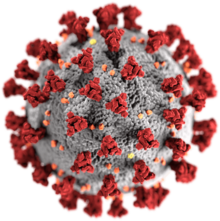
Impact of the COVID-19 pandemic on healthcare workers
The COVID-19 pandemic has impacted healthcare workers physically and psychologically.[1] Healthcare workers are more vulnerable to COVID-19 infection than the general population because of being frequently in contact with affected individuals. Healthcare workers have been required to work under stressful conditions, without proper protective equipment and had to take difficult decisions involving ethical implications. In the US, black healthcare workers are disproportionately impacted by the pandemic due to staff shortage, poor working conditions and poor mental health care system.[2] Health and social systems across the globe are struggling to cope. The situation is especially challenging in humanitarian, fragile and low-income country contexts, where health and social systems are already weak. Services to provide sexual and reproductive health care risk being sidelined, which will lead to higher maternal mortality and morbidity.[3][4]
| Part of a series on the |
| COVID-19 pandemic |
|---|
 |
|
|
|
International response |
|
Medical response |
|
|
|
Risk of infection
The World Health Organization reported that one in ten health workers is infected with coronavirus in some countries.[1] In March 2020, 9% of those affected with COVID-19 in Italy were health workers.[5] In May 2020, the International Council of Nurses reported that at least 90,000 healthcare workers have been infected and more than 260 nurses had died in the COVID-19 pandemic.[6] In March 2020, one in four doctors in the UK were off sick, in isolation or caring for a family member with COVID-19.[7]
The UK government announced that retired healthcare professionals be brought out of retirment to help during the COVID-19 crisis. This led to concerns that they could be at a higher risk for severe COVID-19 illness.[8]
Shortage of PPEs
Shortcomings of personal protective equipment have been reported from several countries.[9][8] In China, inadequate staff training, shortage of PPEs, reduced understanding of PPE use and confused PPE guidance have resulted in infections and deaths among healthcare workers.[10]
Psychological impact
A study from Singapore showed that healthcare workers caring for patients with COVID-19 reported anxiety, depression and stress.[13] Increasing work demands on healthcare professionals conflict with their duties to family and friends, which causes psychological stress.[8] Healthcare professionals reported being anxious about having to self-isolate, quarantine or becoming ill.[14] For healthcare workers, being quarantined was positively associated with minimising direct contact with patients and not reporting to work.[15]
An Italian nurse committed suicide after being traumatized trying to save lives of those with COVID-19.[16]
Violence against healthcare workers
Healthcare workers have been subjected to violent crimes. Hospitals and governments had to take stricter measures to ensure the safety of their staff.[17]
Ethical decisions
The Conversation reports that healthcare workers will have to face 'moral injury' for making difficult decisions such as moving a patient off the ventilator or refusing an ICU bed due to the limtation in resources.[8]
Impact on female staff
Globally, women make up 70 percent of workers in the health and social sector. Women are playing a disproportionate role in responding to the disease, including as front line healthcare workers (as well as carers at home and community leaders and mobilisers). In some countries, COVID-19 infections among female health workers are twice that of their male counterparts.[18][19][20]
Recommendations
World Health Organization
The World Health Organization has given the following key recommendations to decrease the spread of COVID-19 among healthcare workers:[1]
- Training healthcare workers to identify respiratory diseases
- Providing increased access to personal protective equipment
- Providing psychological support to health workers
- Routinely conducting hospital surveillance
- Recognizing that every healthcare system can have gaps
UNFPA
UNFPA recommends that all women and girls must have access to a continuum of sexual and reproductive health services, including antenatal, perinatal and postnatal care, and screening tests according to national guidelines and standards.[3][4]
Karolinska Institute
The Karolinska Institute recommends health workers to take care of oneself, avoid unhelpful strategies, stay in touch with loved ones, not blame oneself and reach out if physical or psychological help is required.[21]
References
- "How to protect health workers now: WHO COVID-19 briefing". World Economic Forum. Retrieved 13 May 2020.
- Wingfield, Adia Harvey (14 May 2020). "The Disproportionate Impact of Covid-19 on Black Health Care Workers in the U.S." Harvard Business Review. Retrieved 27 May 2020.
- Continuing essential Sexual, Reproductive, Maternal, Neonatal, Child and Adolescent Health services during COVID-19 pandemic (PDF). World Health Organization, UNFPA, UNICEF. 2020.
- Coronavirus Disease (COVID-19) Pandemic UNFPA Global Response Plan (PDF). UNFPA. 2020.
- Mitchell, Gemma (20 March 2020). "Nurses among confirmed deaths from Covid-19 around the world". Nursing Times. Retrieved 13 May 2020.
- "90,000 healthcare workers infected with COVID-19: ICN". www.aa.com.tr. Retrieved 13 May 2020.
- "Covid-19: One in four doctors off sick or in isolation". ITV News. Retrieved 13 May 2020.
- Taegtmeyer, Miriam; Wingfield, Tom. "Healthcare workers and coronavirus: behind the stiff upper lip we are highly vulnerable". The Conversation. Retrieved 13 May 2020.
- "Begging for Thermometers, Body Bags, and Gowns: U.S. Health Care Workers Are Dangerously Ill-Equipped to Fight COVID-19". Time. Retrieved 13 May 2020.
- Wang, J.; Zhou, M.; Liu, F. (1 May 2020). "Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China". Journal of Hospital Infection. 105 (1): 100–101. doi:10.1016/j.jhin.2020.03.002. ISSN 0195-6701. Retrieved 13 May 2020.
- contributors, Lost on the Frontline (12 May 2020). "A striving school nurse, a devoted pharmacist: the US health workers who died from Covid-19". The Guardian. Retrieved 13 May 2020.
- "50 doctors have now died in Italy as health system struggles amid coronavirus epidemic". The Independent. 28 March 2020. Retrieved 13 May 2020.
- Tan, Benjamin Y.Q.; Chew, Nicholas W.S.; Lee, Grace K.H.; Jing, Mingxue; Goh, Yihui; Yeo, Leonard L.L.; Zhang, Ka; Chin, Howe-Keat; Ahmad, Aftab; Khan, Faheem Ahmed; Shanmugam, Ganesh Napolean; Chan, Bernard P.L.; Sunny, Sibi; Chandra, Bharatendu; Ong, Jonathan J.Y.; Paliwal, Prakash R.; Wong, Lily Y.H.; Sagayanathan, Renarebecca; Chen, Jin Tao; Ying Ng, Alison Ying; Teoh, Hock Luen; Ho, Cyrus S.; Ho, Roger C.; Sharma, Vijay K. (6 April 2020). "Psychological Impact of the COVID-19 Pandemic on Health Care Workers in Singapore". Annals of Internal Medicine. doi:10.7326/M20-1083. ISSN 0003-4819. PMC 7143149. Retrieved 13 May 2020.
- Brooks, Samantha K.; Webster, Rebecca K.; Smith, Louise E.; Woodland, Lisa; Wessely, Simon; Greenberg, Neil; Rubin, Gideon James (14 March 2020). "The psychological impact of quarantine and how to reduce it: rapid review of the evidence". The Lancet. 395 (10227): 912–920. doi:10.1016/S0140-6736(20)30460-8. ISSN 0140-6736. Retrieved 13 May 2020.
- Marjanovic, Zdravko; Greenglass, Esther R.; Coffey, Sue (1 August 2007). "The relevance of psychosocial variables and working conditions in predicting nurses' coping strategies during the SARS crisis: An online questionnaire survey". International Journal of Nursing Studies. 44 (6): 991–998. doi:10.1016/j.ijnurstu.2006.02.012. ISSN 0020-7489. PMC 7094220. Retrieved 13 May 2020.
- Squires, Nick (25 March 2020). "Italian nurse commits suicide as another 683 people die from coronavirus". The Telegraph. Retrieved 13 May 2020.
- "Health workers become unexpected targets during covid-19". The Economist. Retrieved 13 May 2020.
- "UN Secretary-General's policy brief: The impact of COVID-19 on women | Digital library: Publications". UN Women. Retrieved 2020-06-12.
- "Gender equality matters in COVID-19 response". UN Women. Retrieved 2020-06-12.
- "COVID-19: Emerging gender data and why it matters | UN Women Data Hub". data.unwomen.org. Retrieved 2020-06-12.
- "Covid-19: Recommendations and resources for healthcare workers Karolinska Institutet". ki.se.