manufacturers are racing to answer the demand.[156]
Medtronic made ventilator design specifications publicly available[157] but licensing questions remain unclarified.[158]
Improvised ventilators
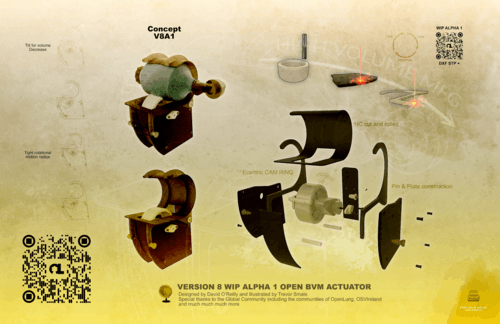
3D makers have been working on various low-cost alternative ventilation devices or adaptations.
Anaesthetist Dr. Alan Gauthier from Ontario, Canada, turned one single-patient ventilator into a nine-patient device thanks to a 2006 YouTube video by 2 doctors from Detroit.[115] The method uses T-shaped tubes to split airflow and multiply the number of patients provided with respiratory support.
In Ireland, volunteers started the Open Source Ventilator Project in collaboration with medical staff.[115]
In Italy, local journalist and journal director Nunzia Vallini of the Giornale di Brescia (Brescia Daily) was informed that nearby Chiani hospital was running out of valves which mix oxygen with air and are therefore a critical part of reanimation devices.[146] The valves supplier was itself out of stock leading to patient deaths.[146] Vallini contacted FabLab founder Massimo Temporelli, which invited Michele Faini, an expert in 3D print manufacturing and a research and development designer at Lonati SpA to join a 3D printing effort.[146] When the supplier didn't wish to share the design's specifics, they reverse-engineered the valves and produced a limited not-for-profit series for local hospitals.[146] To satisfy biomedical requirements that can withstand periodic sanitation, Lonati SpA used their SLS 3D printers to print about 100 valves in Nylon PA12.[146] Faini and Temporelli still acknowledge the limitations of their production: 3D printing not being able to reach the quality and sterilised context of the original valves and manufacturing process.[146] Contrary to rumours online, the valves don't cost US$10,000 each and the original manufacturer did not threaten to sue the 3D printers team.[146]
Hackers of the Ventilator Project have brainstormed to propose to re-purposing CPAP machines (sleep-apnea masks) as ventilators, hacking single ventilators to split air-flow and treat multiple patients, and using grounded aircraft as treatment facilities to leverage their one-oxygen-mask-per-seat infrastructure.[160] Engineers familiar with devices design and production, medical professionals familiar existing respiratory devices and lawyers able to navigate FDA regulations if the needs arise are key participants among the 350 volunteers involved.[160] The central avenue of exploration is to ditch away the most advances features of modern mechanical ventilation, which includes layers of electronics and patients monitoring systems, to focus solely on assisted respiration by pressured airflow. The group is, by example, looking for an old Harry Diamond Laboratories "emergency army respirator" model to study.[160] While hopeful they will be able to submit viable and mass-producible design, several questions linger at this later levels: mass production line, FDA approval, personnel training, personnel availability, and eventually actual needs on the battlegrounds to come.[160]
An MIT team has designed an emergency ventilator.[161]
ECMOs
Extracorporeal membrane oxygenation are devices able to replace both the lungs and the patient's heart. As of 6 February 2020, the medical community was encouraged to set up criteria for ECMO patients triage.[133]
Facilities
Hospitals
As Wuhan's situation worsened and to assist the overwhelmed Central Hospital of Wuhan and Dabie Mountain Regional Medical Centre, China built two emergency field hospitals within a few days: the Huoshenshan Hospital and Leishenshan Hospital. The hospitals were progressively phased out in March 2020.[162][163]
On 23 March, Lieutenant General Todd T. Semonite, Chief of the U.S. Army Corps of Engineers, signalled an ongoing effort to lease existing facilities such as hotels, college dormitories, and a larger hall to temporarily convert them into medical facilities.
On 16 March, French President Emmanuel Macron announced a military hospital would be set up in the Grand-Est region, to provide up to 30 ICU beds.[164] The hospital was being tested 7 days later.[165]
By 8 March, Lombardy had created 482 new ICU beds.[166] Lodi's ICU director reported that every single square metre, every single aisle of the hospital had been re-purposed for severe COVID-19 patients, increasing ICU beds from 7 to 24.[166] In Monza, 3 new wards of 50 beds each were opened on 17 March.[166] In Bergamo, gastrology, internal medicine, neurology services have been repurposed.[166]
In the UK, almost the entire private health stock of beds was requisitioned, providing an additional 8,000 beds.[167] Three Nightingale hospitals were created by NHS England, with the military, to provide an additional 10–11,000 critical care beds, another 1,000-bed hospital created in Scotland, and a 3,000-bed hospital at the Principality Stadium in Cardiff. Temporary wards were constructed in hospital car parks, and existing wards re-organised to free up 33,000 beds in England and 3,000 in Scotland for COVID-19 patients.[168] A hangar at Birmingham International Airport was converted into a 12,000 body mortuary.[168]
Morgues
New York morgue shortages led the city to propose temporary burial in parks.[169]
Health workers
There are many factors to the healthcare worker shortage. First, the excess demand due to the pandemic. Second, the specialised nature of care of the critically ill and the time taken to train for new methods of working to prevent cross-contamination, in some cases with new types of protective equipment (PPE). The third factor is the loss of staff to the pandemic, mostly because they are self-isolating with symptoms (which may be unrelated) or because a household member has symptoms, but also because of long term effects of the disease, or death. This last case applies across the health system and makes it harder to draw staff from non-COVID health workers.
Mitigations being used include recruiting military and sports medics, final-year doctors in training, private sector staff, and re-recruiting retired staff and those who have moved from the medical sector.For non-medical roles staff have been recruited from other sectors.
Patients overload
Facing the prospect of an unmanageable influx of patients both in his city and in others across the United States, New York City mayor Bill de Blasio called on the U.S. federal government to recruit additional medical staff to help meet demand. He suggested recruiting from a pool that includes retired doctors and nurses, private surgeons, and others not actively tending to COVID-19 patients, and he proposed assigning and reassigning them as needed to different parts of the country depending on which cities and states were expected to be hardest hit at any given point in time.
Isolation and trauma
As for China, medical staff are self isolating from families and under high emotional pressure.[166]
Psychological trauma is expected among medical professionals.[171]
The AMA has created a guide for healthcare organisations to reduce psychosocial trauma and increase the likelihood of medical staffs.[172]
Sickness and death
In Italy, at least 50 doctors have died from COVID-19.
In Lombardy, Italy, with the mid-March 2020 outbreak, medical staff reported high level of sick staff.[166] In Lodi, doctors from other services have been called to attend Covid patients.[166] In Cremona, the number of patients entries was three times the usual while services were running with 50% of their staff.[166] On 12 March 8% of Italy's 13,382 cases were health workers.[166] It was also reported that between 5 and 10% of deaths were medical staff.[166] On 17 March, one of the largest hospital of the Bergamo region ran out of ICU beds, patients were flown to other regions by helicopter.[166]
About 14% of Spanish cases are medical staff.[171]
USA, about 62,000 HCW have been detected as infected by late May 2020, 291 have died (0.47%).[174]
By late May, Mexico had 11,000 medical staff detected as infected, depleting medical ranks.[175]
Pharmaceutical products
- Inhaler medication[176]
Consumer goods

Some daily goods have seen shortages as a result of both disruptions to the supply chains and spikes in demand.[177][178] A surge in panic buying led to empty shelves in grocery stores. Affected products included toilet paper, hand sanitiser, cleaning supplies and canned food.[179][180]
Various consumer items were reported in local shortage due to either supply chain disruption or unusual demand, including freezers,[181] $100 bills (on one bank in New York City),[182] jigsaw puzzles,[183][184] Kettlebells,[185] blood,[186] baking yeast,[187] dogs and cats for adoption in New York City,[188] PlayStation 4,[189] Nintendo Switch and Nintendo Switch Lite,[190] laptop and tablet computers,[191] and small gold bars and gold coins.[192]
Condoms
In late March and early April, concerns about a global condom shortage arose after some factories that manufacture condoms were forced to shut down or reduce their operations, in compliance with government-imposed stay-at-home orders, including Malaysia-based Karex, the world's largest condom producer.[193] This has been compounded with delays in delivery due to greater restrictions on imports and freight, such as Egypt's 18-day quarantine on condom shipments.[194] The possibility of a condom shortage has been particularly concerning for groups focused on contraception and HIV prevention in Africa.[194]
Toilet paper and other paper products
The pandemic led to shortages of toilet paper in various countries, including Australia, Singapore, Hong Kong, Canada, the United Kingdom and the United States. In March 2020 at numerous stores throughout these countries, shoppers reported empty shelves in both the toilet paper section as well as sections for related products such as paper towels, tissues, and diapers.[180] Initially, much of this was blamed on panic buying. Consumers began fearing both supply chain disruption and the possibility of being forced into extended quarantines that would prevent them from purchasing toilet paper and related products, despite reassurance from industry and government that neither was likely to occur.[180] As a result, some consumers began hoarding toilet paper, leading to reports of empty shelves, which in turn led to additional fear of a toilet paper shortage that prompted others to hoard toilet paper as well.[180][195]
The shortage created a massive spike in Google Search, over 4000% for the term Toilet Paper alone.[196] Essential supply locator sites and tools sprouted up everywhere in an effort to assist communities in finding local sources as online retailers were out of stock.[196][197]
However, by early April 2020, additional factors other than panic buying were identified as causes of the toilet paper shortage. In particular, as a result of stay-at-home orders, people have been spending much less time at schools, workplaces, and other public venues and much more time at home, thus using public toilets less frequently and home toilets more frequently.[198] This has caused a strain on supply chains, since public toilets and home toilets generally use two different grades of toilet paper: commercial toilet paper and consumer toilet paper, respectively. Georgia-Pacific predicted a 40 percent increase in the use of consumer toilet paper as a result of people staying at home.[198] Due to differences in roll size, packaging, and supply and distribution networks between the two grades, toilet paper manufacturers are expected to have difficulty shifting production to meet the shift in demand from commercial to home use, leading to lingering shortages even after panic buying subsides.[198]
Others
In France, due to closed borders preventing foreign seasonal workers from entering the country,[199] the Minister of Agriculture called for jobless volunteers to contact strawberry farms to help collect the harvest for the usual minimal wage.[199]
Laboratory mice are being culled, and some strains are at risk of shortage due to lockdowns.[200]
In the United States, social distancing has led to shortages of blood donations.[201]
See also
- List of countries by hospital beds – Wikipedia list article
- Economic impact of the COVID-19 pandemic – Economic effects of the COVID-19 pandemic
- List of overwhelmed health care systems in the COVID-19 pandemic
References
- Tiefenthäler, Ainara. "'Health Care Kamikazes': How Spain's Workers Are Battling Coronavirus, Unprotected". The New York Times. ISSN 0362-4331. Archived from the original on 31 March 2020. Retrieved 31 March 2020.
- Cooper 360°, Anderson (2 April 2020). "New York Gov. Andrew Cuomo: "This state had purchased 17,000 ventilators, more than any other state in the nation, and they never got delivered. Because they were all coming from China, and 50 states are competing.... We can't get any more." #CNNTownHall https://cnn.it/2R42aQn pic.twitter.com/vFrbIaqMKJ". @AC360. Retrieved 3 April 2020.
- "Valérie Pécresse sur les masques: " Des Américains ont surenchéri "". 2 April 2020 – via bfmtv.com.
- "Doctors claim they have been gagged over protective equipment shortages". The Independent. 30 March 2020. Archived from the original on 31 March 2020. Retrieved 31 March 2020.
- Imperial College COVID-19 Response Team (16 March 2020). "Impact of non-pharmaceutical interventions (NPIs) to reduce COVID19 mortality and healthcare demand" (PDF). Archived (PDF) from the original on 16 March 2020. Retrieved 23 March 2020.
- Barclay, Eliza (7 April 2020). "Chart: The U.S. doesn't just need to flatten the curve. It needs to "raise the line."". Vox. Archived from the original on 7 April 2020. Retrieved 7 April 2020.
- La France et les épidémies : 2005–2007, le temps de « l’armement »
- Onishi, Norimitsu; Méheut, Constant (17 May 2020). "How France Lost the Weapons to Fight a Pandemic". The New York Times. ISSN 0362-4331. Retrieved 17 May 2020.
- "Pénurie de masques : une responsabilité partagée par les gouvernements". Public Senat (in French). 23 March 2020. Archived from the original on 9 April 2020. Retrieved 6 April 2020.
- BFMTV. "Pénurie de masques: pourquoi la France avait décidé de ne pas renouveler ses stocks il y a neuf ans" (in French). BFMTV. Archived from the original on 6 April 2020. Retrieved 6 April 2020.
- {Cite news|last=Branco|first=Juan|url=https://www.youtube.com/watch?v=RTuTluuVHjY%7Ctitle=Coronavirus, démocratie et vérité|date=3 April 2020}}
- Manjoo, Farhad (25 March 2020). "Opinion | How the World's Richest Country Ran Out of a 75-Cent Face Mask". The New York Times. ISSN 0362-4331. Archived from the original on 25 March 2020. Retrieved 25 March 2020.
- https://www.nytimes.com/2020/05/09/us/politics/whistle-blower-trump-coronavirus.html
- https://www.washingtonpost.com/investigations/in-the-early-days-of-the-pandemic-the-us-government-turned-down-an-offer-to-manufacture-millions-of-n95-masks-in-america/2020/05/09/f76a821e-908a-11ea-a9c0-73b93422d691_story.html
- Reuters (9 May 2020). "In Leaked Call, Obama Describes Trump Handling of Virus as Chaotic". The New York Times. ISSN 0362-4331. Retrieved 17 May 2020.
- Broad, William J. (13 April 2020). "Putin's Long War Against American Science". The New York Times. ISSN 0362-4331. Archived from the original on 1 May 2020. Retrieved 13 April 2020.
- "Wanted: world leaders to answer the coronavirus pandemic alarm". South China Morning Post. 31 March 2020. Archived from the original on 9 April 2020. Retrieved 6 April 2020.
- https://eu.usatoday.com/story/news/factcheck/2020/03/22/coronavirus-fact-check-did-bill-gates-predict-outbreak-2015/2890900001/
- Gates, Bill, The next outbreak? We're not ready, archived from the original on 5 April 2020, retrieved 6 April 2020
- "How the greedy elite failed us, putting profit before pandemic preparedness". South China Morning Post. 6 April 2020. Archived from the original on 9 April 2020. Retrieved 6 April 2020.
- "Biggest companies pay the least tax, leaving society more vulnerable to pandemic – new research". theconversation.com. Archived from the original on 1 April 2020. Retrieved 7 April 2020.
- Whittington, Dale; Wu, Xun (30 March 2020). "Why coronavirus lockdowns will not be easy for developing countries, and what they can learn". South China Morning Post. Archived from the original on 30 March 2020. Retrieved 6 April 2020.
- "U.S. 'wasted' months before preparing for virus pandemic". AP NEWS. 5 April 2020. Retrieved 6 April 2020.
- "How Taiwan Contained COVID-19: Early Action, Technology & Millions of Face Masks". Democracy Now!. Archived from the original on 5 April 2020. Retrieved 6 April 2020.
- "Taiwan, WHO spar again over coronavirus information sharing". Reuters. 11 April 2020. Archived from the original on 8 May 2020. Retrieved 12 April 2020.
- Katrin Bennhold (6 April 2020). "A German Exception? Why the Country's Coronavirus Death Rate Is Low". The New York Times. Retrieved 9 April 2020.
- Bowden, Ebony. "Trump administration weighs legal action over alleged Chinese hoarding of PPE". New York Post. Archived from the original on 6 April 2020. Retrieved 7 April 2020.
- Millar, Kate McClymont, Royce (2 April 2020). "Billions of face masks sent to China during bushfire crisis". The Sydney Morning Herald. Archived from the original on 3 April 2020. Retrieved 3 April 2020.
- "United Front groups in Canada helped Beijing stockpile coronavirus safety supplies – National | Globalnews.ca". Archived from the original on 30 April 2020. Retrieved 5 May 2020.
- "UN Secretary-General's policy brief: The impact of COVID-19 on women | Digital library: Publications". UN Women. Retrieved 5 June 2020.
- "Gender equality matters in COVID-19 response". UN Women. Retrieved 5 June 2020.
- "COVID-19: Emerging gender data and why it matters | UN Women Data Hub". data.unwomen.org. Retrieved 5 June 2020.
- "Ireland says reagent shortage to slow COVID-19 tests rollout for 7–10 days". Reuters. 1 April 2020. Retrieved 2 April 2020.
- Baird, Robert P. (24 March 2020). "Why Widespread Coronavirus Testing Isn't Coming Anytime Soon". The New Yorker. Archived from the original on 28 March 2020. Retrieved 29 March 2020.
South Dakota, said that her state’s public-health laboratory—the only lab doing COVID-19 testing in the state—had so much trouble securing reagents that it was forced to temporarily stop testing altogether. also noted critical shortages of extraction kits, reagents, and test kits
- Ossola, Alexandra (25 March 2020). "Here are the coronavirus testing materials that are in short supply in the U.S." Quartz. Archived from the original on 26 March 2020. Retrieved 29 March 2020.
extract the virus’s genetic material—in this case, RNA—using a set of chemicals that usually come in pre-assembled kits. “The big shortage is extraction kits” There are no easy replacements here: “These reagents that are used in extraction are fairly complex chemicals. They have to be very pure, and they have to be in pure solution”
- Fomsgaard, Anders (27 March 2020). "Statens Serum Institut (SSI) solves essential COVID-19 testing deficiency problem". en.ssi.dk. Statens Serum Institut. Archived from the original on 29 March 2020.
several countries are in lack of the chemical reagents necessary to test their citizens for the disease.
- "Danish researchers behind simple coronavirus test method". The Copenhagen Post. 28 March 2020. Archived from the original on 28 March 2020.
- "Coronavirus: Boris Johnson vows more virus tests as UK deaths exceed 2,000". BBC News. 1 April 2020. Archived from the original on 3 April 2020. Retrieved 4 April 2020.
- Preston, Robert (31 March 2020). "Robert Peston: Is Michael Gove right that there is a shortage of coronavirus test kit ingredients?". ITV News. Archived from the original on 1 April 2020. Retrieved 1 April 2020.
- "Archived copy". Archived from the original on 31 March 2020. Retrieved 3 April 2020.CS1 maint: archived copy as title (link)
- "Swab Manufacturer Works To Meet 'Overwhelming' Demand". NPR. Archived from the original on 2 April 2020. Retrieved 3 April 2020.
- "UK Has Fixed Swab Shortage Problem for Coronavirus Testing, Minister Says". U.S. News & World Report. 2 April 2020.
- "Hospitals left without masks as vital medical supplies shipped to China | 60 Minutes Australia". Retrieved 6 April 2020 – via YouTube.
- McClymont, Kate (27 March 2020). "Second developer flew 82 tonnes of medical supplies to China". The Sydney Morning Herald. Archived from the original on 27 March 2020. Retrieved 27 March 2020.
- McClymont, Kate (26 March 2020). "Chinese-backed company's mission to source Australian medical supplies". The Sydney Morning Herald. Archived from the original on 25 March 2020. Retrieved 26 March 2020.
- Lushington (28 March 2020). "China Pillages Australia's Much-Needed Medical Supplies". The BFD. Archived from the original on 6 April 2020. Retrieved 7 April 2020.
- "Coronavirus Australia: More medical supplies and groceries being shipped to China". News.com.au. 31 March 2020. Archived from the original on 31 March 2020. Retrieved 31 March 2020.
- Jenkins, Shannon (25 March 2020). "COVID-19: Morrison announces latest restrictions". The Mandarin. Archived from the original on 25 March 2020. Retrieved 25 March 2020.
- "Rational use of personal protective equipment for coronavirus disease 2019 (COVID-19)" (PDF). World Health Organization. 27 February 2020. Archived (PDF) from the original on 3 March 2020. Retrieved 21 March 2020.
- "Countries reject Chinese-made equipment". 30 March 2020. Archived from the original on 22 May 2020. Retrieved 3 April 2020 – via bbc.com.
- Choi, David (2 April 2020). "Chinese government rejects allegations that its face masks were defective, tells countries to 'double check' instructions". Business Insider France. Archived from the original on 12 April 2020. Retrieved 3 April 2020.
- "Archived copy". Archived from the original on 21 May 2020. Retrieved 17 May 2020.CS1 maint: archived copy as title (link)
- "Recommendation Regarding the Use of Cloth Face Coverings, Especially in Areas of Significant Community-Based Transmission". Centers for Disease Control and Prevention. Archived from the original on 3 April 2020. Retrieved 4 April 2020.
- "Shortage in supply can halt hand sanitizer production nationwide". West Virginia: WDTV. 5 April 2020. Archived from the original on 7 April 2020. Retrieved 7 April 2020.
- "NYC Businesses Making Sanitizer Challenged by Shortage in Shipping Supplies". New York: NY1. 4 April 2020. Archived from the original on 7 April 2020. Retrieved 7 April 2020.
- Doyne, Shannon; Gonchar, Michael (16 March 2020). "Is It Immoral to Increase the Price of Goods During a Crisis?". The New York Times. ISSN 0362-4331. Archived from the original on 26 March 2020. Retrieved 26 March 2020.
- Bowden, Ebony; Campanile, Carl; Golding, Bruce (25 March 2020). "Worker at NYC hospital where nurses wear trash bags as protection dies from coronavirus". New York Post. Archived from the original on 26 March 2020. Retrieved 26 March 2020.
- "COVID-19 survival kits, Charlotte Moss collages for charity, and more". Businessofhome.com. Archived from the original on 12 April 2020. Retrieved 11 April 2020.
- 谢斌 张纯 (21 January 2020). "一罩难求:南都民调实测走访发现,线上线下口罩基本卖脱销". 南方都市报. Retrieved 21 January 2020.
- 徐榆涵 (23 January 2020). "全球各地瘋搶口罩 專家:不必買N95". 聯合報. Archived from the original on 25 January 2020. Retrieved 25 January 2020.
- 刘灏 (21 January 2020). "广东市场监管部门:将坚决打击囤积居奇、哄抬价格等行为". 南方网. Retrieved 21 January 2020.
- "市场价格行为提醒书". n.d. Archived from the original on 27 January 2020.
- 陈泽云 (22 January 2020). "口罩买不到怎么办?这些药店平台春节期间持续供应". 金羊网. Archived from the original on 22 January 2020. Retrieved 22 January 2020.
- 新京报 (22 January 2020). "京东:禁止第三方商家口罩涨价". 新京报网. Archived from the original on 27 January 2020. Retrieved 22 January 2020.
- 新京报 (22 January 2020). "苏宁易购:口罩等健康类商品禁涨价,并开展百亿补贴". 新京报网. Archived from the original on 22 January 2020. Retrieved 22 January 2020.
- 新京报 (22 January 2020). "拼多多:对口罩等产品进行监测,恶意涨价者将下架". 新京报网. Archived from the original on 22 January 2020. Retrieved 22 January 2020.
- Miroff, Nick. "Protective gear in national stockpile is nearly depleted, DHS officials say". The Washington Post. Archived from the original on 1 April 2020. Retrieved 1 April 2020.
- Roy, Soline; Barotte, Nicolas (19 March 2020). "Quand l'État stratège a renoncé à renouveler ses stocks de masques". Le Figaro (in French). Archived from the original on 5 April 2020. Retrieved 6 April 2020.
- "France to produce 40 million face masks by end of April for domestic battle against Covid-19". Radio France Internationale. 31 March 2020. Archived from the original on 6 April 2020. Retrieved 6 April 2020.
- "Covid-19: French lawmakers to investigate where one and a half billion masks sent". Radio France Internationale. 1 April 2020. Archived from the original on 6 April 2020. Retrieved 6 April 2020.
- "National Nurses United is Stepping Up Pressure On Hospital Employers Across the United States to Provide Safer Facilities". National Nurses United. 27 March 2020. Retrieved 7 June 2020.
- Francesco Guarascio; Philip Blenkinsop (6 March 2020). "EU fails to persuade France, Germany to lift coronavirus health gear controls". Reuters. Archived from the original on 11 April 2020. Retrieved 11 April 2020.
- Rachel Zhou, Yanqiu (18 March 2020). "The Global Effort to Tackle the Coronavirus Face Mask Shortage". U.S. News & World Report. Archived from the original on 11 April 2020. Retrieved 11 April 2020.
- Dahinten, Jan; Wabl, Matthias (9 March 2020). "Germany Faces Backlash From Neighbors Over Mask Export Ban". Bloomberg. Archived from the original on 9 April 2020. Retrieved 11 April 2020.
- "Coronavirus: Germany blocks truck full of protective masks headed for Switzerland". The Local. 9 March 2020. Archived from the original on 9 April 2020. Retrieved 13 April 2020.
- Solar, Martin (13 March 2020). "A truck heading with protective equipment from Germany was confiscated at the border". Nas Region. Retrieved 13 April 2020.
- Onukwugha, Anayo (6 April 2020). "Coronavirus: US, Germany, France In War Of Masks". Leadership. Archived from the original on 9 April 2020. Retrieved 10 April 2020.
- "Spain thanks Turkey for authorizing ventilators". aa.com.tr. Archived from the original on 9 April 2020. Retrieved 20 April 2020.
- "Solidarity? When it comes to masks, it's every nation for itself". France 24. 4 April 2020. Archived from the original on 11 April 2020. Retrieved 9 April 2020.
- Zubkova, Dasha (16 March 2020). "Ukraine Was Ready To Sell Slovakia 2 Million Medical Face Masks, But Order Was Cut Off – Prime Minister Of Slovakia Pellegrini". Ukrainian News.
- "Scramble for Virus Supplies Strains Global Solidarity". The New York Times. 4 April 2020. Retrieved 14 April 2020.
- "800 thousand masks ordered by Gordona blocked in Germany". La Provincia Di Sondrio. 12 March 2020. Archived from the original on 21 May 2020. Retrieved 10 April 2020.
- Paudice, Claudio (14 March 2020). "Lombardia al punto di non-ritorno". HuffPost.
- Barbara Zimic; Barbara Eržen (19 March 2020). "Matej Tonin: It was a mask fraud, the state has not paid anything yet". DEVI Domov.
- Winterburn, Tony (21 March 2020). "FRENCH POLICE IN BID TO CONFISCATE 130,000 FACE MASKS BOUND FOR UK NHS DOCTORS AND NURSES BATTLING THE CORONAVIRUS". Euro Weekly News. Retrieved 13 April 2020.
- Steinbuch, Yaron (22 March 2020). "Czechs send Italy replacement masks after seizing thousands sent from China". New York Post. Archived from the original on 16 April 2020. Retrieved 9 April 2020.
- "Coronavirus: confusion as Chinese face masks bound for Italy end up in Czech Republic". South China Morning Post. 22 March 2020. Archived from the original on 8 April 2020. Retrieved 9 April 2020.
- "French politicians accuse US of buying up Chinese face masks bound for France". France 24. Archived from the original on 14 April 2020. Retrieved 27 April 2020.
- "Berlin lets mask slip on feelings for Trump's America". Politico Europe. 10 April 2020. Archived from the original on 10 April 2020. Retrieved 15 April 2020.
- "Berlin accuses US of 'piracy' over face masks". Politico. 3 April 2020. Archived from the original on 10 April 2020. Retrieved 29 April 2020.
- "US accused of 'modern piracy' after diversion of masks meant for Europe". 3 April 2020. Archived from the original on 3 April 2020.
- Fröhlich, Alexander (4 April 2020). "200,000 respirators not confiscated: Delivery for Berlin police was bought in Thailand at a better price". Der Tagesspiegel.
- Senat will Rätsel um verschwundene Maksen klären Archived 12 April 2020 at the Wayback Machine, rbb24, 4 April 2020
- Tisdall, Simon (12 April 2020). "US's global reputation hits rock-bottom over Trump's coronavirus response". The Guardian. Archived from the original on 22 April 2020. Retrieved 29 April 2020.
- Halon, Yael (3 April 2020). "Florida emergency management official says 3M selling masks to foreign countries: 'We're chasing ghosts'". Fox News Channel. Archived from the original on 4 April 2020. Retrieved 4 April 2020.
- "Interview With Jared Moskowitz, Director of Florida's Division of Emergency Management". WFOR-TV. 3 April 2020. Archived from the original on 6 April 2020. Retrieved 4 April 2020.
- Man, Anthony (5 April 2020). "Florida emergency management chief says state will have enough ICU beds and ventilators". Sun-Sentinel. Archived from the original on 6 April 2020. Retrieved 5 April 2020.
- DiSalvo, David (30 March 2020). "I Spent A Day in the Coronavirus-Driven Feeding Frenzy Of N95 Mask Sellers And Buyers And This Is What I Learned". Forbes. Archived from the original on 2 April 2020. Retrieved 8 April 2020.
- Natasha Bertrand; Gabby Orr; Daneil Lippman; Nahal Toosi (31 March 2020). "Pence task force freezes coronavirus aid amid backlash". Politico. Retrieved 8 April 2020.
- Marlowe, Lara (30 March 2020). "Coronavirus: European solidarity sidelined as French interests take priority". The Irish Times. Retrieved 10 April 2020.
- "France seizes millions of masks, gloves intended for Spain and Italy". Official Journal of the European Union. 3 April 2020. Retrieved 9 April 2020.
- "France seized masks produced for Italy and Spain". Newsmaker. 3 April 2020. Archived from the original on 9 May 2020. Retrieved 9 April 2020.
- Tal Axelrod (24 April 2020). "San Francisco mayor says city's PPE orders have been diverted, confiscated: It 'blows my mind'". The Hill. Retrieved 26 April 2020.
- Eilperin, Juliet; Stein, Jeff; Butler, Desmond; Hamburger, Tom (18 April 2020). "U.S. sent millions of face masks to China early this year, ignoring pandemic warning signs". Washington Post. Retrieved 24 June 2020.
- Ferek, Katy Stech; Zumbrun, Josh (12 April 2020). "U.S. Tariffs Hamper Imports of Sanitizer, Disinfectants, Some Companies Say". The Wall Street Journal. Retrieved 24 June 2020.
- Price, Amy; Chu, Larry (22 March 2020). "Addressing COVID-19 Face Mask Shortages [v1.1] : Can Facial Masks be Disinfected for Re-use?". stanfordmedicine.app.box.com. Stanford University Anesthesia Informatics and Media Lab, COVID-19 Evidence Service Report. p. 5. Archived from the original on 23 March 2020. Retrieved 25 March 2020.
- "Covid-19: des chercheurs tentent de décontaminer les masques – Sciences et Avenir". sciencesetavenir.fr (in French). 27 March 2020. Archived from the original on 28 March 2020. Retrieved 28 March 2020.
- Institution login (26 March 2020). "Absence of contamination of personal protective equipment (PPE) by Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) | Infection Control & Hospital Epidemiology | Cambridge Core". Infection Control & Hospital Epidemiology. Cambridge.org. 41 (5): 614–616. doi:10.1017/ice.2020.91. PMC 7156567. PMID 32213231.
- "Coronavirus can survive long exposure to high temperature, a threat to lab staff around world: paper". South China Morning Post. 14 April 2020. Archived from the original on 22 April 2020. Retrieved 22 April 2020.
- "Face-Masks Disinfection Device – needlab". Hackster.io. Retrieved 13 April 2020.
- James Gorman (11 April 2020). "Disposable N95 Masks Can Be Decontaminated, Researchers Confirm". The New York Times. Archived from the original on 21 April 2020. Retrieved 22 April 2020.
- Opoczynski, David (23 March 2020). "Coronavirus : quand les inventeurs viennent à la rescousse des hôpitaux". Le Parisien (in French). Archived from the original on 24 March 2020. Retrieved 24 March 2020.
- Sindya, Bhanoo (1 April 2020). "Which DIY mask pattern should you use? Even experts can't pick one to recommend". The Washington Post. Archived from the original on 1 April 2020.
- Moriarty, Rick (17 March 2020). "CNY couple, using 3D printers, makes 100s of face shields for coronavirus testing clinic". Retrieved 18 June 2020.
- "Coronavirus: Thousands worldwide get Liverpool couple's template to make face shields with 3D printers". 23 March 2020. Retrieved 18 June 2020.
- Galuppo, Mia (1 April 2020). "How One Hollywood Company Pivoted From Making a Movie to Making Face Masks". Hollywood Reporter. Retrieved 18 June 2020.
- Goehrke, Sarah (28 March 2020). "Making Made Right: This Czech Company Guides Global 3-D Printing Pandemic Response". Forbes. Retrieved 18 June 2020.
- Gershgorn, Dave (25 March 2020). "People Around the World Are 3D-Printing Face Shields to Battle the Coronavirus". OneZero. Retrieved 18 June 2020.
- Statt, Nick (25 March 2020). "3D Printers Are On the Front Lines of the COVID-19 Pandemic". The Verge. Retrieved 18 June 2020.
- "Plan C: Crisis Mode for COVID-19". Make: Magazine. 30 March 2020. Retrieved 18 June 2020.
- "L'imprimante 3D au secours des hôpitaux pour lutter contre le coronavirus". LCI (in French). Archived from the original on 29 March 2020. Retrieved 29 March 2020.
- Vincent, Brandi (31 March 2020). "FDA, NIH, VA Partner to Accelerate 3D-Printed Protective Gear for COVID-19 Response". Retrieved 18 June 2020.
- "COVID-19 Supply Chain Response". NIH Print Exchange. NIH. Retrieved 18 June 2020.
- . FDA https://www.fda.gov/media/136842/download. Retrieved 18 June 2020. Missing or empty
|title=(help) - DeRuy, Emily (6 April 2020). "Coronavirus: Apple to make millions of face shields for hospitals desperate for gear". The Mercury News. Retrieved 8 April 2020.
- Hartmans, Avery (14 April 2020). "Tech companies like Apple and Blue Origin and universities like Duke are using their arsenals of 3D printers to produce millions of face shields for medical workers". Business Insider. Retrieved 18 June 2020.
- Srivastava, Ranjana (16 March 2020). "Now more than ever, we have to be honest about intensive care beds". The Guardian. ISSN 0261-3077. Archived from the original on 23 March 2020. Retrieved 17 March 2020.
- Daugherty Biddison, E. Lee; Faden, Ruth; Gwon, Howard S.; Mareiniss, Darren P.; Regenberg, Alan C.; Schoch-Spana, Monica; Schwartz, Jack; Toner, Eric S. (1 April 2019). "Too Many Patients…A Framework to Guide Statewide Allocation of Scarce Mechanical Ventilation During Disasters". Chest. 155 (4): 848–854. doi:10.1016/j.chest.2018.09.025. ISSN 0012-3692. PMID 30316913.
- Ronco, Claudio; Navalesi, Paolo; Vincent, Jean Louis (1 March 2020). "Coronavirus epidemic: preparing for extracorporeal organ support in intensive care". The Lancet Respiratory Medicine. 8 (3): 240–241. doi:10.1016/S2213-2600(20)30060-6. ISSN 2213-2600. PMC 7154507. PMID 32035509.
- "Video: Emergency mask for hospital ventilators". n.d. Archived from the original on 25 March 2020.
- Isinnova (n.d.). "Easy – Covid19 : Emergency mask for hospital ventilators". Isinnova (in Italian). Archived from the original on 24 March 2020. Retrieved 24 March 2020.
- "Pourquoi ne pas distribuer des masques de plongée Décathlon? BFMTV répond à vos questions" (in French). n.d. Retrieved 1 April 2020 – via YouTube.
- "Le masque de plongée, second souffle des hôpitaux". Le Monde. 11 April 2020.
- "Why coronavirus lockdowns will not be easy for developing countries, and what they can learn". South China Morning Post. n.d. Archived from the original on 30 March 2020. Retrieved 30 March 2020.
- Stieb, Matt (16 March 2020). "U.K. Only Grasped in the 'Last Few Days' It Had the Exact Wrong Coronavirus Plan". Intelligencer. Archived from the original on 17 March 2020. Retrieved 17 March 2020.
- Rhodes, A.; Ferdinande, P.; Flaatten, H.; Guidet, B.; Metnitz, P. G.; Moreno, R. P. (1 October 2012). "The variability of critical care bed numbers in Europe". Intensive Care Medicine. 38 (10): 1647–1653. doi:10.1007/s00134-012-2627-8. ISSN 1432-1238. PMID 22777516.
- Batchelor, George (15 March 2020). "Hospitals could need 7.5 times the number of critical care beds to treat virus patients". The Telegraph. ISSN 0307-1235. Archived from the original on 23 March 2020. Retrieved 17 March 2020.
- "Coronavirus : dans le Grand Est, "pratiquement tous les lits de réanimation sont occupés"". Europe 1. Archived from the original on 17 March 2020. Retrieved 23 March 2020.
- "Covid-19 : l'AP-HP s'attend à faire face à une vague d'hospitalisation bien plus haute que prévu". Le Monde (in French). 17 March 2020. Archived from the original on 23 March 2020. Retrieved 17 March 2020.
- See Assistance Publique – Hôpitaux de Paris.
- "Les transferts de malades du coronavirus se poursuivent pour désengorger les régions saturées" – via bfmtv.com.
- Toussaint, Kristin (16 March 2020). "These Good Samaritans with a 3D printer are saving lives by making new respirator valves for free". Fast Company. Archived from the original on 26 March 2020. Retrieved 24 March 2020.
- Krishnamoorthy, Vijay; Vavilala, Monica S.; Mock, Charles N. (2014). "The need for ventilators in the developing world: An opportunity to improve care and save lives". Journal of Global Health. 4 (1): 010303. doi:10.7189/jogh.04.010303. ISSN 2047-2978. PMC 4073242. PMID 24976958.
- Rosenbaum, Lisa (18 March 2020). "Facing Covid-19 in Italy – Ethics, Logistics, and Therapeutics on the Epidemic's Front Line". New England Journal of Medicine. 0 (20): 1873–1875. doi:10.1056/NEJMp2005492. PMID 32187459.
- Kulish, Nicholas; Kliff, Sarah; Silver-Greenberg, Jessica (29 March 2020). "The U.S. Tried to Build a New Fleet of Ventilators. The Mission Failed". The New York Times. ISSN 0362-4331. Archived from the original on 29 March 2020. Retrieved 29 March 2020.
- Inc, Twitter. "Andrew Cuomo @NYGovCuomo". Periscope. Archived from the original on 27 March 2020. Retrieved 26 March 2020.
- "New York Gov. Cuomo holds briefing on the coronavirus pandemic". CNBC. 25 March 2020. Archived from the original on 31 March 2020.
- "Video, Audio, Photos & Rush Transcript: Amid Ongoing COVID-19 Pandemic, Governor Cuomo Announces 40,000 Health Professionals Have Signed Up to Volunteer as Part of The State's Surge Healthcare Force". Governor Andrew M. Cuomo. 25 March 2020. Archived from the original on 27 March 2020. Retrieved 27 March 2020.
- Evelyn, Kenya (27 March 2020). "Trump on urgent requests for ventilators: 'I don't believe you need 30,000'". The Guardian. ISSN 0261-3077. Archived from the original on 28 March 2020. Retrieved 28 March 2020.
- "Coronavirus : la demande en ventilateurs et respirateurs artificiels est devenue "colossale", explique un spécialiste dans le matériel médical". Franceinfo (in French). 17 March 2020. Archived from the original on 19 March 2020. Retrieved 23 March 2020.
- "China's factories work 24/7 to build ventilators for Milan, New York". South China Morning Post. 24 March 2020. Archived from the original on 25 March 2020. Retrieved 25 March 2020.
- "Medtronic is sharing its portable ventilator design specifications and code for free to all". TechCrunch. Archived from the original on 1 April 2020. Retrieved 2 April 2020.
- "A medical giant is sharing its ventilator designs. Will that change anything?". Fortune. Archived from the original on 7 April 2020. Retrieved 8 April 2020.
- "Open Source Ventilator / OpenLung BVM Ventilator". GitLab. Archived from the original on 27 March 2020. Retrieved 28 March 2020.
- Foggatt, Tyler. "The MacGyvers Taking on the Ventilator Shortage". The New Yorker. Archived from the original on 27 March 2020. Retrieved 27 March 2020.
- "MIT-based team works on rapid deployment of open-source, low-cost ventilator". MIT News. Archived from the original on 28 March 2020. Retrieved 28 March 2020.
- "Wuhan closes makeshift hospital as new COVID-19 cases in China drop sharply". CNA. 2 March 2020. Retrieved 3 March 2020.
- "China closes makeshift hospitals as COVID-19 cases plunge". CNA. Archived from the original on 27 March 2020. Retrieved 27 March 2020.
- "Aide de l'armée : la France dans les bras de "Morphée"" [Aid from the Army: France in the arms of "Morpheus"]. Libération (in French). 17 March 2020. Archived from the original on 24 March 2020. Retrieved 24 March 2020.
- Sébastien, Bozon (23 March 2020). "Coronavirus : voici à quoi ressemble l'hôpital militaire installé à Mulhouse" [Coronavirus: this is what the military hospital in Mulhouse looks like]. Le Monde (in French). Archived from the original on 23 March 2020. Retrieved 24 March 2020.
- Marcolini, Barbara; Stein, Robin (23 March 2020). "'Brace Yourself': How Doctors in Italy Responded to Coronavirus". The New York Times. ISSN 0362-4331. Archived from the original on 26 March 2020. Retrieved 26 March 2020.
- Illman, James. "NHS block books almost all private hospital sector capacity to fight covid-19". Health Service Journal. Retrieved 2 April 2020.
- "Take a look inside NHS Nightingale, London's new coronavirus hospital". World Economic Forum. Archived from the original on 3 April 2020. Retrieved 2 April 2020.
- Feuer, Alan; Stack, Liam (6 April 2020). "New York City Considers Temporary Graves for Virus Victims". The New York Times.
- Jennifer Senior (n.d.). "Opinion | Doctors Must Ration Ventilators as Coronavirus Rages. The Decisions Are Painful". The New York Times. Archived from the original on 30 March 2020. Retrieved 30 March 2020.
- https://www.ama-assn.org/delivering-care/public-health/caring-our-caregivers-during-covid-19
- "More than 62,000 doctors, nurses and other health care workers have had COVID-19". NBC News. Archived from the original on 28 May 2020. Retrieved 28 May 2020.
- Kitroeff, Natalie; Villegas, Paulina (28 May 2020). "'It's Not The Virus': Mexico's Broken Hospitals Become Killers, Too". The New York Times. ISSN 0362-4331. Archived from the original on 28 May 2020. Retrieved 28 May 2020.
- "Critical inhaler medication shortage looms as coronavirus cases soar". ABC News. Archived from the original on 13 April 2020. Retrieved 13 April 2020.
- "Can't find what you want in the grocery store? Here's why". CNN. 2 April 2020. Archived from the original on 7 April 2020. Retrieved 7 April 2020.
- "Empty Grocery Shelves Are Alarming, But They're Not Permanent". NPR. 18 March 2020. Archived from the original on 7 April 2020. Retrieved 7 April 2020.
- "Grocery Stores Start To Cut Hours As Coronavirus Prompts Surge in Panic-Buying". NPR. 14 March 2020. Archived from the original on 8 April 2020. Retrieved 8 April 2020.
- Lee, Bruce Y. (6 March 2020). "Is COVID-19 Coronavirus Leading To Toilet Paper Shortages? Here Is The Situation". Forbes. Retrieved 13 April 2020.
- "Consumer watch: Food hoarders lead to freezer shortage in America". KOAA. 10 April 2020. Retrieved 13 April 2020.
- Cowley, Stacy; Das, Anupreeta (14 March 2020). "A Bank in Midtown Is Cleaned Out of $100 Bills". The New York Times. ISSN 0362-4331. Retrieved 13 April 2020.
- "With People Stuck at Home, Jigsaw Puzzle Sales Soar". NPR. Retrieved 14 April 2020.
- Brisson, Kiernan. "National shortage of puzzles amid coronavirus". wcax.com. Retrieved 13 April 2020.
- Shultz, Alex. "The Truth Behind the Great Kettlebell Shortage of 2020". GQ. Retrieved 13 April 2020.
- "Social Distancing Leads To Blood Shortage". NPR. 17 March 2020. Retrieved 22 April 2020.
- Purdy, Chase. "Food companies are working to get yeast back on store shelves". Quartz. Archived from the original on 4 April 2020. Retrieved 13 April 2020.
- "Newest shortage in New York: The city is running out of dogs to adopt". Crain's New York Business. 25 March 2020. Archived from the original on 1 April 2020. Retrieved 13 April 2020.
- Cook, James (30 March 2020). "From PlayStations to laptops, the consumer gadgets facing shortages". The Telegraph. ISSN 0307-1235. Retrieved 13 April 2020.
- Business, Shannon Liao, CNN. "Nintendo pauses Nintendo Switch shipments to Japan amid global shortage". CNN. Archived from the original on 13 April 2020. Retrieved 13 April 2020.
- "COVID-19 crisis creates shortage of some electronics". wnep.com. Retrieved 13 April 2020.
- "Bloomberg Are you a robot?". Bloomberg L.P. Retrieved 13 April 2020.
- "Global condom shortage looms as coronavirus shuts down production". The Guardian. 27 March 2020. Archived from the original on 8 April 2020.
- Naftulin, Julia (27 March 2020). "There may be a worldwide condom shortage as factories are forced to shut down during the coronavirus pandemic". Business Insider. Retrieved 12 April 2020.
- Porterfield, Carlie (6 March 2020). "Here's Why The Toilet Paper Shortage Is Only Temporary". Forbes. Retrieved 13 April 2020.
- "Google Trends Toilet Paper 2020 Search Term". Google. 26 May 2020. Retrieved 26 May 2020.
- "Toilet Paper Locator". Killcoronavirus.org. 26 May 2020. Retrieved 26 May 2020.
- Nguyen, Terry (3 April 2020). "The toilet paper shortage is more complicated than you think". Vox. Retrieved 13 April 2020.
- BFMTV. "Coronavirus: la cueillette des fraises menacée par le manque de main d'oeuvre et de débouchés" (in French). BFMTV. Archived from the original on 26 March 2020. Retrieved 26 March 2020.
- Grimm, David (23 March 2020). "'It's heartbreaking.' Labs are euthanizing thousands of mice in response to coronavirus pandemic". Science | AAAS. Archived from the original on 28 March 2020. Retrieved 27 March 2020.
- "Social Distancing Leads To Blood Shortage". NPR.



