Mortality due to COVID-19
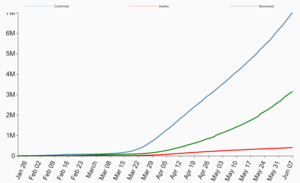
Coronavirus disease 2019 (COVID-19) has a relatively low case fatality rate, but the actual numbers of deaths are considerable given the huge scale of the pandemic.[2] As of 28 June 2020, worldwide over 503,000 people have died due to COVID-19, while more than 5.5 million people have recovered.[3] Deaths are ten times more common in those aged over 60 years and those with co-morbidities. Most people affected with the disease recover without any particular treatment. Poor outcomes and mortality are associated with old age, profound disabilities and frailty.[2]
| Part of a series on the |
| COVID-19 pandemic |
|---|
 |
|
|
|
International response |
|
Medical response |
|
|
|
History
The first confirmed death was in Wuhan on 9 January 2020.[4] The first death outside mainland China occurred in February in the Philippines,[5] and the first death outside Asia was in France on 14 February.[4] By 28 February, outside mainland China, more than a dozen deaths each were recorded in Iran, South Korea, and Italy. By end of March, nearly 100 countries reported deaths due to COVID-19.[6]
Epidemiology
As of April 2020, global death-to-case ratio, the number of deaths attributed to the disease divided by the number of diagnosed cases within the same time frame, is 7% for COVID-19.[7] A large number of cases are undiagnosed, so the actual fatality rate of the disease is likely to be lower than the present death-to-case ratio. In comparison, the case fatality rate for swine flu was between 0.1 and 5.1% ten weeks after the first international alert.[8] The death-to-case ratio is different for different regions.[9] As of June 2020, scientific studies indicate an infection fatality rate (IFR) between 0.5% and 0.9% (in countries where the average age and/or obesity rates are high).[10][11]
Mortality by age
The mortality due to COVID-19 increases with age. The overall death rate from COVID-19 in the UK is 0.0016% in children, while it is 7.8% for those aged over 80.[12]. The majority of victims had serious pre-existing health conditions.
| Age | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Country | 0–9 | 10–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80–89 | 90+ |
| Argentina as of 7 May[13] | 0.0 | 0.0 | 0.1 | 0.4 | 1.3 | 3.6 | 12.9 | 18.8 | 28.4 | |
| Australia as of 4 June[14] | 0.0 | 0.0 | 0.0 | 0.0 | 0.1 | 0.2 | 1.1 | 4.1 | 18.1 | 40.8 |
| Canada as of 3 June[15] | 0.0 | 0.1 | 0.7 | 11.2 | 30.7 | |||||
| Alberta as of 3 June[16] | 0.0 | 0.0 | 0.1 | 0.1 | 0.1 | 0.2 | 1.9 | 11.9 | 30.8 | |
| Br. Columbia as of 2 June[17] | 0.0 | 0.0 | 0.0 | 0.0 | 0.5 | 0.8 | 4.6 | 12.3 | 33.8 | 33.6 |
| Ontario as of 3 June[18] | 0.0 | 0.0 | 0.1 | 0.2 | 0.5 | 1.5 | 5.6 | 17.7 | 26.0 | 33.3 |
| Quebec as of 2 June[19] | 0.0 | 0.1 | 0.1 | 0.2 | 1.1 | 6.1 | 21.4 | 30.4 | 36.1 | |
| Chile as of 31 May[20][21] | 0.1 | 0.3 | 0.7 | 2.3 | 7.7 | 15.6 | ||||
| China as of 11 February[22] | 0.0 | 0.2 | 0.2 | 0.2 | 0.4 | 1.3 | 3.6 | 8.0 | 14.8 | |
| Colombia as of 3 June[23] | 0.3 | 0.0 | 0.2 | 0.5 | 1.6 | 3.4 | 9.4 | 18.1 | 25.6 | 35.1 |
| Denmark as of 4 June[24] | 0.2 | 4.1 | 16.5 | 28.1 | 48.2 | |||||
| Finland as of 4 June[25] | 0.0 | 0.0 | <0.4 | <0.4 | <0.5 | 0.8 | 3.8 | 18.1 | 42.3 | |
| Germany as of 5 June[26] | 0.0 | 0.0 | 0.1 | 1.9 | 19.7 | 31.0 | ||||
| Bavaria as of 5 June[27] | 0.0 | 0.0 | 0.1 | 0.1 | 0.2 | 0.9 | 5.4 | 15.8 | 28.0 | 35.8 |
| Israel as of 3 May[28] | 0.0 | 0.0 | 0.0 | 0.9 | 0.9 | 3.1 | 9.7 | 22.9 | 30.8 | 31.3 |
| Italy as of 3 June[29] | 0.3 | 0.0 | 0.1 | 0.3 | 0.9 | 2.7 | 10.6 | 25.9 | 32.4 | 29.9 |
| Japan as of 7 May[30] | 0.0 | 0.0 | 0.0 | 0.1 | 0.3 | 0.6 | 2.5 | 6.8 | 14.8 | |
| Mexico as of 3 June[31] | 3.3 | 0.6 | 1.2 | 2.9 | 7.5 | 15.0 | 25.3 | 33.7 | 40.3 | 40.6 |
| Netherlands as of 3 June[32] | 0.0 | 0.2 | 0.1 | 0.3 | 0.5 | 1.7 | 8.1 | 25.6 | 33.3 | 34.5 |
| Norway as of 4 June[33] | 0.0 | 0.0 | 0.0 | 0.0 | 0.3 | 0.4 | 2.2 | 9.0 | 22.7 | 57.0 |
| Philippines as of 4 June[34] | 1.6 | 0.9 | 0.5 | 0.8 | 2.4 | 5.5 | 13.2 | 20.9 | 31.5 | |
| Portugal as of 3 June[35] | 0.0 | 0.0 | 0.0 | 0.0 | 0.3 | 1.3 | 3.6 | 10.5 | 21.2 | |
| South Africa as of 28 May[36] | 0.3 | 0.1 | 0.1 | 0.4 | 1.1 | 3.8 | 9.2 | 15.0 | 12.3 | |
| South Korea as of 15 June[37] | 0.0 | 0.0 | 0.0 | 0.2 | 0.2 | 0.7 | 2.6 | 10.1 | 25.6 | |
| Spain as of 17 May[38] | 0.2 | 0.3 | 0.2 | 0.3 | 0.6 | 1.4 | 4.9 | 14.3 | 21.0 | 22.3 |
| Sweden as of 5 June[39] | 0.5 | 0.0 | 0.2 | 0.2 | 0.6 | 1.7 | 6.6 | 23.4 | 35.6 | 40.3 |
| Switzerland as of 4 June[40] | 0.6 | 0.0 | 0.0 | 0.1 | 0.1 | 0.6 | 3.4 | 11.6 | 28.2 | |
| United States | ||||||||||
| Colorado as of 3 June[41] | 0.2 | 0.2 | 0.2 | 0.2 | 0.8 | 1.9 | 6.2 | 18.5 | 39.0 | |
| Connecticut as of 3 June[42] | 0.2 | 0.1 | 0.1 | 0.3 | 0.7 | 1.8 | 7.0 | 18.0 | 31.2 | |
| Georgia as of 3 June[43] | 0.0 | 0.1 | 0.5 | 0.9 | 2.0 | 6.1 | 13.2 | 22.0 | ||
| Idaho as of 3 June[44] | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.4 | 3.1 | 8.9 | 31.4 | |
| Indiana as of 3 June[45] | 0.1 | 0.1 | 0.2 | 0.6 | 1.8 | 7.3 | 17.1 | 30.2 | ||
| Kentucky as of 20 May[46] | 0.0 | 0.0 | 0.0 | 0.2 | 0.5 | 1.9 | 5.9 | 14.2 | 29.1 | |
| Maryland as of 20 May[47] | 0.0 | 0.1 | 0.2 | 0.3 | 0.7 | 1.9 | 6.1 | 14.6 | 28.8 | |
| Massachusetts as of 20 May[48] | 0.0 | 0.0 | 0.1 | 0.1 | 0.4 | 1.5 | 5.2 | 16.8 | 28.9 | |
| Minnesota as of 13 May[49] | 0.0 | 0.0 | 0.0 | 0.1 | 0.3 | 1.6 | 5.4 | 26.9 | ||
| Mississippi as of 19 May[50] | 0.0 | 0.1 | 0.5 | 0.9 | 2.1 | 8.1 | 16.1 | 19.4 | 27.2 | |
| Missouri as of 19 May[51] | 0.0 | 0.0 | 0.1 | 0.2 | 0.8 | 2.2 | 6.3 | 14.3 | 22.5 | |
| Nevada as of 20 May[52] | 0.0 | 0.3 | 0.3 | 0.4 | 1.7 | 2.6 | 7.7 | 22.3 | ||
| N. Hampshire as of 12 May[53] | 0.0 | 0.0 | 0.4 | 0.0 | 1.2 | 0.0 | 2.2 | 12.0 | 21.2 | |
| Oregon as of 12 May[54] | 0.0 | 0.0 | 0.0 | 0.0 | 0.5 | 0.8 | 5.6 | 12.1 | 28.9 | |
| Texas as of 20 May[55] | 0.0 | 0.5 | 0.4 | 0.3 | 0.8 | 2.1 | 5.5 | 10.1 | 30.6 | |
| Virginia as of 19 May[56] | 0.0 | 0.0 | 0.0 | 0.1 | 0.4 | 1.0 | 4.4 | 12.9 | 24.9 | |
| Washington as of 10 May[57] | 0.0 | 0.2 | 1.3 | 9.8 | 31.2 | |||||
| Wisconsin as of 20 May[58] | 0.0 | 0.0 | 0.2 | 0.2 | 0.6 | 2.0 | 5.0 | 14.7 | 19.9 | 30.4 |
| Age | 0–19 | 20–44 | 45–54 | 55–64 | 65–74 | 75–84 | 85+ |
|---|---|---|---|---|---|---|---|
| United States as of 16 March[59] | 0.0 | 0.1–0.2 | 0.5–0.8 | 1.4–2.6 | 2.7–4.9 | 4.3–10.5 | 10.4–27.3 |
| Note: The lower bound includes all cases. The upper bound excludes cases that were missing data. | |||||||
| Percent of infected people who are hospitalized | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| 0–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80+ | Total | |
| Female | 0.2 (0.1–0.3) |
0.6 (0.3–0.9) |
1.1 (0.7–1.8) |
1.6 (0.9–2.4) |
3.2 (1.9–4.9) |
6.2 (3.7–9.6) |
9.6 (5.7–14.8) |
23.6 (14.0–36.4) |
3.2 (1.9–5.0) |
| Male | 0.2 (0.1–0.3) |
0.7 (0.4–1.1) |
1.4 (0.9–2.2) |
1.9 (1.1–3.0) |
3.9 (2.3–6.1) |
8.1 (4.8–12.6) |
13.4 (8.0–20.7) |
45.9 (27.3–70.9) |
4.0 (2.4–6.2) |
| Total | 0.2 (0.1–0.3) |
0.6 (0.4–1.0) |
1.3 (0.8–2.0) |
1.7 (1.0–2.7) |
3.5 (2.1–5.4) |
7.1 (4.2–11.0) |
11.3 (6.7–17.5) |
32.0 (19.0–49.4) |
3.6 (2.1–5.6) |
| Percent of hospitalized people who go to Intensive Care Unit | |||||||||
| 0–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80+ | Total | |
| Female | 16.7 (14.4–19.2) |
8.6 (7.5–9.9) |
11.9 (10.9–13.0) |
16.6 (15.6–17.7) |
20.7 (19.8–21.7) |
23.1 (22.2–24.0) |
18.7 (18.0–19.5) |
4.2 (4.0–4.5) |
14.3 (13.9–14.7) |
| Male | 26.9 (23.2–31.0) |
14.0 (12.2–15.9) |
19.2 (17.6–20.9) |
26.9 (25.3–28.5) |
33.4 (32.0–34.8) |
37.3 (36.0–38.6) |
30.2 (29.2–31.3) |
6.8 (6.5–7.2) |
23.1 (22.6–23.6) |
| Total | 22.2 (19.2–25.5) |
11.5 (10.1–13.2) |
15.9 (14.6–17.3) |
22.2 (21.0–23.5) |
27.6 (26.5–28.7) |
30.8 (29.8–31.8) |
24.9 (24.1–25.8) |
5.6 (5.3–5.9) |
19.0 (18.7–19.44) |
| Percent of hospitalized people who die | |||||||||
| 0–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80+ | Total | |
| Female | 0.5 (0.2–1.1) |
0.9 (0.5–1.3) |
1.5 (1.2–1.9) |
2.6 (2.3–3.0) |
5.2 (4.8–5.6) |
10.1 (9.5–10.6) |
16.7 (16.0–17.4) |
25.2 (24.4–26.0) |
14.4 (14.0–14.9) |
| Male | 0.7 (0.3–1.5) |
1.3 (0.8–1.9) |
2.2 (1.7–2.7) |
3.8 (3.4–4.4) |
7.6 (7.0–8.2) |
14.8 (14.1–15.6) |
24.6 (23.7–25.6) |
37.1 (36.1–38.2) |
21.22 (20.8–21.7) |
| Total | 0.6 (0.3–1.3) |
1.1 (0.7–1.6) |
1.9 (1.5–2.3) |
3.3 (2.9–3.7) |
6.5 (6.0–7.0) |
12.6 (12.0–13.2) |
21.0 (20.3–21.8) |
31.6 (30.9–32.4) |
18.1 (17.8–18.4) |
| Percent of infected people who die – infection fatality rate (IFR) | |||||||||
| 0–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80+ | Total | |
| Female | 0.001 (<0.001–0.002) |
0.005 (0.002–0.009) |
0.02 (0.01–0.03) |
0.04 (0.02–0.07) |
0.2 (0.1–0.3) |
0.6 (0.4–1.0) |
1.6 (1.0–2.5) |
5.9 (3.5–9.2) |
0.5 (0.3–0.7) |
| Male | 0.001 (<0.001–0.003) |
0.008 (0.004–0.02) |
0.03 (0.02–0.05) |
0.07 (0.04–0.1) |
0.3 (0.2–0.5) |
1.2 (0.7–1.9) |
3.3 (2.0–5.1) |
17.1 (10.1–26.3) |
0.8 (0.5–1.3) |
| Total | 0.001 (<0.001–0.002) |
0.007 (0.003–0.01) |
0.02 (0.01–0.04) |
0.06 (0.03–0.09) |
0.2 (0.1–0.36) |
0.9 (0.5–1.4) |
2.4 (1.4–3.7) |
10.1 (6.0–15.6) |
0.7 (0.4–1.0) |
| Numbers in parentheses are 95% credible intervals for the estimates. | |||||||||
| 0–9 | 10–19 | 20–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70–79 | 80+ | |
|---|---|---|---|---|---|---|---|---|---|
| Severe disease | 0.0 (0.0–0.0) |
0.04 (0.02–0.08) |
1.0 (0.62–2.1) |
3.4 (2.0–7.0) |
4.3 (2.5–8.7) |
8.2 (4.9–17) |
11 (7.0–24) |
17 (9.9–34) |
18 (11–38) |
| Death | 0.0016 (0.00016–0.025) |
0.0070 (0.0015–0.050) |
0.031 (0.014–0.092) |
0.084 (0.041–0.19) |
0.16 (0.076–0.32) |
0.60 (0.34–1.3) |
1.9 (1.1–3.9) |
4.3 (2.5–8.4) |
7.8 (3.8–13) |
| Total infection fatality rate is estimated to be 0.66% (0.39–1.3). Infection fatality rate is fatality per all infected individuals, regardless of whether they were diagnosed or had any symptoms. Numbers in parentheses are 95% credible intervals for the estimates. | |||||||||
Mortality by gender
As of April 2020, men die more often than women after being affected with COVID-19 infection.[62][63][64] The highest risk gap for men is in their 50s, with the gap between men and women closing only at 90.[63] In China, the death rate was 2.8 percent for men and 1.7 percent for women.[63] The exact reasons for this sex-difference is not known, but genetic and behavioural factors could be a reason for this difference.[62] Sex-based immunological differences, lesser prevalence of smoking in women and men developing co-morbid conditions such as hypertension at a younger age than women could have contributed to the higher mortality in men.[63] In Europe, 57% of the infected individuals were men and 72% of those died with COVID-19 were men.[65] As of April 2020, the US government is not tracking sex-related data of COVID-19 infections.[66] Research has shown that viral illnesses like Ebola, HIV, influenza and SARS affect men and women differently.[66]
Mortality in people with co-morbidities
Individuals with comorbidities such as diabetes, hypertension and malignancy had poorer outcomes of treatment following COVID-19 infection.[67][68] In Italy, the most common comorbidities observed in deceased patients were hypertension (69%), diabetes (32%), ischemic heart disease (27%), atrial fibrillation (21%), chronic obstructive pulmonary disease (18%) and active cancer in the last 5 years (16%).[69] In New York state, 86% of deaths from COVID-19 had at least one comorbidity.[70]
Causes for mortality
The main cause of death in people with COVID-19 is respiratory failure, similar to the causes of death in types of flu.[71] In order to promote recovery, invasive mechanical ventilation is recommended until the lungs recover from the injury.[2] Extracorporeal membrane oxygenation can be used if the situation deteriorates further.[2] Other causes of mortality in COVID-19 infection are septic shock and multiple organ failure.[72][73] In Wuhan, about 15% of the patients developed severe pneumonia and 6% needed ventilatory support. In Wuhan, only around 25% of those who died received extracorporeal membrane oxygenation because of shortage of trained staff.[74] The role of secondary bacterial infections in mortality is not well-described in literature.[2] Acute kidney injury, cardiogenic shock due to acute myocardial injury or myocarditis are also causes of death due to COVID-19.[2]
It is difficult to differentiate between those who died due to COVID-19 or as a result of overload of cases in hospitals. Critically ill people infected with COVID-19 could not sometimes be given adequate treatment because of shortage of resources and a part of COVID-19 mortality could be because of insufficient hospital facilities.[75]
Predictors of mortality
Low lymphocyte count, high C-reactive protein and high D-dimer levels are frequently found in non-survivors.[71][72][74] The change of lymphocyte count during the first four days of hospital admission was highly associated with mortality in China.[74]
Mortality by country
The official deaths reported usually do not give accurate numbers because this may ignore those who died without testing, such as at nursing homes or residences.[76] Conversely, in countries with high rates of COVID-19 infection, patients might be admitted to the hospital due to unrelated illnesses, but they could also have COVID-19. When these patients succumb to death due to the initial condition, their deaths are usually attributed to COVID-19 although the actual contribution of COVID-19 to the death is minimal.[2] The measures for quantifying mortality are affected by the time since initial outbreak, population characteristics (prominently, age and gender), quality of healthcare system, availability of treatment options and volume of testing.[77] How COVID-19 deaths are recorded may differ between countries because of the differences in counting them.[78]
References
- "Worldwide Coronavirus Statistics". Coronavirus Dashboard. Retrieved 7 June 2020.
- Vincent, Jean-Louis; Taccone, Fabio S. (6 April 2020). "Understanding pathways to death in patients with COVID-19". The Lancet Respiratory Medicine. 0. doi:10.1016/S2213-2600(20)30165-X. ISSN 2213-2600. PMID 32272081. Retrieved 26 April 2020.
- "COVID-19 Virus Pandemic". www.worldometers.info. Retrieved 28 June 2020.
10,229,030 Cases, 503,985 Deaths, 5,546,483 Recovered
- "Coronavirus Live Updates: First Death Outside Asia Reported in France". The New York Times. 15 February 2020. Retrieved 15 February 2020.
- Ramzy A, May T (2 February 2020). "Philippines Reports First Coronavirus Death Outside China". The New York Times. Archived from the original on 3 February 2020. Retrieved 4 February 2020.
- "WHO situation report" (PDF). Retrieved 26 April 2020.
- "ArcGIS Dashboards". gisanddata.maps.arcgis.com. Retrieved 26 April 2020.
- "Global Covid-19 Case Fatality Rates". CEBM. Retrieved 27 April 2020.
- Lazzerini, Marzia; Putoto, Giovanni (18 March 2020). "COVID-19 in Italy: momentous decisions and many uncertainties". The Lancet Global Health. 0 (5): e641–e642. doi:10.1016/S2214-109X(20)30110-8. ISSN 2214-109X. PMC 7104294. PMID 32199072. Retrieved 26 April 2020.
- Roques, Lionel; Klein, Etienne K.; Papaïx, Julien; Sar, Antoine; Soubeyrand, Samuel (May 2020). "Using Early Data to Estimate the Actual Infection Fatality Ratio from COVID-19 in France". Biology. 9 (5): 97. doi:10.3390/biology9050097.
- Verity, Robert; Okell, Lucy C; Dorigatti, Ilaria; Winskill, Peter; Whittaker, Charles; Imai, Natsuko; Cuomo-Dannenburg, Gina; Thompson, Hayley; Walker, Patrick G T; Fu, Han; Dighe, Amy (March 2020). "Estimates of the severity of coronavirus disease 2019: a model-based analysis". The Lancet Infectious Diseases. doi:10.1016/s1473-3099(20)30243-7. ISSN 1473-3099. PMC 7158570. PMID 32240634.
- Mahase, Elisabeth (1 April 2020). "Covid-19: death rate is 0.66% and increases with age, study estimates". BMJ. 369: m1327. doi:10.1136/bmj.m1327. ISSN 1756-1833. PMID 32238354. Retrieved 27 April 2020.
- "Sala de Situación COVID-19 Nuevo Coronavirus 2019 Novedades al 07/05 - 18 hs- SE 19" (PDF) (in Spanish). 7 May 2020.
- Health, Australian Government Department of (2020-06-04). "COVID-19 cases by age group and sex". Australian Government Department of Health. Retrieved 2020-06-04. Health, Australian Government Department of (2020-06-04). "COVID-19 deaths by age group and sex". Australian Government Department of Health. Retrieved 2020-06-04.
- "Coronavirus Disease 2019 (COVID-19) DAILY EPIDEMIOLOGY UPDATE Updated: 3 June, 2020, 11:00 AM ET" (PDF). Public Health Agency of Canada. 3 June 2020. Retrieved 4 June 2020.
- https://www.alberta.ca/stats/covid-19-alberta-statistics.htm
- http://www.bccdc.ca/Health-Info-Site/Documents/BC_Surveillance_Summary_June_3_2020.pdf
- "Ontario COVID-19 Data Tool". Public Health Ontario.
- "Situation of the coronavirus (COVID-19) in Québec". www.quebec.ca.
- "22° informe epidemiológico COVID-19". Ministerio de Salud – Gobierno de Chile.
- https://cdn.digital.gob.cl/public_files/Campañas/Corona-Virus/Reportes/01.06.2020_Reporte_Covid19.pdf
- Yanping Z, et al. (The Novel Coronavirus Pneumonia Emergency Response Epidemiology Team) (17 February 2020). "The Epidemiological Characteristics of an Outbreak of 2019 Novel Coronavirus Diseases (COVID-19)—China, 2020". China CDC Weekly. Chinese Center for Disease Control and Prevention. 2 (8): 113–122. Archived from the original on 19 February 2020. Retrieved 18 March 2020.
- "Coronavirus Colombia". www.ins.gov.co.
- Overvågning af COVID-19 (Report) (in Danish). Statens Serum Institut. 2020-06-04. Retrieved 2020-06-04.
- "Confirmed coronavirus cases (COVID-19) in Finland". experience.arcgis.com. THL. "Tilannekatsaus koronaviruksesta - Infektiotaudit ja rokotukset - THL". Terveyden ja hyvinvoinnin laitos.
- "Coronavirus Disease 2019 (COVID-19) Daily Situation Report of the Robert Koch Institute 05/06/2020 - UPDATED STATUS FOR GERMANY" (PDF). Robert Koch Institute.
- https://www.lgl.bayern.de/gesundheit/infektionsschutz/infektionskrankheiten_a_z/coronavirus/karte_coronavirus/index.htm
- "קורונה - משרד הבריאות". Ministry of Health (Israel). 3 May 2020. Retrieved 5 May 2020.
- "Integrated surveillance of COVID-19 in Italy" (PDF). Istituto Superiore di Sanità.
- "Coronavirus Disease (COVID-19) Situation Report in Japan". toyokeizai.net.
- COVID-19 Tablero México - CONACYT (Report) (in Spanish). Mexico City: CONACYT. 2020-06-03. Retrieved 2020-06-04.
- Epidemiologische situatie COVID-19 in Nederland 3 juni 2020 (Report) (in Dutch). Bilthoven: Rijksinstituut voor Volksgezondheid en Milie. 2020-06-04. Retrieved 2020-06-04.
- "COVID-19 Dagsrapport fredag 4. juni 2020" (PDF). Folkehelseinstituttet. 2020-06-04. Retrieved 2020-06-04.
- "COVID-19 Tracker | Department of Health website". Doh.gov.ph. 2020-06-04. Retrieved 2020-06-04.
- "NOVO CORONAVÍRUS COVID-19 RELATÓRIO DE SITUAÇÃO" (PDF) (in Portuguese). 2020-06-04. Retrieved 2020-06-04.
- "Update on Covid-19 (28th May 2020)". sacoronavirus.co.za. May 29, 2020.
- 코로나바이러스감염증-19 국내 발생 현황 (6월 15일, 정례브리핑) (Report). Korea Centers for Disease Control and Prevention. 2020-06-15. Retrieved 2020-06-15.
- Actualización nº 109. Enfermedad por el coronavirus (COVID-19) (PDF) (Report) (in Spanish). Ministerio de Sanidad, Consumo y Bienestar Social. 18 May 2020. Retrieved 20 May 2020.
- "FOHM Covid-19". Public Health Agency of Sweden. 2020-06-05. Retrieved 2020-06-05.
- "Todesfälle in der Schweiz nach Altersgruppen". datawrapper.dwcdn.net. 2020-06-04. Retrieved 2020-06-04.
- "Case data | Colorado COVID-19 Updates". covid19.colorado.gov.
- "COVID-19 confirmed cases and deaths by age group | Connecticut Data". data.ct.gov. 3 June 2020. Retrieved 4 June 2020.
- https://dph.georgia.gov/covid-19-daily-status-report
- "Tableau Public". public.tableau.com.
- "COVID-19 Case Demographics - the Indiana Data Hub". hub.mph.in.gov.
- "KDPH COVID-19 Dashboard". Kygeonet.maps.arcgis.com. Retrieved 21 May 2020.
- https://coronavirus.maryland.gov Probable but not lab-confirmed deaths not included
- "COVID-19 Response Reporting". Mass.gov. 20 May 2020. Retrieved 20 May 2020.
- https://www.health.state.mn.us/diseases/coronavirus/stats/covidweekly10.pdf
- "Coronavirus COVID-19 - Mississippi State Department of Health". msdh.ms.gov. 19 May 2020. Retrieved 20 May 2020.
- "Story Map Series". mophep.maps.arcgis.com.
- "Microsoft Power BI". app.powerbigov.us.
- "Microsoft Word - HAV Situation Report #6 07MAY19" (PDF). Retrieved 2020-06-03.
- "Oregon Health Authority | COVID-19 Updates". govstatus.egov.com.
- "Texas COVID-19 Data". Dshs.texas.gov. Retrieved 2020-06-03.
- "COVID-19 Cases in Virginia: Demographics". public.tableau.com. 20 May 2020. Retrieved 20 May 2020.
- "2019 Novel Coronavirus Outbreak (COVID-19)". Washington State Department of Health. 19 May 2020. Retrieved 20 May 2020.
- "COVID-19: Wisconsin Deaths". Wisconsin Department of Health Services. 17 April 2020.
- CDC COVID-19 Response Team (18 March 2020). "Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19)—United States, February 12 – March 16, 2020". Morbidity and Mortality Weekly Report. Centers for Disease Control. 69 (12): 343–346. doi:10.15585/mmwr.mm6912e2. PMID 32214079. Archived from the original on 22 March 2020. Retrieved 22 March 2020.
- Salje, Henrik; Tran Kiem, Cécile; Lefrancq, Noémie; Courtejoie, Noémie; Bosetti, Paolo; Paireau, Juliette; Andronico, Alessio; Hozé, Nathanaël; Richet, Jehanne; Dubost, Claire-Lise; Le Strat, Yann (2020-05-13). "Estimating the burden of SARS-CoV-2 in France". Science: eabc3517. doi:10.1126/science.abc3517. ISSN 0036-8075.
- Verity, Robert; Okell, Lucy C; Dorigatti, Ilaria; Winskill, Peter; Whittaker, Charles; Imai, Natsuko; Cuomo-Dannenburg, Gina; Thompson, Hayley; Walker, Patrick G T; Fu, Han; Dighe, Amy (30 March 2020). "Estimates of the severity of coronavirus disease 2019: a model-based analysis". The Lancet Infectious Diseases. doi:10.1016/s1473-3099(20)30243-7. ISSN 1473-3099. PMC 7158570. PMID 32240634.
- Wenham, Clare; Smith, Julia; Morgan, Rosemary (14 March 2020). "COVID-19: the gendered impacts of the outbreak". The Lancet. 395 (10227): 846–848. doi:10.1016/S0140-6736(20)30526-2. ISSN 0140-6736. PMC 7124625. PMID 32151325.
- Rabin, Roni Caryn (20 March 2020). "In Italy, Coronavirus Takes a Higher Toll on Men". The New York Times. Retrieved 7 April 2020.
- Chen, Nanshan; Zhou, Min; Dong, Xuan; Qu, Jieming; Gong, Fengyun; Han, Yang; Qiu, Yang; Wang, Jingli; Liu, Ying; Wei, Yuan; Xia, Jia'an; Yu, Ting; Zhang, Xinxin; Zhang, Li (15 February 2020). "Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study". The Lancet. 395 (10223): 507–513. doi:10.1016/S0140-6736(20)30211-7. ISSN 0140-6736. PMC 7135076. PMID 32007143. Retrieved 7 April 2020.
- "COVID-19 weekly surveillance report". www.euro.who.int. Retrieved 7 April 2020.
- Gupta, Alisha Haridasani (3 April 2020). "Does Covid-19 Hit Women and Men Differently? U.S. Isn't Keeping Track". The New York Times. Retrieved 7 April 2020.
- Guan, Wei-jie; Liang, Wen-hua; Zhao, Yi; Liang, Heng-rui; Chen, Zi-sheng; Li, Yi-min; Liu, Xiao-qing; Chen, Ru-chong; Tang, Chun-li; Wang, Tao; Ou, Chun-quan; Li, Li; Chen, Ping-yan; Sang, Ling; Wang, Wei; Li, Jian-fu; Li, Cai-chen; Ou, Li-min; Cheng, Bo; Xiong, Shan; Ni, Zheng-yi; Xiang, Jie; Hu, Yu; Liu, Lei; Shan, Hong; Lei, Chun-liang; Peng, Yi-xiang; Wei, Li; Liu, Yong; Hu, Ya-hua; Peng, Peng; Wang, Jian-ming; Liu, Ji-yang; Chen, Zhong; Li, Gang; Zheng, Zhi-jian; Qiu, Shao-qin; Luo, Jie; Ye, Chang-jiang; Zhu, Shao-yong; Cheng, Lin-ling; Ye, Feng; Li, Shi-yue; Zheng, Jin-ping; Zhang, Nuo-fu; Zhong, Nan-shan; He, Jian-xing (1 January 2020). "Comorbidity and its impact on 1590 patients with Covid-19 in China: A Nationwide Analysis". European Respiratory Journal: 2000547. doi:10.1183/13993003.00547-2020. ISSN 0903-1936. PMC 7098485. PMID 32217650. Retrieved 27 April 2020.
- Halpin, David M. G.; Faner, Rosa; Sibila, Oriol; Badia, Joan Ramon; Agusti, Alvar (3 April 2020). "Do chronic respiratory diseases or their treatment affect the risk of SARS-CoV-2 infection?". The Lancet Respiratory Medicine. 0. doi:10.1016/S2213-2600(20)30167-3. ISSN 2213-2600. PMID 32251625. Retrieved 27 April 2020.
- "Most common comorbidities in COVID-19 deceased patients in Italy 2020". statista.com. 27 April 2020. Retrieved 4 May 2020.
- Franki, Richard (8 April 2020). "Comorbidities the rule in New York's COVID-19 deaths". www.the-hospitalist.org. Society of Hospital Medicine. Retrieved 27 April 2020.
- Ruan, Qiurong; Yang, Kun; Wang, Wenxia; Jiang, Lingyu; Song, Jianxin (3 March 2020). "Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China". Intensive Care Medicine. doi:10.1007/s00134-020-05991-x. ISSN 1432-1238. PMC 7080116. PMID 32125452.
- Chen, Nanshan; Zhou, Min; Dong, Xuan; Qu, Jieming; Gong, Fengyun; Han, Yang; Qiu, Yang; Wang, Jingli; Liu, Ying; Wei, Yuan; Xia, Jia'an; Yu, Ting; Zhang, Xinxin; Zhang, Li (15 February 2020). "Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study". The Lancet. 395 (10223): 507–513. doi:10.1016/S0140-6736(20)30211-7. ISSN 0140-6736. PMC 7135076. PMID 32007143. Retrieved 26 April 2020.
- Wang, Dawei; Hu, Bo; Hu, Chang; Zhu, Fangfang; Liu, Xing; Zhang, Jing; Wang, Binbin; Xiang, Hui; Cheng, Zhenshun; Xiong, Yong; Zhao, Yan; Li, Yirong; Wang, Xinghuan; Peng, Zhiyong (17 March 2020). "Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus–Infected Pneumonia in Wuhan, China". JAMA. 323 (11): 1061–1069. doi:10.1001/jama.2020.1585. ISSN 0098-7484. PMC 7042881. PMID 32031570.
- Xie, Jianfeng; Tong, Zhaohui; Guan, Xiangdong; Du, Bin; Qiu, Haibo; Slutsky, Arthur S. (2 March 2020). "Critical care crisis and some recommendations during the COVID-19 epidemic in China". Intensive Care Medicine. doi:10.1007/s00134-020-05979-7. ISSN 1432-1238. PMC 7080165. PMID 32123994.
- Rosenbaum, Lisa (18 March 2020). "Facing Covid-19 in Italy — Ethics, Logistics, and Therapeutics on the Epidemic's Front Line". New England Journal of Medicine. 0. doi:10.1056/NEJMp2005492. ISSN 0028-4793. PMID 32187459.
- "Italy's coronavirus deaths could be underestimated in data: official". Reuters. 31 March 2020. Retrieved 26 April 2020.
- Morris, Chris; Reuben, Anthony (29 April 2020). "Can you compare different countries?". BBC News. Retrieved 2 May 2020.
- Roser, Max; Ritchie, Hannah; Ortiz-Ospina, Esteban; Hasell, Joe (4 March 2020). "Coronavirus Pandemic (COVID-19)". Our World in Data. Retrieved 27 April 2020.