Pharmacology of progesterone
The pharmacology of progesterone, a progestogen medication and naturally occurring steroid hormone, concerns its pharmacodynamics, pharmacokinetics, and various routes of administration.[13][14]
Progesterone is a naturally occurring and bioidentical progestogen, or an agonist of the progesterone receptor, the biological target of progestogens like endogenous progesterone.[13] Progesterone also has antimineralocorticoid and inhibitory neurosteroid activity, whereas it appears to have little or no glucocorticoid or antiandrogenic activity and has no androgenic activity.[13] Because of its progestogenic activity, progesterone has functional antiestrogenic effects in certain tissues such as the uterus, cervix, and vagina.[13] In addition, progesterone has antigonadotropic effects due to its progestogenic activity and can inhibit fertility and suppress sex hormone production.[13] Progesterone differs from progestins (synthetic progestogens) like medroxyprogesterone acetate and norethisterone, with implications for pharmacodynamics and pharmacokinetics as well as efficacy, tolerability, and safety.[13]
Progesterone can be taken by mouth, in through the vagina, and by injection into muscle or fat, among other routes.[13] A progesterone vaginal ring and progesterone intrauterine device are also available as pharmaceutical products.[15][16]
Pharmacodynamics
Mechanism of action
Progesterone is a progestogen, or an agonist of the nuclear progesterone receptors (PRs), the PR-A, PR-B, and PR-C.[13] In one study, progesterone showed EC50 values of 7.7 nM for the human PR-A and 8.0 nM for the human PR-B.[17] In addition to the PRs, progesterone is an agonist of the membrane progesterone receptors (mPRs), including the mPRα, mPRβ, mPRγ, mPRδ, and mPRϵ.[18][19] It is also a potent antimineralocorticoid (antagonist of the mineralocorticoid receptor (MR)),[20][21] as well as a very weak glucocorticoid (agonist of the glucocorticoid receptor).[22][23] Progesterone does not bind to the androgen receptor (AR) or to the estrogen receptor (ER).[13] In addition to its activity as a steroid hormone, progesterone is a neurosteroid.[24] Specifically, it is an antagonist of the sigma σ1 receptor,[25][26] a negative allosteric modulator of nicotinic acetylcholine receptors,[24] and, via its active metabolites allopregnanolone and pregnanolone, a potent positive allosteric modulator of the GABAA receptor, the major signaling receptor of the inhibitory neurotransmitter γ-aminobutyric acid (GABA).[27]
| Compound | PR | AR | ER | GR | MR | SHBG | CBG |
|---|---|---|---|---|---|---|---|
| Progesterone | 50 | 0 | 0 | 10 | 100 | 0 | 36 |
| Values are percentages (%). Reference ligands (100%) were promegestone for the PR, metribolone for the AR, E2 for the ER, DEXA for the GR, aldosterone for the MR, DHT for SHBG, and cortisol for CBG. Source:[13] | |||||||
| Progestogen | Type | Class | TFD (14 days) | MDT (week) | OID (month) | POIC-D (2–3 months) | CIC-D (month) | Duration |
|---|---|---|---|---|---|---|---|---|
| Algestone acetophenide | Synthetic | Pregnane | ND | ND | ND | NA | 75–150 mg | ND |
| Gestonorone caproate | Synthetic | Norpregnane | ND | ND | ND | NA | NA | ND |
| Hydroxyprogesterone caproate | Synthetic | Pregnane | 250–500 mg | 25 mg | 250–500 mg | NA | 250–500 mg | 250 mg ≈ 10 days |
| Medroxyprogesterone acetate | Synthetic | Pregnane | 50–100 mg | ND | ND | 150 mg | 25 mg | 50 mg ≈ 14 days |
| Megestrol acetate | Synthetic | Pregnane | ND | ND | ND | NA | 25 mg | ND |
| Norethisterone enanthate | Synthetic | Estrane | ND | ND | ND | 200 mg | 50 mg | ND |
| Progesterone (oil soln.) | Bioidentical | Pregnane | 200 mg | ND | ND | NA | NA | 25 mg ≈ 2–3 days |
| Progesterone (cryst. susp.) | Bioidentical | Pregnane | 50–100 mg | ND | ND | NA | NA | 50 mg ≈ 14 days |
| Notes: All by intramuscular injection. Abbreviations: TFD = Endometrial transformation dose. MDT = Menstrual delay test dose (Greenblatt). OID = Ovulation-inhibiting dose (antigonadotropic effect; without an estrogen). POIC-D = Progestogen-only injectable contraceptive dose(s). CIC-D = Combined injectable contraceptive dose(s). Miscellaneous: Direct link to table. Sources:[28][29][30][31][32] | ||||||||
Effects in the body and brain
The PRs are expressed widely throughout the body, including in the uterus, cervix, vagina, fallopian tubes, breasts, fat, skin, pituitary gland, hypothalamus, and elsewhere throughout the brain.[13][33] Through activation of the PRs (as well as the mPRs), progesterone has many effects, including the following:[13][33]
- Induces endometrial secretory transformation in preparation for pregnancy
- Prevents estrogen-induced endometrial hyperplasia and increased endometrial cancer risk
- Maintains pregnancy via effects in endometrium (with withdrawal resulting in miscarriage)
- Reduces amount and fibrosity of cervical mucus and causes cervix to become firmer and more tightly closed[34]
- Controls motility and composition of fluid in the fallopian tubes
- Reduced cornification and maturation of the vaginal lining[35]
- Causes water retention in the breasts resulting in temporary enlargement during the menstrual cycle[36][37]
- Mediates lobuloalveolar development of the breasts necessary for lactation
- Suppresses lactation initiation and triggers lactation upon withdrawal (as with parturition)
- Maintains skin health, integrity, appearance, and hydration and slows the rate of aging of the skin[38][39]
- Modulates brain function, with effects on mood, emotionality, and sexuality, as well as cognition and memory
- Exerts negative feedback on the hypothalamic–pituitary–gonadal axis (HPG axis) by suppressing the secretion of the gonadotropins FSH and LH from the pituitary gland (including the mid-cycle gonadotropin surge), thereby inhibiting gonadal sex hormone production as well as ovulation and fertility
- Increases basal body temperature (by 0.3–0.6 °C (0.5–1.0 °F) relative to preovulation) via the hypothalamus[40]
- Reduces hot flashes via the hypothalamus[41][42]
- Stimulates respiration via the hypothalamus and/or respiratory center[43][44]
- Influences the risk and/or progression of hormone-sensitive cancers including breast cancer and endometrial cancer
It should be noted that many of the effects of progesterone require estrogen, as estrogens prime tissues for progesterone by inducing expression of the PRs.[13][33] The PRs are induced in the breasts by estrogens, and for this reason, it is assumed that progestogens cannot mediate breast changes in the absence of estrogens.[45]
Progesterone also lowers blood pressure and reduces water and salt retention among other effects via its antimineralocorticoid activity.[13][46]
Progesterone can produce sedative, hypnotic, anxiolytic, euphoric, cognitive-, memory-, and motor-impairing, anticonvulsant, and even anesthetic effects via formation of sufficiently high concentrations of its neurosteroid metabolites and consequent GABAA receptor potentiation in the brain.[47][48][49][50]
Antiestrogenic effects
Progesterone, like all progestogens, has antiestrogenic effects in certain tissues such as the uterus, cervix, and vagina and possibly also the breasts and brain.[13][51][52] These effects are mediated by activation of the PR in these tissues.[13] Progesterone does not have antiestrogenic effects in the more conventional sense of binding to and antagonizing the ER or binding to and inhibiting enzymes involved in estrogen biosynthesis.[13] Instead, for instance in the endometrium, progesterone causes downregulation of the ER and upregulation of the estrogen-inactivating enzymes 17β-hydroxysteroid dehydrogenase 2 (converts estradiol into estrone) and estrone sulfotransferase (converts estrone into estrone sulfate).[13] In the breasts, progesterone similarly downregulates the ER as well as the estrogen-activating enzymes steroid sulfatase (converts estrone sulfate into estrone) and 17β-hydroxysteroid-dehydrogenase 1 (converts estrone into estradiol) and upregulates estrone sulfotransferase.[51][52] The antiestrogenic effects of progesterone and other progestogens form the basis for their only approved indication in menopausal hormone therapy: prevention of long-term unopposed estrogen-induced endometrial hyperplasia and increased endometrial cancer risk in women with intact uteruses.[13]
It has been hypothesized that progestogens may counteract various effects of estrogens in the brain such as stimulatory and excitatory effects on neuronal activity.[13] Progesterone moreover has a special position among progestogens concerning such actions due to its inhibitory neurosteroid metabolites and their central depressant effects.[13] It has been suggested that these actions of progestogens may explain the unfavorable effects on mood that have been observed with these medications in some women.[13] However, the mutual interactions of estrogens and progestogens in the brain in general are controversial and require more research.[13]
Progesterone can also have body-wide antiestrogenic effects at very high doses in both women and men via its antigonadotropic effects and consequent suppression of gonadal estrogen production (see below).[13][53] These antigonadotropic effects are mediated by hyperactivation of the PR.[13][53]
Antigonadotropic effects
Progestogens have antigonadotropic effects at sufficiently high dosages via activation of the PR and consequent negative feedback on and hence suppression of the hypothalamic–pituitary–gonadal axis (HPG axis).[53] This results in suppression of gonadotropin secretion and by extension interference with fertility and gonadal sex hormone production.[53] The minimum ovulation-inhibiting (i.e., contraceptive) dosage of oral progesterone in women, this effect being the result of suppression of the mid-cycle surge in gonadotropin secretion, is 300 mg/day.[10][54][13] However, this figure is based on limited clinical data.[10] Conversely, treatment with a high dosage of oral progesterone of 100 mg four times per day (or 400 mg/day total) in men for 10 days that resulted in approximately mid-luteal phase levels of progesterone (7.9–9.4 ng/mL; measured by RIA) did not cause any change in testosterone levels, suggesting that progesterone has little or no antigonadotropic effect in males at typical clinical dosages.[47][55] In addition, a study found that administration of 1,000 mg/day oral progesterone for 3 months had no significant effect on urinary gonadotropin excretion.[10] On the other hand, a single 50 mg intramuscular injection of progesterone, which is associated with high progesterone levels of approximately 50 ng/mL (or early- to mid-pregnancy levels),[56][57][58] resulted in substantial (50–60%) suppression of luteinizing hormone, follicle-stimulating hormone, and testosterone levels in men.[59] Similarly, continuous or intermittent intravenous injections of 100 to 400 mg/day progesterone for 10 days significantly decreased urinary gonadotropin excretion.[10] Progestogens in general are able to suppress gonadal testosterone production in men by a maximum of about 70 to 80% or to just above castrate levels when used at sufficiently high dosages.[60][61]
Antimineralocorticoid activity
Progesterone is a potent antimineralocorticoid.[20][21] It has similar or higher affinity for the MR than aldosterone, the major endogenous agonist of the receptor.[13][20] Progesterone produces antimineralocorticoid effects such as natriuresis (excretion of sodium in the urine) at normal physiological concentrations.[21] A 200 mg dose of oral progesterone is considered to be approximately equivalent in antimineralocorticoid effect to a 25 to 50 mg dose of the potent antimineralocorticoid spironolactone, which itself is a derivative of progesterone.[62] The antimineralocorticoid effects of progesterone underlie its ability to lower blood pressure and reduce water and salt retention and its potential application in the treatment of hypertension.[47][13][46] An active metabolite of progesterone, 11-deoxycorticosterone (21-hydroxyprogesterone), is a precursor of aldosterone and has strong mineralocorticoid activity (i.e., is a strong agonist of the MR).[62] However, it is formed in relatively small amounts, and any such effects produced by it are usually outweighed by the antimineralocorticoid activity of progesterone.[62]
Glucocorticoid activity
Progesterone is a partial agonist of the glucocorticoid receptor.[13][22][23][63][64] It has about 10 or 11% of the affinity of the corticosteroid dexamethasone for this receptor.[13][64] However, progesterone appears to show weak or no glucocorticoid activity and no antiglucocorticoid activity in vitro and in animals.[64]
| Steroid | Type | TR (↑)a | GR (%)b |
|---|---|---|---|
| Dexamethasone | Corticosteroid | ++ | 100 |
| Ethinylestradiol | Estrogen | – | 0 |
| Etonogestrel | Progestin | + | 14 |
| Gestodene | Progestin | + | 27 |
| Levonorgestrel | Progestin | – | 1 |
| Medroxyprogesterone acetate | Progestin | + | 29 |
| Norethisterone | Progestin | – | 0 |
| Norgestimate | Progestin | – | 1 |
| Progesterone | Progestogen | + | 10 |
| Footnotes: a = Thrombin receptor (TR) upregulation (↑) in vascular smooth muscle cells (VSMCs). b = RBA (%) for the glucocorticoid receptor (GR). Strength: – = No effect. + = Pronounced effect. ++ = Strong effect. Miscellaenous: Direct link to table. Source:[13] | |||
Androgenic and antiandrogenic activities
Progesterone does not bind importantly to the AR, the biological target of androgens like testosterone and dihydrotestosterone (DHT), and hence does not possess any direct androgenic or antiandrogenic activity.[13][65][66] This is in contrast to many progestins, such as 19-nortestosterone derivatives (e.g., norethisterone, levonorgestrel, dienogest) and 17α-hydroxyprogesterone derivatives (e.g., cyproterone acetate, medroxyprogesterone acetate), which do bind to the AR and have been associated with androgenic or antiandrogenic effects depending on the progestin in question.[13][66]
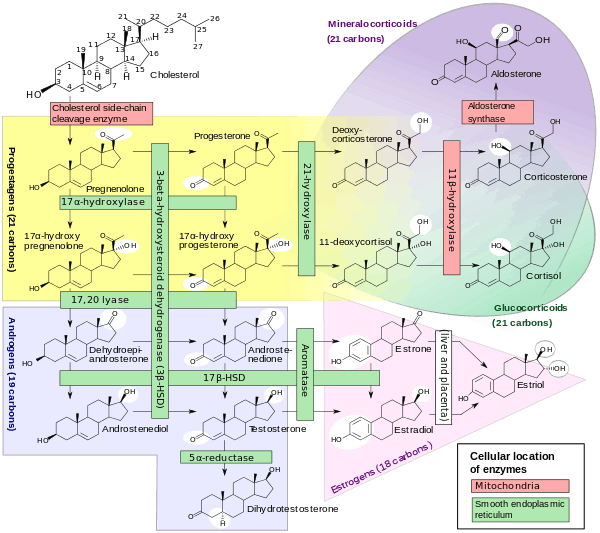
Although progesterone does not bind directly to the AR, it is a precursor and intermediate, albeit distant, in the biosynthesis of androgens from cholesterol.[67][68] For this reason, there has been some speculation that exogenous progesterone could be transformed into androgens by certain tissues that express the requisite enzymes.[68][69] Progesterone is converted by 17α-hydroxylase into 17α-hydroxyprogesterone; 17α-hydroxyprogesterone is converted by 17,20-lyase into androstenedione; and androstenedione is converted by 17β-hydroxysteroid dehydrogenases into testosterone.[67] CYP17A1, the cytochrome P450 gene that encodes 17α-hydroxylase and 17,20-lyase, is expressed mainly in the gonads (ovaries and testes) and the adrenal glands.[70] However, while it is theoretically possible that progesterone could be transformed in the body into androgens, clinical studies in which women were treated with 100 to 300 mg/day oral progesterone have found no or only a small increase in levels of 17α-hydroxyprogesterone and no change in androgen levels, including of dehydroepiandrosterone, androstenedione, and testosterone.[71][72][73] In these studies, levels of estradiol and cortisol, which progesterone is also a precursor of, did not change either, although levels of 11-deoxycorticosterone did increase significantly.[72][73] In accordance with the lack of changes in androgen levels, progesterone, unlike various progestins,[13] has not been associated with androgenic effects in clinical studies, including changes in the blood lipid profile or sex hormone-binding globulin levels,[74][71] acne, skin oiliness, hirsutism, or voice deepening, or induction of teratogenicity (i.e., virilization of female fetuses).[73][75][76]
5α-Reductase inhibition
Progesterone is a substrate for 5α-reductase, and has been found to act as a competitive inhibitor of this enzyme in vitro in a variety of studies.[13] In one study, it showed IC50 values of 1,375 nM and 88 nM (in the presence of 50 nM androstenedione as the substrate) for 5α-reductase types 1 and 2, respectively.[77] 5α-Reductase is highly expressed in skin, hair follicles, and prostate gland, and is responsible for the transformation of testosterone into the several-fold more potent androgen DHT in such tissues.[78][79] As such, it has been suggested that progesterone might possess some antiandrogenic effects via acting as a 5α-reductase inhibitor.[13] However, inhibition of 5α-reductase by progesterone is described as a weak effect that has only been demonstrated in vitro and at supraphysiological concentrations.[80][81] In accordance, physiological levels of circulating progesterone have not been found to importantly influence circulating DHT concentrations.[82][83]
Congenital 5α-reductase 2 deficiency is a rare intersex condition which is associated with ambiguous genitalia in male fetuses due to a deficiency in DHT production during genital differentiation.[79] Experimental prenatal exposure to established 5α-reductase inhibitors like finasteride has been found to produce similar feminized genital defects in male animals including rodents and monkeys.[84] In contrast, exogenous administration of progesterone to pregnant rodents has been found not to produce fetal defects in either male or female pups.[85][86][10] In addition, endogenous progesterone levels naturally increase to very high concentrations during pregnancy (e.g., 100-fold by term), yet genital defects do not occur.[87] In accordance, while total concentrations of progesterone in pregnant women at term are around 150 ng/mL (~500 nM), free or unbound and hence bioactive concentrations of progesterone are only about 3 ng/mL (~10 nM) due to the high plasma protein binding of progesterone, and these concentrations are still well below the aforementioned IC50 values for inhibition of 5α-reductase types 1 and 2.[88][89] As with endogenous progesterone during pregnancy, exogenous administration of additional progesterone during pregnancy has been found not to increase the risk of hypospadias in male infants.[90]
Although systemic progesterone does not appear to be an effective 5α-reductase inhibitor, topical progesterone may produce potent inhibition of 5α-reductase in the skin due to the very high local concentrations produced.[91][92] A study found that topical progesterone inhibited 5α-reductase in male pubic skin by more than 70% in vivo.[92]
Neurosteroid effects and fluctuations
Progesterone, through the actions of neurosteroid active metabolites such as allopregnanolone and pregnanolone, is a potent positive allosteric modulator of the GABAA receptor, the major signaling receptor of the inhibitory neurotransmitter γ-aminobutyric acid (GABA).[27] It can produce sedative, hypnotic, anxiolytic, euphoric, cognitive-, memory-, and motor-impairing, anticonvulsant, and even anesthetic effects with formation of sufficiently high concentrations of its neurosteroid metabolites and consequent GABAA receptor potentiation in the brain.[47][48][49][50] These actions and effects are characteristically similar to those of other GABAA receptor positive allosteric modulators like alcohol, barbiturates, and benzodiazepines.[50]
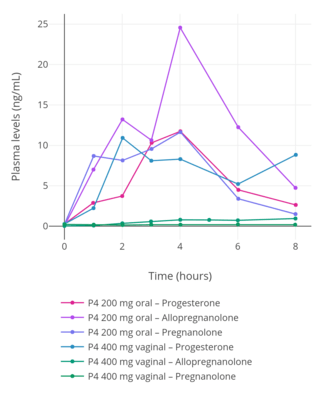
Progesterone is extensively metabolized into allopregnanolone and pregnanolone upon oral ingestion due to a large first-pass effect (80–90% or greater metabolism).[94][95][96] In accordance, with oral administration, allopregnanolone and pregnanolone circulate at higher concentrations than does progesterone.[13][93] These neurosteroid metabolites of progesterone have relatively short biological half-lives in the circulation.[97][98] Because of this, there are dramatic and highly supraphysiological spikes in allopregnanolone and pregnanolone concentrations followed by steep declines with each oral intake of progesterone.[94][95][93] As such, neurosteroid levels fluctuate substantially (e.g., 15-fold in the case of allopregnanolone) and in an unphysiological manner with oral progesterone therapy.[94][96] In addition, consumption of food with oral progesterone increases its absorption by two-fold, and this may also further amplify fluctuations in neurosteroid levels, particularly if food intake with progesterone is not consistent from dose to dose.[8]
Similarly to other GABAA receptor positive allosteric modulators like alcohol, barbiturates, and benzodiazepines, tolerance has been found to develop with exposure to increased levels of allopregnanolone and related inhibitory neurosteroids.[97][99] This includes downregulation and desensitization of the GABAA receptor, reduced effects of allopregnanolone and other GABAA receptor activators (e.g., GABA and benzodiazepines), and rebound or withdrawal effects upon falls in allopregnanolone levels.[97][99] In addition, changes in allopregnanolone levels have been implicated in adverse neuropsychiatric effects associated with the menstrual cycle (e.g., dysphoria, depression, anxiety, irritability) and postpartum period (e.g., postpartum depression), as well as in catamenial epilepsy (seizures).[100][101] Low and high levels of allopregnanolone seem to have a neutral effect on mood, whereas moderate levels have a negative effect, which may underlie the symptoms of premenstrual syndrome and premenstrual dysphoric disorder that are observed in 30 to 40% of premenopausal women.[100][101][102] This U-shaped effect on mood appears to be a common property of GABAA receptor positive allosteric modulators.[100][101]
In contrast to oral administration, parenteral progesterone, such as with vaginal administration, avoids the first-pass effect, and is not associated with supraphysiological concentrations of neurosteroid metabolites, nor with spikes or marked fluctuations in neurosteroid levels.[94] Parenteral routes can be used instead of oral administration to avoid adverse effects related to neurosteroid fluctuations if they prove to be problematic.[96][13] Lower doses of oral progesterone (e.g., 100 mg/day) are also associated with relatively reduced formation of neurosteroid metabolites, and may similarly help to alleviate such side effects.[13] In addition, the 5α-reductase inhibitor dutasteride, which blocks the production of allopregnanolone (though not of pregnanolone) from progesterone, has been found to diminish symptoms of premenstrual syndrome.[103]
Pregnenolone, an over-the-counter supplement and close analogue of progesterone, is extensively converted into neurosteroids such as allopregnanolone and pregnanolone with oral administration similarly to progesterone.[104][105][106][107] Conversely, this was not seen with transdermal administration of pregnenolone.[107]
Pharmacokinetics
The pharmacokinetics of progesterone are dependent on its route of administration. The medication is approved in the form of oil-filled capsules containing micronized progesterone for oral administration, termed "oral micronized progesterone" ("OMP") or simply "oral progesterone".[75] It is also available in the form of vaginal or rectal suppositories or pessaries, topical creams and gels,[108] oil solutions for intramuscular injection, and aqueous solutions for subcutaneous injection.[75][9][56]
Routes of administration that progesterone has been used by include oral, intranasal, transdermal/topical, vaginal, rectal, intramuscular, subcutaneous, and intravenous injection.[9] Oral progesterone has been found to be inferior to vaginal and intramuscular progesterone in terms of absorption (low) and clearance rate (rapid).[9] Vaginal progesterone is available in the forms of progesterone gel, rings, and suppositories or pessaries.[9] Advantages of intravaginal progesterone over oral administration include high bioavailability, rapid absorption, avoidance of first-pass metabolism, sustained plasma concentrations, and a local endometrial effect, while advantages of intravaginal progesterone relative to intramuscular injection include greater convenience and lack of injection site pain.[9]
Intranasal progesterone as a nasal spray has been found to be effective in achieving therapeutic levels, and was not associated with nasal irritation, but was associated with an unpleasant taste of the spray.[9] Rectal, intramuscular, and intravenous routes may be inconvenient, especially for long-term treatment.[9] Plasma levels of progesterone are similar after vaginal and rectal administration in spite of the different routes of administration, and rectal administration is an alternative to vaginal progesterone in conditions of vaginal infection, cystitis, recent childbirth, or when barrier contraception methods are used.[9] Intramuscular injection of progesterone may achieve much higher levels of progesterone than normal luteal phase concentrations and levels achieved with other routes.[9]
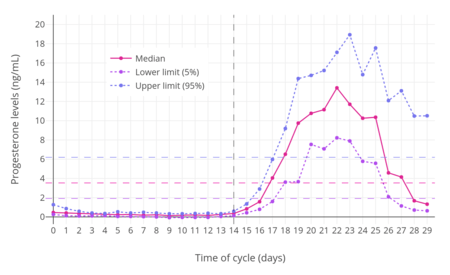
For purposes of comparison with normal physiological circumstances, luteal phase levels of progesterone are 4 to 30 ng/mL (with levels of 5 to 9 ng/mL during the mid-luteal phase), while follicular phase levels of progesterone are 0.02 to 0.9 ng/mL, menopausal levels are 0.03 to 0.3 ng/mL, and levels of progesterone in men are 0.12 to 0.3 ng/mL.[57][110] During pregnancy, levels of progesterone in the first 4 to 8 weeks are 25 to 75 ng/mL, and levels are typically around 140 to 200 ng/mL at term.[58][57] Production of progesterone in the body in late pregnancy is approximately 250 mg per day, 90% of which reaches the maternal circulation.[111]
The pharmacokinetics of progesterone have been reviewed.[13][112]
| Route | Dose | Time | P4 (levels) | Allo (levels) | Preg (levels) | Assay | Ref |
|---|---|---|---|---|---|---|---|
| Oral (in oil, micronized) | 100 mg 100 mg 100 mg 200 mg 200 mg 200 mg 300 mg 300 mg 600 mg 1,200 mg | 2.7 hours ? ? 2.2 hours ? ? 2.0 hours ? ? ? | 10.2 ng/mL 1.5–6.5 ng/mL 1.5–2.2 ng/mL 19.9 ng/mL 3.2–13.8 ng/mL 12 ng/mL 49.8 ng/mL 9.0–32.2 ng/mL 32.8 ng/mL 58.5 ng/mL | ND ND 14 ng/mL ND ND 30 ng/mL ND ND ND ND | ND ND 3.6 ng/mL ND ND 60 ng/mL ND ND ND ND | RIA ? LC–MS RIA ? RIA (+CS) RIA RIA RIA RIA | [113][8] [47][13] [13][94][1] [113][8] [47][13] [13][114] [113][8] [47][115] [47][115] [47][115] |
| Vaginal | 25 mg 50 mg 100 mg 100 mg 200 mg 400 mg | ? ? ? ? 12 hours ? | 7.3 ng/mL 8.8 ng/mL 9.5–19.0 ng/mL 5 ng/mL 5.2 ng/mL 16 ng/mL | ND ND ND 3.5 ng/mL ND 1.2 ng/mL | ND ND ND NC ND 0.3 ng/mL | ? ? ? RIA (+CS) RIA RIA (+CS) | [47][13] [47][13] [47][13][94] [13] [13][116] [13] |
| Rectal | 25 mg 100 mg 200 mg | ? ? ? | 6.4 ng/mL 22.5 ng/mL 19.3–20.3 ng/mL | ND ND ND | ND ND ND | ? ? ? | [47] [47] [47] |
| Intramuscular (in oil) | 25 mg 50 mg 100 mg 200 mg | ? ? ? ? | 16.9 ng/mL 36.5 ng/mL 81.8–83.8 ng/mL 194–270 ng/mL | ND ND ND ND | ND ND ND ND | ? ? ? ? | [47][13] [47][13] [47][13] [47][13] |
| Note that in the case of oral progesterone, RIA may overestimate levels of progesterone by as much as 8-fold due to its low specificity and cross-reactivity with high levels of progesterone metabolites.[117][118][1] LC–MS and RIA plus CS are exact methods and can be considered accurate, on the other hand.[117][118][1] | |||||||
| Group | P4 (prod) | P4 (levels) | ||
|---|---|---|---|---|
| Prepubertal children | ND | 0.06–0.5 ng/mL | ||
| Pubertal girls Tanner stage I (childhood) Tanner stage II (ages 8–12) Tanner stage III (ages 10–13) Tanner stage IV (ages 11–14) Tanner stage V (ages 12–15) Follicular phase (days 1–14) Luteal phase (days 15–28) | ND ND ND ND ND ND | 0.22 (<0.10–0.32) ng/mL 0.30 (0.10–0.51) ng/mL 0.36 (0.10–0.75) ng/mL 1.75 (<0.10–25.0) ng/mL 0.35 (0.13–0.75) ng/mL 2.0–25.0 ng/mL | ||
| Premenopausal women Follicular phase (days 1–14) Luteal phase (days 15–28) Oral contraceptive (anovulatory) | 0.75–5.4 mg/day 15–50 mg/day ND | 0.02–1.2 ng/mL 4–30 ng/mL 0.1–0.3 ng/mL | ||
| Postmenopausal women Oophorectomized women | ND 1.2 mg/day | 0.03–0.3 ng/mL 0.39 ng/mL | ||
| Pregnant women First trimester (weeks 1–12) Second trimester (weeks 13–26) Third trimester (weeks 27–40) Postpartum (at 24 hours) | ND 92 mg/daya 132–563 mg/day ND | 9–75 ng/mL 17–146 ng/mL 55–255 ng/mL 19 ng/mL | ||
| Men | 0.75 mg/day | 0.1–0.3 ng/mL | ||
| a = At 15 weeks. Mean levels are given as a single value and ranges are given after in parentheses. Sources:[10][119][35][57][110][58][120] | ||||
Oral administration
| Parameter | Oral 100 mga | Vaginal 90 mgb | ||
|---|---|---|---|---|
| LC–MS | RIA | LC–MS | RIA | |
| Cmax (ng/mL) | 2.2 | 19.4 | 10.5 | 10.5 |
| Cmax (ng/mL/mg) (DN) | 0.02 | ND | 0.12 | ND |
| Cavg(0–24) (ng/mL) | 0.14 | ND | 5.55 | ND |
| Tmax (h) | 1.0 | 1.0 | 7.7 | 7.7 |
| AUC0–24 (ng•h/mL) | 3.5 | ND | 133.3 | ND |
| AUC0–24 (ng•h/mL/mg) (DN) | 0.035 | ND | 1.5 | ND |
| DN = Dose-normalized. a = Prometrium. b = Crinone 8% gel. | ||||
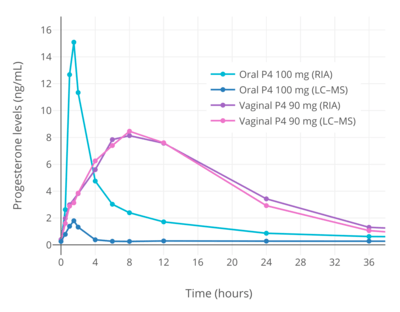
Knowledge about the pharmacokinetics of oral progesterone has been complicated by the use of flawed analytical techniques.[121][117][118] When progesterone is taken orally, due to first-pass metabolism, very high levels of its metabolites occur.[121][117][118] Most previous studies have used a method known as radioimmunoassay (RIA) to measure progesterone levels.[121][117][118] However, RIA has high cross-reactivity and is unable to differentiate between progesterone and metabolites such as allopregnanolone and pregnanolone.[121][117][118] As a result, studies that have assessed the pharmacokinetics of oral progesterone using RIA have reported falsely high progesterone levels and inaccurate dependent pharmacokinetic parameters.[121][117][118] Comparative studies using reliable and exact methods such as liquid chromatography–mass spectrometry (LC–MS) and RIA in conjunction with adequate chromatographic separation (CS) have shown that RIA overestimates levels of progesterone by 5- to 8-fold.[121][117][118] For this reason, the use of reliable assays is mandatory when studying the pharmacokinetics of oral progesterone, and an awareness of these methodological issues is likewise essential in understanding the pharmacokinetics of oral progesterone.[121][117][118] Conversely, the same issues are not applicable to parenteral routes of progesterone such as vaginal administration and intramuscular injection, because these routes are not subject to a first pass and relatively low levels of progesterone metabolites are formed.[121][117][118] Aside from the relevant methodological issues, it is also important to note that when the term "oral progesterone" is used, what is used clinically and what is almost always being referred to, unless noted otherwise, is micronized progesterone suspended in oil.[122][13][121]
The oral bioavailability of progesterone is very low.[122] Studies using RIA have generally measured the bioavailability of oral progesterone as less than 10%,[122] with one study reporting values of 6.2 to 8.6%.[113][8] However, these values are overestimations; a study using LC–MS found that the bioavailability of oral progesterone was only 2.4% relative to vaginal progesterone gel[1] (and notably not relative to the standard of progesterone by intramuscular injection, which has much higher bioavailability than vaginal progesterone).[123] The very low bioavailability of oral progesterone is due to the fact that it is poorly absorbed from the gastrointestinal tract and undergoes massive metabolism, resulting in almost complete inactivation during the first pass through the liver.[122][124] Because of its poor oral bioavailability, very high doses of progesterone must be used by the oral route to achieve significant circulating progesterone levels.[122] In addition, oral progesterone is always micronized and suspended in oil.[122][75][123][125] This improves the bioavailability of oral progesterone significantly compared to plain milled progesterone, and allows it to be used at practical doses.[122]
Micronization is the process of reducing the average diameter of the particles of a solid material.[125] By micronizing progesterone, its particles are made smaller (mainly <10 μM) and its surface area is increased, thereby enhancing absorption from the intestines.[122][125] Suspension and partial solubilization[126] of progesterone in oil containing medium- to long-chain fatty acids likewise improves the bioavailability of oral progesterone.[13][127][128] Progesterone is a lipophilic compound and it has been theorized that suspension of progesterone in oil may improve its absorption by the lymphatic system, thereby allowing a portion of oral progesterone to bypass the first pass through the liver and hence enhancing its bioavailability.[122][129][130][131] Compared to plain milled progesterone, peak levels of progesterone following a single 200 mg oral dose were increased 1.4-fold by micronization, 1.2-fold by suspension in oil, and 3.2-fold by the combination of micronization and suspension in oil.[131] Oral micronized progesterone suspended in oil is rapidly and almost completely absorbed from the intestines.[10] There is wide interindividual variability in the bioavailability of oral progesterone.[13][8] As progesterone was not used orally for many decades due to its poor bioavailability (until the introduction of oral micronized progesterone in oil-filled gelatin capsules in 1980),[123] oral progestins (synthetic progestogens) with improved metabolic stability and high oral bioavailability were developed and have been used clinically instead.[132]
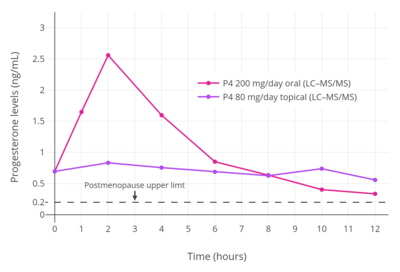
When oral progesterone is used at typical clinical dosages, only very low levels of progesterone are measured using reliable methods.[121][117][118] Following single doses of oral progesterone, peak levels of progesterone of 1.5 to 2.4 ng/mL with 100 mg and 2.8 to 4.7 ng/mL with 200 mg have been measured using LC–MS, liquid chromatography–tandem mass spectrometry (LC–MS/MS), and RIA with adequate CS.[121][133][1] In one such study, although peak levels of progesterone were 2.2 ng/mL after a single 100 mg dose of oral progesterone, levels of progesterone remained significantly elevated for less than about 4 hours, and the average progesterone levels over a period of 24 hours were only 0.14 ng/mL.[118][1] For comparison, normal progesterone levels during the luteal phase of the menstrual cycle with LC–MS/MS are 6.7 to 22.2 ng/mL.[134] When the unreliable method of standalone RIA has been used to measure progesterone levels with oral progesterone, far higher peak levels of 6.5 to 10.2 ng/mL, 13.8 to 19.9 ng/mL, and 32.3 to 49.8 ng/mL have been erroneously observed after single 100, 200, and 300 mg doses, respectively.[113][8] In addition, progesterone levels have been inaccurately measured by RIA as remaining elevated for 12 to 24 hours.[1][75] Regardless of assay method, peak levels of progesterone following a dose of oral progesterone occur after about 1 to 3 hours.[117] The elimination half-life of progesterone in the circulation is very short at a range of about 3 to 90 minutes.[10] Previous studies using RIA have reported an overestimated half-life of oral progesterone of about 16 to 18 hours.[75] A subsequent, reliable study using high-performance liquid chromatography–tandem mass spectrometry (HPLC–MS/MS) reported a half-life of oral progesterone of about 4.6 to 5.2 hours when it was taken with food.[4] Due to the short half-life and duration of action of oral progesterone, it is often taken in divided doses of two or three times per day.[75][135]
Because of studies that used RIA, it was incorrectly believed for many years that oral progesterone could easily achieve luteal phase levels of progesterone or beyond and could produce considerable progestogenic effects.[121][117][118] In actuality, the very low levels of progesterone with oral administration, as measured by reliable methods like LC–MS, appear to be insufficient for adequate and full progestogenic effects.[118][1] This is evidenced by the fact that, in contrast to almost all progestins, an increased risk of endometrial cancer has been observed when oral progesterone is combined with an estrogen in menopausal hormone therapy.[118][1] This finding indicates that typical clinical dosages of oral progesterone are insufficient for full endometrial protection.[118][1] However, in spite of the very low levels of progesterone achieved, typical clinical dosages of oral progesterone do seem to be able to adequately prevent estrogen-induced endometrial hyperplasia.[121][117] On the other hand, oral progesterone fails to produce full endometrial secretory transformation, and is considered to be inappropriate for use in assisted reproduction, whereas vaginal and intramuscular progesterone are effective.[136][137] Even very high doses of 600 mg/day oral progesterone fail to produce full luteal-phase endometrial changes,[96] although doses of 300 to 600 mg/day oral progesterone have reportedly been used for luteal support in assisted reproduction.[137]
The very low levels of progesterone achieved with oral progesterone may also explain the absence of an increase in risk of breast cancer and venous thromboembolism when oral progesterone is added to estrogen therapy in postmenopausal women.[118] Such risks are increased by progestins, which are PR agonists similarly to progesterone, but have not been found to be increased by oral progesterone.[117][118] Since typical clinical dosages of oral progesterone achieve only very low levels of progesterone, and progesterone therapy resulting in adequate progesterone levels has never been properly evaluated in sufficiently large clinical studies, it has been said that notion that progesterone somehow differs from progestins and does not increase the risk of breast cancer or venous thromboembolism are unsubstantiated.[117][118][133] Moreover, it has been said that in the absence of adequate data to the contrary, it would be reasonable to consider progesterone at least equivalent to progestins as a potential risk factor for such complications.[117][118][133] Indeed, the French E3N study did observe a significant increase in risk of breast cancer with estrogen and progesterone therapy in postmenopausal women after long-term (>5-year) administration, which is consistent with a weak proliferative effect of oral progesterone on the breasts such that a longer duration of exposure is necessary for a significant increase in breast cancer incidence to manifest.[117][118]
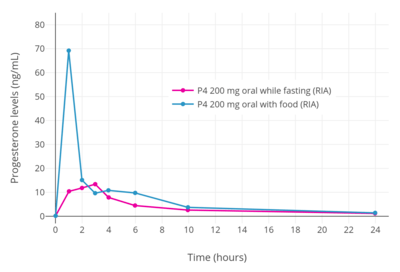
When oral progesterone is taken with food instead of taken in a fasting state, it appears that maximal levels of progesterone and its overall bioavailability may be greatly improved.[8][4] Measured with the unreliable method of RIA, peak levels of progesterone were increased by 5-fold and area-under-the-curve levels of progesterone by 2-fold when oral progesterone was taken with food.[8] In this RIA study, a single dose of 200 mg oral progesterone in fasting and fed conditions resulted in peak levels of progesterone of 13.4 ng/mL and 69.5 ng/mL, respectively, and AUC0–24 levels of progesterone of 91.5 ng/mL and 182.5 ng/mL, respectively.[8] Likewise however, a study using the reliable method of HPLC–MS/MS found that peak levels of progesterone were 69.7 to 89.2 ng/mL and AUC0–24 levels of progesterone were 111.6 to 125.9 ng/mL after a single dose of 200 mg oral progesterone with a high-fat, high-calorie meal.[4] These data, which are fairly similar, indicate that the previous findings of the RIA study may not have been fully erroneous and may in considerable part have indeed represented actual levels of progesterone rather than those of its metabolites.[8][4] On the basis of the HPLC–MS/MS study findings and previous studies using reliable methods, peak levels of progesterone when oral progesterone is taken with food may be on the order of 15- to 20-fold greater than when it is taken in a fasting state.[4][1][133] The apparent substantial improvement in progesterone levels and bioavailability when oral progesterone is taken with food may be due to enhanced lymphatic absorption, allowing oral progesterone to bypass some first-pass metabolism.[8][122][129][130] In accordance, a related steroid medication, oral testosterone undecanoate in oil-filled capsules, is absorbed by the lymphatic system but must be taken with meals that contain at least a moderate or "normal" amount of fat for adequate bioavailability.[138][139] Taking oral testosterone undecanoate with food has been found to increase peak testosterone levels by 16-fold and the overall bioavailability by 11-fold relative to when the medication is taken in a fasting state.[140][141] Although the bioavailability of oral progesterone is greatly increased if it is taken with food, its overall bioavailability is still relatively low, even if measured using RIA.[14]
Progesterone is metabolized into allopregnanolone and pregnanolone, which are neurosteroids and potent potentiators of the GABAA receptor.[48][49] The conversion of progesterone into these metabolites is catalayzed by the enzymes 5α- and 5β-reductase and 3α-hydroxysteroid dehydrogenase, and occurs primarily in the liver, but also in reproductive endocrine tissues, the skin, the brain, and other tissues.[142] Due to the first pass with oral progesterone, about 90% of progesterone is rapidly transformed into these metabolites, and massive quantities of these neurosteroids are consequently formed and circulate.[137] It is for this reason that commonly reported side effects of progesterone include dizziness, drowsiness, sedation, somnolence, and fatigue.[48][49] Both oral and sufficiently high doses of intramuscular progesterone can produce these sedative effects, indicating that first-pass metabolism in the liver is not necessarily essential for the conversion to take place.[143][144][145] However, the levels of these neurosteroids have been found to be comparatively very low with parenteral routes like vaginal and intramuscular progesterone relative to oral progesterone.[93][144] As with the bioavailability of oral progesterone, there is high interindividual variability in the formation and levels of allopregnanolone and pregnanolone with oral progesterone.[13] As a result, some individuals may experience considerable central depressant effects with oral progesterone, whereas others may experience few such effects.[13]
Buccal administration
Progesterone has been studied for use by buccal administration.[13][146]
Sublingual administration
| Route | Form | Dose | Cmax | Tmax | t1/2 |
|---|---|---|---|---|---|
| Vaginal | Tableta | 100 mg | 10.9 ng/mL | 6–7 hours | 13.7 hours |
| Vaginal | Capsule | 100 mg | 9.7 ng/mL | 1–3 hours | |
| Sublingual | Tableta | 100 mg | 13.5 ng/mL | 1–4 hours | ~6–7 hours |
| Sublingual | Suspension | 100 mg | 17.6 ng/mL | 0.5–1 hours | |
| Oral | Capsule | 200 mg | 4.3–11.7 ng/mL | 2 hours | |
| Oral | Capsule | 200 mg | 4.3 ng/mL | 2.5 hours | |
| Intramuscular | Oil | 50 mg | 14.3 ng/mL | 8.7 hours | |
| a = Luteina. | |||||
A micronized tablet formulation of progesterone marketed under the brand name Luteina is indicated for use by sublingual administration in addition to the vaginal route and is approved for use in Poland and Ukraine.[149] It is used by the sublingual route at dosages of 50 to 150 mg three to four times per day.[149][5] A single 100 mg sublingual dose of Luteina has been found to reach mean peak progesterone levels of 13.5 ng/mL after 1 to 4 hours, with an elimination half-life of about 6 to 7 hours.[149][5]
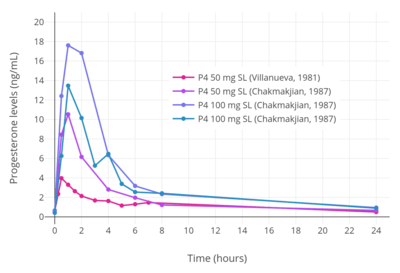
A number of other studies have also investigated the use of progesterone by sublingual administration.[150][151][147][148] Older studies have also explored sublingual progesterone.[152][153][154] A study of sublingual progesterone for luteal support in patients undergoing embryo transfer found that after sublingual administration of 50 or 100 mg progesterone dissolved in a 1 mL suspension, peak levels of progesterone were reached in 30 to 60 minutes and were on average 17.61 ± 3.78 ng/mL with the 100-mg dose.[150][151] However, the duration was short, with levels of less than 5 ng/mL at 6 hours, and re-administration had to be done two or three times per day for adequate circulating levels of progesterone to be maintained throughout the day.[150][151] Another study found that sublingual progesterone had to be administered at a dose of 400 mg every 8 hours to achieve circulating levels similar to those produced by 100 mg/day intramuscular progesterone.[150] One study administered 400 mg sublingual progesterone three times per day and achieved mean progesterone levels of 57.8 ± 37.4 ng/mL, which were similar to those produced by 50 mg/day intramuscular progesterone.[151]
Intranasal administration
Progesterone has been evaluated by the intranasal route, in the form of a nasal spray, in one study.[150][13][155]
Transdermal administration
Progesterone for transdermal or topical administration is not approved by the FDA in the United States but is available from custom compounding pharmacies and is also notably available over-the-counter without a prescription in this country.[156][157][133] It is available from these sources in the form of creams and gels.[156][157] Topical progesterone has been used as a component of menopausal hormone therapy to treat thousands of women in the United States and Europe.[156] However, these products are unregulated and have not been clinically tested, often with little being known about their pharmacokinetics.[156] Moreover, the effectiveness of topical progesterone for systemic therapy, as in menopausal hormone therapy, is controversial.[156][157] Clinical studies have found only very low levels (<3.5 ng/mL) of progesterone in circulation with the use of topical progesterone, and these levels are thought to be insufficient to confer endometrial protection from unopposed estrogen.[156][157] The range of circulating levels of progesterone that has been observed in clinical studies with various preparations and doses of transdermal progesterone is 0.38 to 3.5 ng/mL.[123][156]
Although very low levels of progesterone have been observed in venous blood, very high and in fact greatly supraphysiological levels of progesterone have been found in saliva and capillary blood with topical progesterone.[156][157][158] In one study, the levels of progesterone in saliva and capillary blood were 10- and 100-fold greater than levels in venous blood, respectively.[156][157][158] Levels of salivary progesterone that have been observed in clinical studies with transdermal progesterone have ranged from 2.9 to 2,840 ng/mL.[123] Findings of high salivary and capillary blood levels of progesterone suggest that in spite of the fact that progesterone levels in circulation remain low, and for reasons that are poorly understood, systemic distribution with topically administered progesterone may be occurring somehow and there may be substantial exposure of some tissues, such as the endometrium, to the hormone.[156][157][158] However, the few clinical studies that have assessed the effects of topical progesterone on the endometrium have had mixed findings, and further research is needed to determine whether topical progesterone can confer adequate endometrial protection in menopausal hormone therapy.[156][157]
Topical progesterone is usually supplied in the form of creams and water-based gels, and the studies in which very low levels of progesterone in circulation were observed with topical progesterone used these formulations.[156][157] However, a study of topical progesterone in the form of an alcohol-based gel found relatively high concentrations of progesterone in circulation that corresponded to luteal phase levels, and were theoretically sufficient to confer endometrial protection.[156][157]
A study that investigated the pharmacokinetics of topical progesterone using a hydrophilic (gel), lipophilic, or emulsion-type base found that in all three cases the time to peak concentrations was around 4 hours and the elimination half-life was in the range of 30 to 40 hours.[7] The venous blood levels observed were very low.[7]
Because progesterone is a lipophilic and hydrophobic compound, it is not absorbed efficiently by the skin.[14][150] Moreover, because the body produces about 25 mg progesterone per day on average during the luteal phase, around 50% of the body would need to be used as a surface of absorption to deliver a similar quantity of progesterone.[14][150] As such, the transdermal route cannot easily achieve adequate circulating progesterone levels, and this makes transdermal progesterone impractical for systemic therapy.[14][150]
Topical application of progesterone with the intention of systemic therapy should not be equated with local treatment.[123] Despite the fact that it is not approved for use in menopausal hormone therapy, topical progesterone is registered in some countries under the brand name Progestogel as a 1% gel for direct local application to the breasts to treat premenstrual mastodynia (breast pain).[159][123] It has been found in clinical studies to inhibit estrogen-induced proliferation of breast epithelial cells and to abolish breast pain and tenderness in women with the condition.[123] The effectiveness of topical progesterone for this indication may be related in part to the fact that the site of application of topical progesterone has been found to significantly influence its absorption.[157] A study observed a significant increase in serum levels of progesterone when it was applied as a topical ointment to the breasts but not when it was applied to other areas like the thigh or abdomen.[157]
Some unregulated topical progesterone products contain "wild yam extract" derived from Dioscorea villosa, but there is no evidence that the human body can convert its active ingredient (diosgenin, the plant steroid that is chemically converted to produce progesterone industrially)[160] into progesterone.[161][162]
Vaginal administration
Progesterone for vaginal administration is available in the form of a gel or insert (suppository). With vaginal administration, a 100 mg dose of progesterone results in peak levels at 4 hours and 8 hours after dosing, respectively, with the levels achieved being in the luteal phase range.[110] Following peak levels, there is a gradual decline in circulating concentrations, and after 24 hours, levels typical of the follicular phase are reached.[110] The bioavailability of vaginal progesterone is about 40-fold greater than that of oral progesterone.[163][1] There is a uterine first-pass effect with vaginal progesterone, such that progesterone levels are far greater in the uterus than in the circulation.[123]
Rectal administration
Progesterone can be taken by rectal administration.[47][14][110] A suppository sold under the brand name Cyclogest is indicated for rectal use in addition to the vaginal route.[125][164][165] Daily rectal administration of progesterone is inconvenient and poorly accepted for long-term therapy.[113][47] Nonetheless, rectal progesterone can be a useful alternative to the vaginal route in the context of vaginal infection, cystitis, recent childbirth, or when barrier contraception methods are used.[47]
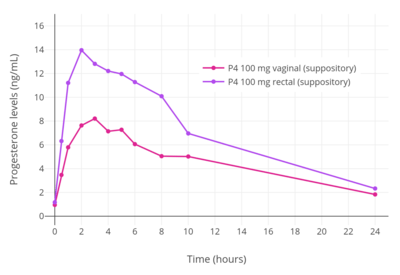
A number of studies have assessed progesterone by the rectal route.[166][167][168][169][170][155] Levels of progesterone following rectal administration have been found to be 6.4 ng/mL after a single 25 mg suppository, 22.5 ng/mL after a single 100 mg suppository, and 19.4 to 20.3 ng/mL after a single 200 mg suppository.[47] The absorption of the rectal route is variable, with a wide range of maximal concentrations of 15 to 52 ng/mL progesterone after a single rectal dose of 100 mg progesterone.[14][168] Levels of progesterone peak after 6 to 8 hours and then gradually decrease.[14][47] Progesterone levels have been found to be similar and non-significantly different after administration of rectal and vaginal suppositories in several studies.[47]
Progesterone is delivered directly into the circulation when it is absorbed by the lower portion of the rectum and transported by the inferior and middle rectal veins.[14] Conversely, if it is absorbed by the upper portion of the rectum, progesterone is subject to hepatic first-pass metabolism due to entry into the hepatic portal system via the superior rectal vein.[14] As such, although rectal administration is a parenteral route, it can still be subject to some first-pass metabolism similarly to oral progesterone.[14]
Intramuscular injection
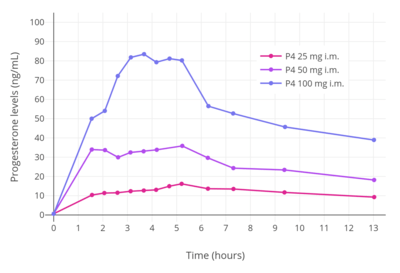
When used by intramuscular injection, progesterone bypasses first-pass metabolism in the intestines and liver and achieves very high circulating progesterone levels.[13][123] Levels of progesterone with 100 mg/day intramuscular progesterone were substantially higher than with 800 mg/day vaginal progesterone (about 70 ng/mL and 12 ng/mL, respectively), although local progesterone levels in the uterus were 10 times higher with the vaginal route due to a uterine first-pass effect (around 1.5 ng/mL and almost 12 ng/mL, respectively).[123] The duration of progesterone is extended by the intramuscular route due to a depot effect in which it is stored locally in adipose tissue, and can be administered once every 1 to 3 days.[14] The half-life of intramuscular progesterone is significantly longer when it is injected into the gluteal muscles of the buttocks rather than the deltoid muscle of the upper arm.[14] Intramuscular progesterone has traditionally been the most popular form of progesterone used for luteal support in assisted reproduction in the United States, although vaginal progesterone is also used and effective.[123][14]
With intramuscular injection of 10 mg progesterone in vegetable oil, maximum plasma concentrations (Cmax) are reached at approximately 8 hours after administration, and serum levels remain above baseline for about 24 hours.[56] Doses of 10, 25, and 50 mg via intramuscular injection have been found to result in average maximal concentrations of 7, 28, and 50 ng/mL, respectively.[56] With intramuscular injection, a dose of 25 mg results in normal luteal phase serum levels of progesterone within 8 hours, and a 100 mg dose produces mid-pregnancy levels of 40 to 80 ng/mL at peak.[110] At these doses, levels of progesterone remain elevated above baseline for at least 48 hours (6 ng/mL at this point for 100 mg),[110] with an elimination half-life of about 22 hours.[9]
Due to the high concentrations achieved, progesterone by intramuscular injection at the usual clinical dose range is able to suppress gonadotropin secretion from the pituitary gland, demonstrating antigonadotropic efficacy (and therefore suppression of gonadal sex steroid production).[56]
Intramuscular progesterone often causes pain when injected.[14] It irritates tissues and is associated with injection site reactions such as changes in skin color, pain, redness, transient indurations (due to inflammation), ecchymosis (bruising/discoloration), and others.[171][14] Rarely, sterile abscesses can occur.[14]
An intramuscular suspension formulation of progesterone contained in microspheres is marketed under the brand name ProSphere in Mexico.[171][172][173] It is far longer-lasting than regular intramuscular progesterone and is administered once weekly or once monthly, depending on the indication.[171]
Subcutaneous injection
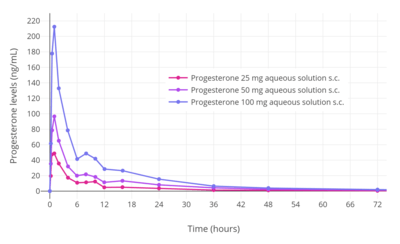
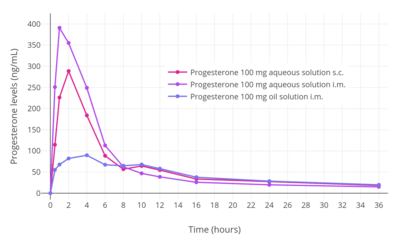
Progesterone can also be administered alternatively via subcutaneous injection, with the aqueous formulation Prolutex in Europe being intended specifically for once-daily administration by this route.[9][174][175] This formulation is rapidly absorbed and has been found to result in higher serum peak progesterone levels relative to intramuscular oil formulations.[175] In addition, subcutaneous injection of progesterone is considered to be easier, safer (less risk of injection site reactions), and less painful relative to intramuscular injection.[175] The elimination half-life of this formulation is 13 to 18 hours,[9] compared to 20 to 28 hours for intramuscular injection in oil.[8][6][9]
| Parameter | Subcutaneous injection (aq.)a | Intramuscular injection | |||
|---|---|---|---|---|---|
| 25 mg | 50 mg | 100 mg | 100 mg (aq.)a | 100 mg (oil) | |
| Cmax (ng/mL) | 57.8 | 103 | 235–300 | 440 | 113 |
| Tmax (hours) | 0.92 | 0.92 | 0.92 | 0.88 | 6.7 |
| AUC0–t (ng/mL/h) | 338 | 729 | 1466–1856 | 1902 | 2049 |
| AUC0–∞ (ng/mL/h) | 349 | 746 | 1490–1885 | 1919 | 2097 |
| t1/2 (hours) | 13.1 | 17.2 | 17.2–17.6 | 14.3 | 22.3 |
| a = Progesterone complexed with β-cyclodextrin (Prolutex) to increase its water solubility.[9] | |||||
Intrauterine administration
A one-year progesterone intrauterine device (IUD) for hormonal birth control was previously available in the United States and a few other countries under the brand name Progestasert.[176][177] It was marketed between 1976 and 2001.[176] The IUD was never widely used due to a relatively high contraceptive failure rate of 2.9% and the requirement of annual replacement.[176] It contained 38 mg progesterone and released 65 μg progesterone into the uterus per day (adding up to about 35 mg after one year).[176][177] For comparison, a woman's body produces on average about 25 mg progesterone per day during the luteal phase.[14][150] While effective as a form of contraception and for decreasing menstrual bleeding and discomfort, long-lived IUDs can fundamentally only deliver small amounts of progesterone per day, and hence intrauterine progesterone cannot achieve adequate circulating progesterone levels and is unsuitable as a form of systemic therapy.[150]
General (ADME)
Distribution
Progesterone crosses the blood–brain barrier.[178] In terms of plasma protein binding, progesterone is 98 to 99% protein-bound in the circulation.[2][3] It is bound 80% to albumin, 18% to corticosteroid-binding globulin, and less than 1% to sex hormone-binding globulin, with the remaining fraction of 1 to 2% circulating freely or unbound.[2][3]
Metabolism
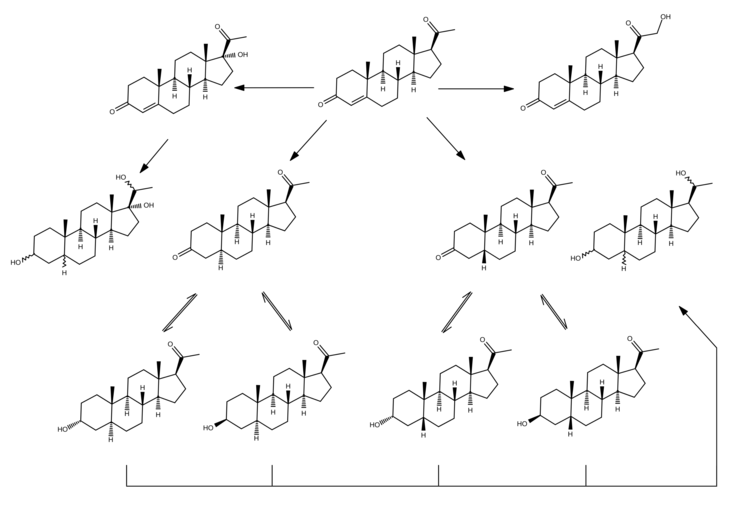
With oral administration, progesterone is rapidly metabolized in the gastrointestinal tract and liver.[159] As many as 30 different metabolites have been found to be formed from progesterone with oral ingestion.[159] Regardless of the route of administration, 5α-reductase is the major enzyme involved in the metabolism of progesterone and is responsible for approximately 60 to 65% of its metabolism.[94] 5β-Reductase is also a major enzyme in the metabolism of progesterone.[94] 5α-Reduction of progesterone occurs predominantly in the intestines (specifically the duodenum), whereas 5β-reduction occurs almost exclusively in the liver.[94] The metabolites of progesterone produced by 5α-reductase and 5β-reductase (after further transformation by 3α-hydroxysteroid dehydrogenase) are allopregnanolone and pregnanolone, respectively.[159] With oral administration of progesterone, they occur in circulation at very high and in fact supraphysiological concentrations that are well in excess of those of progesterone itself (peak concentrations of 30 ng/mL for allopregnanolone and 60 ng/mL for pregnanolone versus 12 ng/mL for progesterone at 4 hours after a single 200-mg oral dose of progesterone).[159]
The percentage constitutions of progesterone and its metabolites as reflected in serum levels have been determined for a single 100 mg dose of oral or vaginal progesterone.[96] With oral administration, progesterone accounts for less than 20% of the dose in circulation while 5α- and 5β-reduced products like allopregnanolone and pregnanolone account for around 80%.[96] With vaginal administration, progesterone accounts for around 50% of the dose and 5α- and 5β-reduced metabolites for around 40%.[96]
A small amount of progesterone is converted by 21-hydroxylase into 11-deoxycorticosterone.[62][94] Increases in levels of 11-deoxycorticosterone are markedly higher when progesterone is given orally as opposed to via parenteral routes like vaginal or intramuscular injection.[94] The conversion of progesterone into 11-deoxycorticosterone occurs in the intestines (specifically the duodenum) and in the kidneys.[62][94] 21-Hydroxylase appears to be absent in the liver, so conversion of progesterone into 11-deoxycorticosterone is thought not to occur in this part of the body.[94]
The biological half-life of progesterone in the circulation is very short; with intravenous injection, its half-life has ranged widely from 3 to 90 minutes in various studies.[10] The metabolic clearance rate of progesterone ranges between 2,100 and 2,800 L/day, and is constant across the menstrual cycle.[10][179]
Elimination
Progesterone is eliminated in bile and urine.[11][12]
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Levine H, Watson N (March 2000). "Comparison of the pharmacokinetics of Crinone 8% administered vaginally versus Prometrium administered orally in postmenopausal women(3)". Fertil. Steril. 73 (3): 516–21. doi:10.1016/S0015-0282(99)00553-1. PMID 10689005.
- 1 2 3 Fritz MA, Speroff L (28 March 2012). Clinical Gynecologic Endocrinology and Infertility. Lippincott Williams & Wilkins. pp. 44–. ISBN 978-1-4511-4847-3.
- 1 2 3 Marshall WJ, Marshall WJ, Bangert SK (2008). Clinical Chemistry. Elsevier Health Sciences. pp. 192–. ISBN 0-7234-3455-7.
- 1 2 3 4 5 6 7 8 Pickar JH, Bon C, Amadio JM, Mirkin S, Bernick B (December 2015). "Pharmacokinetics of the first combination 17β-estradiol/progesterone capsule in clinical development for menopausal hormone therapy". Menopause. 22 (12): 1308–16. doi:10.1097/GME.0000000000000467. PMC 4666011. PMID 25944519.
- 1 2 3 4 5 Хомяк, Н. В., Мамчур, В. И., & Хомяк, Е. В. (2014). Клинико-фармакологические особенности современных лекарственных форм микронизированного прогестерона, применяющихся во время беременности. Здоровье, (4), 90. http://health-ua.com/wp-content/uploads/2015/09/MAZG2-2015_28-35.pdf
- 1 2 3 http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/020701s026lbl.pdf
- 1 2 3 Mircioiu C, Perju A, Griu E, Calin G, Neagu A, Enachescu D, Miron DS (1998). "Pharmacokinetics of progesterone in postmenopausal women: 2. Pharmacokinetics following percutaneous administration". Eur J Drug Metab Pharmacokinet. 23 (3): 397–402. PMID 9842983.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Simon JA, Robinson DE, Andrews MC, Hildebrand JR, Rocci ML, Blake RE, Hodgen GD (1993). "The absorption of oral micronized progesterone: the effect of food, dose proportionality, and comparison with intramuscular progesterone". Fertil. Steril. 60 (1): 26–33. doi:10.1016/S0015-0282(16)56031-2. PMID 8513955.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Cometti B (November 2015). "Pharmaceutical and clinical development of a novel progesterone formulation". Acta Obstetricia et Gynecologica Scandinavica. 94 Suppl 161: 28–37. doi:10.1111/aogs.12765. PMID 26342177.
The administration of progesterone in injectable or vaginal form is more efficient than by the oral route, since it avoids the metabolic losses of progesterone encountered with oral administration resulting from the hepatic first-pass effect (32). In addition, the injectable forms avoid the need for higher doses that cause a fairly large number of side-effects, such as somnolence, sedation, anxiety, irritability and depression (33).
- 1 2 3 4 5 6 7 8 9 10 11 12 Aufrère MB, Benson H (June 1976). "Progesterone: an overview and recent advances". J Pharm Sci. 65 (6): 783–800. doi:10.1002/jps.2600650602. PMID 945344.
- 1 2 http://www.accessdata.fda.gov/drugsatfda_docs/label/1998/20843lbl.pdf
- 1 2 http://www.accessdata.fda.gov/drugsatfda_docs/label/2007/017362s104lbl.pdf
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61 62 Kuhl H (2005). "Pharmacology of estrogens and progestogens: influence of different routes of administration" (PDF). Climacteric. 8 Suppl 1: 3–63. doi:10.1080/13697130500148875. PMID 16112947.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Unfer, Vittorio; di Renzo, Gian; Gerli, Sandro; Casini, Maria (2006). "The Use of Progesterone in Clinical Practice: Evaluation of its Efficacy in Diverse Indications Using Different Routes of Administration". Current Drug Therapy. 1 (2): 211–219. doi:10.2174/157488506776930923. ISSN 1574-8855.
- ↑ Whitaker, Amy; Gilliam, Melissa (2014). Contraception for Adolescent and Young Adult Women. Springer. p. 98. ISBN 9781461465799.
- ↑ Chaudhuri (2007). Practice Of Fertility Control: A Comprehensive Manual (7Th Edition). Elsevier India. pp. 153–. ISBN 978-81-312-1150-2.
- ↑ Attardi BJ, Burgenson J, Hild SA, Reel JR (March 2004). "In vitro antiprogestational/antiglucocorticoid activity and progestin and glucocorticoid receptor binding of the putative metabolites and synthetic derivatives of CDB-2914, CDB-4124, and mifepristone". J. Steroid Biochem. Mol. Biol. 88 (3): 277–88. doi:10.1016/j.jsbmb.2003.12.004. PMID 15120421.
- ↑ Soltysik K, Czekaj P (April 2013). "Membrane estrogen receptors - is it an alternative way of estrogen action?". J. Physiol. Pharmacol. 64 (2): 129–42. PMID 23756388.
- ↑ Prossnitz ER, Barton M (May 2014). "Estrogen biology: New insights into GPER function and clinical opportunities". Mol. Cell. Endocrinol. 389 (1–2): 71–83. doi:10.1016/j.mce.2014.02.002. PMC 4040308. PMID 24530924.
- 1 2 3 Rupprecht R, Reul JM, van Steensel B, Spengler D, Söder M, Berning B, Holsboer F, Damm K (October 1993). "Pharmacological and functional characterization of human mineralocorticoid and glucocorticoid receptor ligands". European Journal of Pharmacology. 247 (2): 145–54. doi:10.1016/0922-4106(93)90072-H. PMID 8282004.
- 1 2 3 Elger W, Beier S, Pollow K, Garfield R, Shi SQ, Hillisch A (2003). "Conception and pharmacodynamic profile of drospirenone". Steroids. 68 (10–13): 891–905. doi:10.1016/j.steroids.2003.08.008. PMID 14667981.
- 1 2 Attardi BJ, Zeleznik A, Simhan H, Chiao JP, Mattison DR, Caritis SN (2007). "Comparison of progesterone and glucocorticoid receptor binding and stimulation of gene expression by progesterone, 17-alpha hydroxyprogesterone caproate, and related progestins". Am. J. Obstet. Gynecol. 197 (6): 599.e1–7. doi:10.1016/j.ajog.2007.05.024. PMC 2278032. PMID 18060946.
- 1 2 Lei K, Chen L, Georgiou EX, Sooranna SR, Khanjani S, Brosens JJ, Bennett PR, Johnson MR (2012). "Progesterone acts via the nuclear glucocorticoid receptor to suppress IL-1β-induced COX-2 expression in human term myometrial cells". PLoS One. 7 (11): e50167. Bibcode:2012PLoSO...750167L. doi:10.1371/journal.pone.0050167. PMID 23209664.
- 1 2 Baulieu E, Schumacher M (2000). "Progesterone as a neuroactive neurosteroid, with special reference to the effect of progesterone on myelination". Steroids. 65 (10–11): 605–12. doi:10.1016/s0039-128x(00)00173-2. PMID 11108866.
- ↑ Maurice T, Urani A, Phan VL, Romieu P (November 2001). "The interaction between neuroactive steroids and the sigma1 receptor function: behavioral consequences and therapeutic opportunities". Brain Research. Brain Research Reviews. 37 (1–3): 116–32. doi:10.1016/s0165-0173(01)00112-6. PMID 11744080.
- ↑ Johannessen M, Fontanilla D, Mavlyutov T, Ruoho AE, Jackson MB (February 2011). "Antagonist action of progesterone at σ-receptors in the modulation of voltage-gated sodium channels". American Journal of Physiology. Cell Physiology. 300 (2): C328–37. doi:10.1152/ajpcell.00383.2010. PMC 3043630. PMID 21084640.
- 1 2 Paul SM, Purdy RH (March 1992). "Neuroactive steroids". FASEB Journal. 6 (6): 2311–22. PMID 1347506.
- ↑ Karl Knörr; Fritz K. Beller; Christian Lauritzen (17 April 2013). Lehrbuch der Gynäkologie. Springer-Verlag. pp. 214–. ISBN 978-3-662-00942-0.
- ↑ Karl Knörr; Henriette Knörr-Gärtner; Fritz K. Beller; Christian Lauritzen (8 March 2013). Geburtshilfe und Gynäkologie: Physiologie und Pathologie der Reproduktion. Springer-Verlag. pp. 583–. ISBN 978-3-642-95583-9.
- ↑ Sang GW (April 1994). "Pharmacodynamic effects of once-a-month combined injectable contraceptives". Contraception. 49 (4): 361–85. doi:10.1016/0010-7824(94)90033-7. PMID 8013220.
- ↑ Toppozada MK (April 1994). "Existing once-a-month combined injectable contraceptives". Contraception. 49 (4): 293–301. doi:10.1016/0010-7824(94)90029-9. PMID 8013216.
- ↑ Bagade O, Pawar V, Patel R, Patel B, Awasarkar V, Diwate S (2014). "Increasing use of long-acting reversible contraception: safe, reliable, and cost-effective birth control" (PDF). World J Pharm Pharm Sci. 3 (10): 364–392. ISSN 2278-4357.
- 1 2 3 P. J. Bentley (1980). Endocrine Pharmacology: Physiological Basis and Therapeutic Applications. CUP Archive. pp. 264, 274. ISBN 978-0-521-22673-8.
- ↑ Sue Macdonald; Gail Johnson (3 June 2017). Mayes' Midwifery E-Book. Elsevier Health Sciences. pp. 391–. ISBN 978-0-7020-6336-7.
- 1 2 Kenneth L. Becker (2001). Principles and Practice of Endocrinology and Metabolism. Lippincott Williams & Wilkins. pp. 889, 940. ISBN 978-0-7817-1750-2.
- ↑ Lee-Ellen C. Copstead-Kirkhorn; Jacquelyn L. Banasik (25 June 2014). Pathophysiology - E-Book. Elsevier Health Sciences. pp. 660–. ISBN 978-0-323-29317-4.
Throughout the reproductive years, some women note swelling of the breast around the latter part of each menstrual cycle before the onset of menstruation. The water retention and subsequent swelling of breast tissue during this phase of the menstrual cycle are thought to be due to high levels of circulating progesterone stimulating the secretory cells of the breast.12
- ↑ Farage MA, Neill S, MacLean AB (2009). "Physiological changes associated with the menstrual cycle: a review". Obstet Gynecol Surv. 64 (1): 58–72. doi:10.1097/OGX.0b013e3181932a37. PMID 19099613.
- ↑ Raine-Fenning NJ, Brincat MP, Muscat-Baron Y (2003). "Skin aging and menopause : implications for treatment". Am J Clin Dermatol. 4 (6): 371–8. doi:10.2165/00128071-200304060-00001. PMID 12762829.
- ↑ Holzer G, Riegler E, Hönigsmann H, Farokhnia S, Schmidt JB, Schmidt B (2005). "Effects and side-effects of 2% progesterone cream on the skin of peri- and postmenopausal women: results from a double-blind, vehicle-controlled, randomized study". Br. J. Dermatol. 153 (3): 626–34. doi:10.1111/j.1365-2133.2005.06685.x. PMID 16120154.
- ↑ Charles R. B. Beckmann; William Herbert; Douglas Laube; Frank Ling, Roger Smith (21 January 2013). Obstetrics and Gynecology. Lippincott Williams & Wilkins. pp. 342–. ISBN 978-1-4698-2604-2.
- ↑ Shanafelt TD, Barton DL, Adjei AA, Loprinzi CL (2002). "Pathophysiology and treatment of hot flashes". Mayo Clin. Proc. 77 (11): 1207–18. doi:10.4065/77.11.1207. PMID 12440557.
- ↑ Sassarini J, Lumsden MA (2010). "Hot flushes: are there effective alternatives to estrogen?". Menopause Int. 16 (2): 81–8. doi:10.1258/mi.2010.010007. PMID 20729500.
- ↑ Bayliss DA, Millhorn DE (1992). "Central neural mechanisms of progesterone action: application to the respiratory system". J. Appl. Physiol. 73 (2): 393–404. PMID 1399957.
- ↑ Ghada Bourjeily; Karen Rosene-Montella (21 April 2009). Pulmonary Problems in Pregnancy. Springer Science & Business Media. pp. 21–. ISBN 978-1-59745-445-2.
- ↑ Gompel A, Plu-Bureau G (August 2018). "Progesterone, progestins and the breast in menopause treatment". Climacteric. 21 (4): 326–332. doi:10.1080/13697137.2018.1476483. PMID 29852797.
- 1 2 Oelkers W (2000). "Drospirenone--a new progestogen with antimineralocorticoid activity, resembling natural progesterone". Eur J Contracept Reprod Health Care. 5 Suppl 3: 17–24. PMID 11246598.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 Goletiani NV, Keith DR, Gorsky SJ (2007). "Progesterone: review of safety for clinical studies" (PDF). Exp Clin Psychopharmacol. 15 (5): 427–44. doi:10.1037/1064-1297.15.5.427. PMID 17924777.
- 1 2 3 4 Wang-Cheng R, Neuner JM, Barnabei VM (2007). Menopause. ACP Press. p. 97. ISBN 978-1-930513-83-9.
- 1 2 3 4 Bergemann N, Ariecher-Rössler A (27 December 2005). Estrogen Effects in Psychiatric Disorders. Springer Science & Business Media. p. 179. ISBN 978-3-211-27063-9.
- 1 2 3 Bäckström T, Bixo M, Johansson M, Nyberg S, Ossewaarde L, Ragagnin G, Savic I, Strömberg J, Timby E, van Broekhoven F, van Wingen G (2014). "Allopregnanolone and mood disorders". Prog. Neurobiol. 113: 88–94. doi:10.1016/j.pneurobio.2013.07.005. PMID 23978486.
- 1 2 Pasqualini JR (2007). "Progestins and breast cancer". Gynecol. Endocrinol. 23 Suppl 1: 32–41. doi:10.1080/09513590701585003. PMID 17943537.
- 1 2 Pasqualini JR (2009). "Breast cancer and steroid metabolizing enzymes: the role of progestogens". Maturitas. 65 Suppl 1: S17–21. doi:10.1016/j.maturitas.2009.11.006. PMID 19962254.
- 1 2 3 4 de Lignières B, Silberstein S (April 2000). "Pharmacodynamics of oestrogens and progestogens". Cephalalgia : an International Journal of Headache. 20 (3): 200–7. doi:10.1046/j.1468-2982.2000.00042.x. PMID 10997774.
- ↑ Endrikat J, Gerlinger C, Richard S, Rosenbaum P, Düsterberg B (2011). "Ovulation inhibition doses of progestins: a systematic review of the available literature and of marketed preparations worldwide". Contraception. 84 (6): 549–57. doi:10.1016/j.contraception.2011.04.009. PMID 22078182.
- ↑ Tollan A, Oian P, Kjeldsen SE, Eide I, Maltau JM (1993). "Progesterone reduces sympathetic tone without changing blood pressure or fluid balance in men". Gynecol. Obstet. Invest. 36 (4): 234–8. doi:10.1159/000292636. PMID 8300009.
- 1 2 3 4 5 Progesterone - Drugs.com, retrieved 2015-08-23
- 1 2 3 4 Josimovich J (11 November 2013). Gynecologic Endocrinology. Springer Science & Business Media. pp. 9, 25–29, 139. ISBN 978-1-4613-2157-6.
- 1 2 3 Jerome Frank Strauss; Robert L. Barbieri (2009). Yen and Jaffe's Reproductive Endocrinology: Physiology, Pathophysiology, and Clinical Management. Elsevier Health Sciences. pp. 807–. ISBN 1-4160-4907-X.
- ↑ Brady BM, Anderson RA, Kinniburgh D, Baird DT (2003). "Demonstration of progesterone receptor-mediated gonadotrophin suppression in the human male". Clin. Endocrinol. (Oxf). 58 (4): 506–12. PMID 12641635.
- ↑ Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA (25 August 2011). Campbell-Walsh Urology: Expert Consult Premium Edition: Enhanced Online Features and Print, 4-Volume Set. Elsevier Health Sciences. pp. 2938–. ISBN 978-1-4160-6911-9.
- ↑ Kjeld JM, Puah CM, Kaufman B, Loizou S, Vlotides J, Gwee HM, Kahn F, Sood R, Joplin GF (1979). "Effects of norgestrel and ethinyloestradiol ingestion on serum levels of sex hormones and gonadotrophins in men". Clinical Endocrinology. 11 (5): 497–504. doi:10.1111/j.1365-2265.1979.tb03102.x. PMID 519881.
- 1 2 3 4 5 Simon JA (December 1995). "Micronized progesterone: vaginal and oral uses". Clinical Obstetrics and Gynecology. 38 (4): 902–14. doi:10.1097/00003081-199538040-00024. PMID 8616985.
- ↑ Zerr-Fouineau M, Chataigneau M, Blot C, Schini-Kerth VB (January 2007). "Progestins overcome inhibition of platelet aggregation by endothelial cells by down-regulating endothelial NO synthase via glucocorticoid receptors". FASEB J. 21 (1): 265–73. doi:10.1096/fj.06-6840com. PMID 17116740.
- 1 2 3 Fuhrmann U, Krattenmacher R, Slater EP, Fritzemeier KH (October 1996). "The novel progestin drospirenone and its natural counterpart progesterone: biochemical profile and antiandrogenic potential". Contraception. 54 (4): 243–51. PMID 8922878.
Drospirenone and progesterone exhibited low binding affinities to the rat GR as is documented by 1% and 11% RBA values compared to the reference dexamethasone, respectively. Similar results were reported elsewhere.8 In accordance with the low affinity to the GR, progesterone and drospirenone showed weak or no detectable agonistic activities, respectively, in the GR-dependent transactivation assay (Figure 2A and Figure 2B). Furthermore, both progestins were devoid of antiglucocorticoid activity in vitro. These data are in agreement with in vivo studies carried out with rats where drospirenone and progesterone showed neither glucocorticoid nor antiglucocorticoid activity.8
- ↑ Sitruk-Ware R (2002). "Progestogens in hormonal replacement therapy: new molecules, risks, and benefits". Menopause. 9 (1): 6–15. PMID 11791081.
- 1 2 Sumino, Hiroyuki; Ichikawa, Shuichi; Kasama, Shu; Takahashi, Takashi; Kumakura, Hisao; Takayama, Yoshiaki; Minami, Kazutomo; Kanda, Tsugiyasu; Kurabayashi, Masahiko; Murakami, Masami (2011). "Hormone Therapy and Blood Pressure in Postmenopausal Women". Journal of Experimental & Clinical Medicine. 3 (3): 112–115. doi:10.1016/j.jecm.2011.04.005. ISSN 1878-3317.
Natural progesterone, such as micronized progesterone, has no androgenic properties, whereas some synthetic progestins, such as MPA and norethisterone acetate, possess androgenic side effects, which raise the concern of potentially harmful effects on blood pressure.
- 1 2 3 Häggström, Mikael; Richfield, David (2014). "Diagram of the pathways of human steroidogenesis". WikiJournal of Medicine. 1 (1). doi:10.15347/wjm/2014.005. ISSN 2002-4436.
- 1 2 Samuel B. Frank (1971). Acne Vulgaris. Thomas. p. 131.
The chemical structure of progesterone and testosterone are remarkably similar; they differ only in the side chain at the 17-carbon position. The possibility that progesterone can be transformed to testosterone has been considered good by many. If true, it could then be a source of androgens in women. [...] Laboratory evidence exists that progesterone can be converted to testosterone in vitro by human and animal ovarian and testicular tissue.44-47 Although the role of progesterone in acne and its effect on sebaceous gland activity is not fully established, the possibility that endogenous progesterone is a precursor of testosterone or of another androgenic substance invites further exploration.48,49
- ↑ Vermorken, A. J. M.; Houben, J. J. G. (2016). "Topical Androgen Treatment for ACNE a Review". Drug Intelligence & Clinical Pharmacy. 12 (3): 151–157. doi:10.1177/106002807801200302. ISSN 0012-6578.
The only concern Voigt and Hsia expressed about the use of progesterone as an anti-androgen was the possibility that the small amount of hormone which reached the circulation could be converted into testosterone by the sexual organs, mainly the testes.
- ↑ Shufeng Zhou (6 April 2016). Cytochrome P450 2D6: Structure, Function, Regulation and Polymorphism. CRC Press. pp. 52–. ISBN 978-1-4665-9788-4.
- 1 2 Woods KS, Reyna R, Azziz R (2002). "Effect of oral micronized progesterone on androgen levels in women with polycystic ovary syndrome". Fertil. Steril. 77 (6): 1125–7. PMID 12057716.
The mean values of TT, FT, SHBG, DHEAS, A4, and 17-OHP did not change with OMP administration. However, a higher 17-OHP level was observable at the completion of OMP administration (week 2).
- 1 2 Whitehead MI, Townsend PT, Gill DK, Collins WP, Campbell S (1980). "Absorption and metabolism of oral progesterone". Br Med J. 280 (6217): 825–7. PMC 1600943. PMID 7370683.
Plasma concentrations of oestradiol were unchanged by giving progesterone.
- 1 2 3 Ottosson UB (1984). "Oral progesterone and estrogen/progestogen therapy. Effects of natural and synthetic hormones on subfractions of HDL cholesterol and liver proteins". Acta Obstet Gynecol Scand Suppl. 127: 1–37. PMID 6596830.
Natural progesterone is devoid of any androgenic activity that might compromise lipoprotein metabolism or induce teratogenicity.
- ↑ Samsioe, Göran; Dören, Martina; Lobo, Rogerio A (2006). "Hormone replacement therapy – the agents". Women's Health Medicine. 3 (5): 213–216. doi:10.1053/S1744-1870(06)70207-4. ISSN 1744-1870.
Progestogens differ in their relative metabolic and androgenic effects; for example MPA is minimally androgenic, but does counteract the rise in HDL-cholesterol caused by oestrogen therapy. In contrast, oral micronized progesterone does not mitigate against increased HDL-cholesterol levels.
- 1 2 3 4 5 6 7 Zutshi (2005). Hormones in Obstetrics and Gynaecology. Jaypee Brothers, Medical Publishers. pp. 74–75. ISBN 978-81-8061-427-9.
It has been observed that micronized progesterone has no suppressive effects on high-density lipoprotein-cholesterol (HDL-C). Jensen et al have proved that oral micronized progesterone has no adverse effect on serum lipids. These preparations have the same antiestrogenic and antimineralocorticoid effect but no androgenic action. It does not affect aldosterone synthesis, blood pressure, carbohydrate metabolism or mood changes. No side effects have been reported as far as lipid profile, coagulation factors and blood pressure are concerned.
- ↑ Levy T, Yairi Y, Bar-Hava I, Shalev J, Orvieto R, Ben-Rafael Z (2000). "Pharmacokinetics of the progesterone-containing vaginal tablet and its use in assisted reproduction" (PDF). Steroids. 65 (10–11): 645–9. PMID 11108871.
Natural progesterone is devoid of any androgenic activity and is thus extensively used in assisted reproduction, sometimes for long periods of time.
- ↑ Rižner TL, Brožič P, Doucette C, Turek-Etienne T, Müller-Vieira U, Sonneveld E, van der Burg B, Böcker C, Husen B (May 2011). "Selectivity and potency of the retroprogesterone dydrogesterone in vitro". Steroids. 76 (6): 607–15. doi:10.1016/j.steroids.2011.02.043. PMID 21376746.
- ↑ Swerdloff RS, Dudley RE, Page ST, Wang C, Salameh WA (2017). "Dihydrotestosterone: Biochemistry, Physiology, and Clinical Implications of Elevated Blood Levels". Endocr. Rev. 38 (3): 220–254. doi:10.1210/er.2016-1067. PMID 28472278.
- 1 2 Marks LS (2004). "5α-reductase: history and clinical importance". Rev Urol. 6 Suppl 9: S11–21. PMC 1472916. PMID 16985920.
- ↑ Golub MS, Kaufman FL, Campbell MA, Li LH, Donald JM (October 2006). ""Natural" progesterone: information on fetal effects". Birth Defects Res. B Dev. Reprod. Toxicol. 77 (5): 455–70. doi:10.1002/bdrb.20089. PMID 17066418.
Progesterone has been shown to inhibit 5α-reductase, another important enzyme in steroid hormone metabolism, (Dean and Winter, 1984; Beckmann et al., 1993; Cassidenti et al., 1991; Kadohama et al., 1983; Mauvais-Jarvis et al., 1974; Dube et al., 1975). However, this is a weak effect that has only been demonstrated at supra-physiological concentrations and in vitro conditions.
- ↑ Kincl, Fred A. (1990). "Control of Reproductive Function in the Adult". 31: 5–120. doi:10.1007/978-3-642-83794-4_2. ISSN 0077-1015.
Progesterone (and other progestational agents) inhibit testosterone from expressing its activity at the target sites (Kincl, 1971a). Mice and rats are the test animals of choice (Dorfman, 1963a,b). Inhibition of 5α-reductase activity of binding to cytosol and nuclear receptors has been shown to be the steps at which antiandrogens express their activity (Neumann and Steinbeck, 1974). Relatively high amounts are needed to achieve a significant effect (Table 2.16).
- ↑ Dewis P, Newman M, Anderson DC (October 1984). "The effect of endogenous progesterone on serum levels of 5α-reduced androgens in hirsute women". Clin. Endocrinol. (Oxf). 21 (4): 383–92. doi:10.1111/j.1365-2265.1984.tb03225.x. PMID 6542470.
These studies suggest that [...] a rise in serum progesterone has only a minimal effect on circulating levels of the active 5α‐reduced androgen metabolites. [...] Progesterone has been shown to be a potent in vitro inhibitor of cutaneous 5α-reductase (Mauvais-Jarvis et al., 1974). However we found only a small reduction in serum DHT levels in the late luteal phase in ovulatory women and no change in serum 3α-diol. Hence the rise in serum progesterone in ovulatory women has only a minimal effect on the circulating levels of the major active 5α-reduced androgens in vivo.
- ↑ Kålund-Jensen H, Myrén CJ (December 1984). "Vaginal absorption of oestradiol and progesterone". Maturitas. 6 (4): 359–67. doi:10.1016/0378-5122(84)90009-4. PMID 6543461.
- ↑ Picut CA, Ziejewski MK, Stanislaus D (February 2018). "Comparative Aspects of Pre- and Postnatal Development of the Male Reproductive System". Birth Defects Res. 110 (3): 190–227. doi:10.1002/bdr2.1133. PMID 29063715.
- ↑ Fred A. Kincl (6 December 2012). Hormone Toxicity in the Newborn. Springer Science & Business Media. p. 60. ISBN 978-3-642-83794-4.
- ↑ Kawashima K, Nakaura S, Nagao S, Tanaka S, Kuwamura T (February 1977). "Virilizing activities of various steroids in female rat fetuses". Endocrinol. Jpn. 24 (1): 77–81. doi:10.1507/endocrj1954.24.77. PMID 558879.
- ↑ Tony M. Plant; Anthony J. Zeleznik (15 November 2014). Knobil and Neill's Physiology of Reproduction. Academic Press. pp. 2289, 2386. ISBN 978-0-12-397769-4.
- ↑ Hormones, Brain and Behavior, Five-Volume Set. Elsevier. 18 June 2002. pp. 54–. ISBN 978-0-08-053415-2.
- ↑ Heidrich A, Schleyer M, Spingler H, Albert P, Knoche M, Fritze J, Lanczik M (February 1994). "Postpartum blues: relationship between not-protein bound steroid hormones in plasma and postpartum mood changes". J Affect Disord. 30 (2): 93–8. PMID 8201129.
- ↑ Baek, K.; Rosenwaks, Z.; Poppas, D.P.; Palermo, G.D. (2006). "P-657". Fertility and Sterility. 86 (3): S377. doi:10.1016/j.fertnstert.2006.07.1033. ISSN 0015-0282.
- ↑ Pharmacology of the Skin I: Pharmacology of Skin Systems Autocoids in Normal and Inflamed Skin. Springer Science & Business Media. 6 December 2012. pp. 249–250. ISBN 978-3-642-73797-8.
- 1 2 Pharmacology of the Skin II: Methods, Absorption, Metabolism and Toxicity, Drugs and Diseases. Springer Science & Business Media. 6 December 2012. pp. 253, 485–. ISBN 978-3-642-74054-1.
- 1 2 3 4 5 de Lignieres B, Dennerstein L, Backstrom T (April 1995). "Influence of route of administration on progesterone metabolism". Maturitas. 21 (3): 251–7. doi:10.1016/0378-5122(94)00882-8. PMID 7616875.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Nahoul K, Dehennin L, Jondet M, Roger M (May 1993). "Profiles of plasma estrogens, progesterone and their metabolites after oral or vaginal administration of estradiol or progesterone". Maturitas. 16 (3): 185–202. doi:10.1016/0378-5122(93)90064-O. PMID 8515718.
- 1 2 Warren MP, Shantha S (1999). "Uses of progesterone in clinical practice". Int J Fertil Womens Med. 44 (2): 96–103. PMID 10338267.
- 1 2 3 4 5 6 7 de Ziegler D, Fanchin R (2000). "Progesterone and progestins: applications in gynecology". Steroids. 65 (10–11): 671–9. doi:10.1016/S0039-128X(00)00123-9. PMID 11108875.
- 1 2 3 Turkmen S, Backstrom T, Wahlstrom G, Andreen L, Johansson IM (2011). "Tolerance to allopregnanolone with focus on the GABA-A receptor". Br. J. Pharmacol. 162 (2): 311–27. doi:10.1111/j.1476-5381.2010.01059.x. PMC 3031054. PMID 20883478.
- ↑ Timby E, Balgård M, Nyberg S, Spigset O, Andersson A, Porankiewicz-Asplund J, Purdy RH, Zhu D, Bäckström T, Poromaa IS (2006). "Pharmacokinetic and behavioral effects of allopregnanolone in healthy women". Psychopharmacology. 186 (3): 414–24. doi:10.1007/s00213-005-0148-7. PMID 16177884.
- 1 2 Follesa P, Concas A, Porcu P, Sanna E, Serra M, Mostallino MC, Purdy RH, Biggio G (2001). "Role of allopregnanolone in regulation of GABA(A) receptor plasticity during long-term exposure to and withdrawal from progesterone". Brain Res. Brain Res. Rev. 37 (1–3): 81–90. PMID 11744076.
- 1 2 3 Schiller CE, Schmidt PJ, Rubinow DR (2014). "Allopregnanolone as a mediator of affective switching in reproductive mood disorders". Psychopharmacology. 231 (17): 3557–67. doi:10.1007/s00213-014-3599-x. PMC 4135022. PMID 24846476.
- 1 2 3 Bäckström T, Haage D, Löfgren M, Johansson IM, Strömberg J, Nyberg S, Andréen L, Ossewaarde L, van Wingen GA, Turkmen S, Bengtsson SK (2011). "Paradoxical effects of GABA-A modulators may explain sex steroid induced negative mood symptoms in some persons". Neuroscience. 191: 46–54. doi:10.1016/j.neuroscience.2011.03.061. PMID 21600269.
- ↑ Andréen L, Sundström-Poromaa I, Bixo M, Andersson A, Nyberg S, Bäckström T (February 2005). "Relationship between allopregnanolone and negative mood in postmenopausal women taking sequential hormone replacement therapy with vaginal progesterone". Psychoneuroendocrinology. 30 (2): 212–24. doi:10.1016/j.psyneuen.2004.07.003. PMID 15471618.
- ↑ Pearlstein T (2016). "Treatment of Premenstrual Dysphoric Disorder: Therapeutic Challenges". Expert Rev Clin Pharmacol: 1–4. doi:10.1586/17512433.2016.1142371. PMID 26766596.
A recent study with a 5α-reductase inhibitor dutasteride, that blocks the conversion of progesterone to ALLO, reported that dutasteride 2.5 mg daily decreased several premenstrual symptoms [7].
- ↑ Sripada RK, Marx CE, King AP, Rampton JC, Ho SS, Liberzon I (2013). "Allopregnanolone elevations following pregnenolone administration are associated with enhanced activation of emotion regulation neurocircuits". Biol. Psychiatry. 73 (11): 1045–53. doi:10.1016/j.biopsych.2012.12.008. PMC 3648625. PMID 23348009.
- ↑ Ducharme N, Banks WA, Morley JE, Robinson SM, Niehoff ML, Mattern C, Farr SA (2010). "Brain distribution and behavioral effects of progesterone and pregnenolone after intranasal or intravenous administration". Eur. J. Pharmacol. 641 (2–3): 128–34. doi:10.1016/j.ejphar.2010.05.033. PMC 3008321. PMID 20570588.
- ↑ Saudan C, Desmarchelier A, Sottas PE, Mangin P, Saugy M (2005). "Urinary marker of oral pregnenolone administration". Steroids. 70 (3): 179–83. doi:10.1016/j.steroids.2004.12.007. PMID 15763596.
- 1 2 Piper T, Schlug C, Mareck U, Schänzer W (2011). "Investigations on changes in ¹³C/¹²C ratios of endogenous urinary steroids after pregnenolone administration". Drug Test Anal. 3 (5): 283–90. doi:10.1002/dta.281. PMID 21538944.
- ↑ Lark S (1999). Making the Estrogen Decision. McGraw-Hill Professional. p. 22. ISBN 9780879836962.
- ↑ Stricker R, Eberhart R, Chevailler MC, Quinn FA, Bischof P, Stricker R (2006). "Establishment of detailed reference values for luteinizing hormone, follicle stimulating hormone, estradiol, and progesterone during different phases of the menstrual cycle on the Abbott ARCHITECT analyzer". Clin. Chem. Lab. Med. 44 (7): 883–7. doi:10.1515/CCLM.2006.160. PMID 16776638.
- 1 2 3 4 5 6 7 van Keep P, Utian W (6 December 2012). The Premenstrual Syndrome: Proceedings of a workshop held during the Sixth International Congress of Psychosomatic Obstetrics and Gynecology, Berlin, September 1980. Springer Science & Business Media. pp. 51–52. ISBN 978-94-011-6255-5.
- ↑ Blackburn S (14 April 2014). Maternal, Fetal, & Neonatal Physiology. Elsevier Health Sciences. pp. 92–. ISBN 978-0-323-29296-2.
- ↑ Die Gestagene. Springer-Verlag. 27 November 2013. pp. 264–274. ISBN 978-3-642-99941-3.
- 1 2 3 4 5 6 de Lignières B (1999). "Oral micronized progesterone". Clin Ther. 21 (1): 41–60, discussion 1–2. doi:10.1016/S0149-2918(00)88267-3. PMID 10090424.
- ↑ Arafat ES, Hargrove JT, Maxson WS, Desiderio DM, Wentz AC, Andersen RN (November 1988). "Sedative and hypnotic effects of oral administration of micronized progesterone may be mediated through its metabolites". Am. J. Obstet. Gynecol. 159 (5): 1203–9. doi:10.1097/00006254-198904000-00015. PMID 3189454.
- 1 2 3 Freeman EW, Weinstock L, Rickels K, Sondheimer SJ, Coutifaris C (March 1992). "A placebo-controlled study of effects of oral progesterone on performance and mood". Br J Clin Pharmacol. 33 (3): 293–8. doi:10.1111/j.1365-2125.1992.tb04038.x. PMC 1381278. PMID 1576050.
- ↑ Kleinstein J, Schlegelmilch R, Mazur D, Vens-Cappell B (2002). "[Pharmacokinetic comparison of progesterone capsules with a progesterone gel after vaginal administration]". Arzneimittelforschung (in German). 52 (8): 615–21. doi:10.1055/s-0031-1299940. PMID 12236050.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 Kuhl H, Schneider HP (August 2013). "Progesterone – promoter or inhibitor of breast cancer". Climacteric. 16 Suppl 1: 54–68. doi:10.3109/13697137.2013.768806. PMID 23336704.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 Davey DA (March 2018). "Menopausal hormone therapy: a better and safer future". Climacteric: 1–8. doi:10.1080/13697137.2018.1439915. PMID 29526116.
- ↑ Cynthia C. Chernecky; Barbara J. Berger (31 October 2012). Laboratory Tests and Diagnostic Procedures - E-Book. Elsevier Health Sciences. pp. 908–. ISBN 1-4557-4502-2.
- ↑ Lalit Bajaj; Stephen Berman (1 January 2011). Berman's Pediatric Decision Making. Elsevier Health Sciences. pp. 160–. ISBN 0-323-05405-6.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Kuhl H (2011). "Pharmacology of Progestogens" (PDF). Journal für Reproduktionsmedizin und Endokrinologie-Journal of Reproductive Medicine and Endocrinology. 8 (1): 157–177.
- 1 2 3 4 5 6 7 8 9 10 Fotherby K (August 1996). "Bioavailability of orally administered sex steroids used in oral contraception and hormone replacement therapy". Contraception. 54 (2): 59–69. doi:10.1016/0010-7824(96)00136-9. PMID 8842581.
Progesterone is rapidly metabolized which leads to a low bioavailability and the necessity for high doses (200 mg); its pharmacological actions, except upon reproductive processes, are weak. [...] For many years after its isolation and synthesis, progesterone could only be used therapeutically by intramuscular injection of large doses since it was quickly recognized that, after oral administration, progesterone was poorly absorbed and rapidly metabolized in the gastrointestinal tract, liver and most tissues, and then eliminated. However, like estradiol, the absorption of progesterone can be improved by micronization.16 This led to the development of formulations of progesterone, mainly of particle size <10 μg, dissolved in oil in a gelatin capsule. [...] five formulations differing in particle size and vehicle were compared; all led to significant absorption of progesterone and with similar plasma progesterone concentrations 6 hours after administration, but only the micronized or oil vehicle preparations improved absorption (probably by increasing lymphatic absorption and thus avoiding some of the first-pass effect). [...] Plasma progesterone concentrations may be higher when the formulation is administered with food but, even under the best conditions, bioavailability appears to be very low since the AUC after intramuscular injection of progesterone is at least ten times higher than after oral intake.21
- 1 2 3 4 5 6 7 8 9 10 11 12 Ruan X, Mueck AO (November 2014). "Systemic progesterone therapy—oral, vaginal, injections and even transdermal?". Maturitas. 79 (3): 248–55. doi:10.1016/j.maturitas.2014.07.009. PMID 25113944.
- ↑ Lynn Wecker (31 May 2018). Brody's Human Pharmacology E-Book. Elsevier Health Sciences. pp. 419–. ISBN 978-0-323-59662-6.
- 1 2 3 4 Anita MV; Sandhya Jain; Neerja Goel (31 July 2018). Use of Progestogens in Clinical Practice of Obstetrics and Gynecology. JP Medical Ltd. pp. 4, 15–20. ISBN 978-93-5270-218-3.
Progesterone is also available in the forms of vaginal or rectal suppositories or pessaries (Cyclogest), [...]
- ↑ David J. Hauss (8 June 2007). Oral Lipid-Based Formulations: Enhancing the Bioavailability of Poorly Water-Soluble Drugs. CRC Press. pp. 17–. ISBN 978-1-4200-1726-7.
- ↑ Marc S. Micozzi; Tieraona Low Dog (19 August 2004). Women's Health in Complementary and Integrative Medicine E-Book: A Clinical Guide. Elsevier Health Sciences. pp. 69–. ISBN 0-7020-3598-X.
- ↑ Porter CJ, Pouton CW, Cuine JF, Charman WN (March 2008). "Enhancing intestinal drug solubilisation using lipid-based delivery systems". Adv. Drug Deliv. Rev. 60 (6): 673–91. doi:10.1016/j.addr.2007.10.014. PMID 18155801.
- 1 2 Humberstone, Andrew J.; Charman, William N. (1997). "Lipid-based vehicles for the oral delivery of poorly water soluble drugs". Advanced Drug Delivery Reviews. 25 (1): 103–128. doi:10.1016/S0169-409X(96)00494-2. ISSN 0169-409X.
- 1 2 Kincl FA, Ciaccio LA, Benagiano G (January 1978). "Increasing oral bioavailability of progesterone by formulation". J. Steroid Biochem. 9 (1): 83–4. doi:10.1016/0022-4731(78)90106-1. PMID 628211.
- 1 2 Hargrove JT, Maxson WS, Wentz AC (October 1989). "Absorption of oral progesterone is influenced by vehicle and particle size". Am. J. Obstet. Gynecol. 161 (4): 948–51. doi:10.1016/0002-9378(89)90759-X. PMID 2801843.
- ↑ Schindler AE, Campagnoli C, Druckmann R, Huber J, Pasqualini JR, Schweppe KW, Thijssen JH (2008). "Classification and pharmacology of progestins" (PDF). Maturitas. 61 (1–2): 171–80. doi:10.1016/j.maturitas.2008.11.013. PMID 19434889.
- 1 2 3 4 5 6 Hermann AC, Nafziger AN, Victory J, Kulawy R, Rocci ML, Bertino JS (2005). "Over-the-counter progesterone cream produces significant drug exposure compared to a food and drug administration-approved oral progesterone product". J Clin Pharmacol. 45 (6): 614–9. doi:10.1177/0091270005276621. PMID 15901742.
- ↑ J. Larry Jameson; Leslie J. De Groot (25 February 2015). Endocrinology: Adult and Pediatric E-Book. Elsevier Health Sciences. pp. 2660–. ISBN 978-0-323-32195-2.
- ↑ Integrative Medicine. Elsevier Health Sciences. 2012. p. 343. ISBN 1-4377-1793-4.
- ↑ Mark V. Sauer (1 March 2013). Principles of Oocyte and Embryo Donation. Springer Science & Business Media. pp. 117–. ISBN 978-1-4471-2392-7.
- 1 2 3 Alam V, Vega M, Rísquez F (2001). "Luteal phase support". Reprod. Biomed. Online. 3 (3): 250–262. doi:10.1016/S1472-6483(10)62044-5. PMID 12513863.
- ↑ Alexandre Hohl (30 March 2017). Testosterone: From Basic to Clinical Aspects. Springer. pp. 13–. ISBN 978-3-319-46086-4.
- ↑ Eberhard Nieschlag; Hermann M. Behre; Susan Nieschlag (26 July 2012). Testosterone: Action, Deficiency, Substitution. Cambridge University Press. pp. 313–. ISBN 978-1-107-01290-5.
- ↑ Bagchus WM, Hust R, Maris F, Schnabel PG, Houwing NS (March 2003). "Important effect of food on the bioavailability of oral testosterone undecanoate". Pharmacotherapy. 23 (3): 319–25. doi:10.1592/phco.23.3.319.32104. PMID 12627930.
- ↑ Schnabel PG, Bagchus W, Lass H, Thomsen T, Geurts TB (April 2007). "The effect of food composition on serum testosterone levels after oral administration of Andriol Testocaps". Clin. Endocrinol. (Oxf). 66 (4): 579–85. doi:10.1111/j.1365-2265.2007.02781.x. PMC 1859980. PMID 17371478.
- ↑ Reddy DS (2010). "Neurosteroids: endogenous role in the human brain and therapeutic potentials". Progress in Brain Research. 186: 113–37. doi:10.1016/B978-0-444-53630-3.00008-7. PMC 3139029. PMID 21094889.
- ↑ Söderpalm AH, Lindsey S, Purdy RH, Hauger R, Wit de H (2004). "Administration of progesterone produces mild sedative-like effects in men and women". Psychoneuroendocrinology. 29 (3): 339–54. doi:10.1016/s0306-4530(03)00033-7. PMID 14644065.
- 1 2 3 de Wit H, Schmitt L, Purdy R, Hauger R (2001). "Effects of acute progesterone administration in healthy postmenopausal women and normally-cycling women". Psychoneuroendocrinology. 26 (7): 697–710. doi:10.1016/s0306-4530(01)00024-5. PMID 11500251.
- ↑ van Broekhoven F, Bäckström T, Verkes RJ (2006). "Oral progesterone decreases saccadic eye velocity and increases sedation in women". Psychoneuroendocrinology. 31 (10): 1190–9. doi:10.1016/j.psyneuen.2006.08.007. PMID 17034954.
- ↑ Wren BG, Day RO, McLachlan AJ, Williams KM (June 2003). "Pharmacokinetics of estradiol, progesterone, testosterone and dehydroepiandrosterone after transbuccal administration to postmenopausal women". Climacteric. 6 (2): 104–11. doi:10.1080/cmt.6.2.104.111. PMID 12841880.
- 1 2 3 Chakmakjian ZH, Zachariah NY (June 1987). "Bioavailability of progesterone with different modes of administration". J Reprod Med. 32 (6): 443–8. PMID 3612635.
- 1 2 Villanueva B, Casper RF, Yen SS (April 1981). "Intravaginal administration of progesterone: enhanced absorption after estrogen treatment". Fertil. Steril. 35 (4): 433–7. doi:10.1016/S0015-0282(16)45439-7. PMID 7215569.
- 1 2 3 Zygmunt, Malgozhata; Sapa, Yatsek (2017). "Progesterone – a new look at an old drug". Reproductive Endocrinology. 0 (33): 17–25. doi:10.18370/2309-4117.2017.33.17-25. ISSN 2411-1295.
[In other pharmacokinetic studies it has been proven that after administration of 100 mg of progesterone the hormone reached its maximum concentration in the plasma after 1-4 hours, which was on average 13.5 ng/mL.]
- 1 2 3 4 5 6 7 8 9 10 Unfer V, Casini ML, Marelli G, Costabile L, Gerli S, Di Renzo GC (2005). "Different routes of progesterone administration and polycystic ovary syndrome: a review of the literature". Gynecol. Endocrinol. 21 (2): 119–27. doi:10.1080/09513590500170049. PMID 16109599.
- 1 2 3 4 Stovall DW, Van Voorhis BJ, Mattingly KL, Sparks AE, Chapler FK, Syrop CH (May 1996). "The effectiveness of sublingual progesterone administration during cryopreserved embryo transfer cycles: results of a matched follow-up study". Fertil. Steril. 65 (5): 986–91. doi:10.1016/S0015-0282(16)58274-0. PMID 8612862.
- ↑ BICKERS W (August 1949). "Progesterone; a comparison of intramuscular, oral and sublingual routes of administration". J. Clin. Endocrinol. Metab. 9 (8): 736–42. doi:10.1210/jcem-9-8-736. PMID 18133494.
- ↑ Corner, George W. (1944). "The Absorption of Steroid Hormones from the Oral Mucous Membranes, with Special Reference to the Sublingual Administration of Progesterone". American Journal of Obstetrics and Gynecology. 47 (5): 670–677. doi:10.1016/S0002-9378(16)40321-2. ISSN 0002-9378.
- ↑ Greenblatt, Robert B. (1944). "Sublingual Absorption of Progesterone and Anhydrohydroxyprogesterone". The Journal of Clinical Endocrinology & Metabolism. 4 (4): 156–158. doi:10.1210/jcem-4-4-156. ISSN 0021-972X.
- 1 2 Steege JF, Rupp SL, Stout AL, Bernhisel M (October 1986). "Bioavailability of nasally administered progesterone". Fertil. Steril. 46 (4): 727–9. doi:10.1016/S0015-0282(16)49661-5. PMID 3758397.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Stanczyk FZ (2014). "Treatment of postmenopausal women with topical progesterone creams and gels: are they effective?". Climacteric. 17 Suppl 2: 8–11. doi:10.3109/13697137.2014.944496. PMID 25196424.
- 1 2 3 4 5 6 7 8 9 10 11 12 Stanczyk FZ, Paulson RJ, Roy S (2005). "Percutaneous administration of progesterone: blood levels and endometrial protection". Menopause. 12 (2): 232–7. PMID 15772572.
- 1 2 3 Du JY, Sanchez P, Kim L, Azen CG, Zava DT, Stanczyk FZ (2013). "Percutaneous progesterone delivery via cream or gel application in postmenopausal women: a randomized cross-over study of progesterone levels in serum, whole blood, saliva, and capillary blood". Menopause. 20 (11): 1169–75. doi:10.1097/GME.0b013e31828d39a2. PMID 23652031.
- 1 2 3 4 5 Bińkowska, Małgorzata; Woroń, Jarosław (2015). "Progestogens in menopausal hormone therapy". Menopausal Review. 2: 134–143. doi:10.5114/pm.2015.52154. ISSN 1643-8876.
- ↑ Marker RE, Krueger J (1940). "Sterols. CXII. Sapogenins. XLI. The Preparation of Trillin and its Conversion to Progesterone". J. Am. Chem. Soc. 62 (12): 3349–3350. doi:10.1021/ja01869a023.
- ↑ Zava DT, Dollbaum CM, Blen M (March 1998). "Estrogen and progestin bioactivity of foods, herbs, and spices". Proceedings of the Society for Experimental Biology and Medicine. Society for Experimental Biology and Medicine. 217 (3): 369–78. doi:10.3181/00379727-217-44247. PMID 9492350.
- ↑ Komesaroff PA, Black CV, Cable V, Sudhir K (June 2001). "Effects of wild yam extract on menopausal symptoms, lipids and sex hormones in healthy menopausal women". Climacteric. 4 (2): 144–50. doi:10.1080/713605087. PMID 11428178.
- ↑ Schmidt JW, Wollner D, Curcio J, Riedlinger J, Kim LS (October 2006). "Hormone replacement therapy in menopausal women: Past problems and future possibilities". Gynecol. Endocrinol. 22 (10): 564–77. doi:10.1080/09513590600927017. PMID 17135036.
- ↑ E Scott Sills (7 September 2015). Screening the Single Euploid Embryo: Molecular Genetics in Reproductive Medicine. Springer. pp. 276–277. ISBN 978-3-319-16892-0.
- ↑ E.P.W. Tatford (6 December 2012). Problems in Gynaecology. Springer Science & Business Media. pp. 85–. ISBN 978-94-009-4125-0.
Progesterone can also be given by rectal or vaginal suppository (Cyclogest) in a dose of 400 mg daily.
- ↑ Aghsa MM, Rahmanpour H, Bagheri M, Davari-Tanha F, Nasr R (October 2012). "A randomized comparison of the efficacy, side effects and patient convenience between vaginal and rectal administration of Cyclogest(®) when used for luteal phase support in ICSI treatment". Arch. Gynecol. Obstet. 286 (4): 1049–54. doi:10.1007/s00404-012-2410-7. PMID 22714063.
- ↑ Khrouf M, Slimani S, Khrouf MR, Braham M, Bouyahia M, Berjeb KK, Chaabane HE, Merdassi G, Kaffel AZ, Zhioua A, Zhioua F (2016). "Progesterone for Luteal Phase Support in In Vitro Fertilization: Comparison of Vaginal and Rectal Pessaries to Vaginal Capsules: A Randomized Controlled Study". Clin Med Insights Womens Health. 9: 43–47. doi:10.4137/CMWH.S32156. PMC 5217976. PMID 28096703.
- 1 2 Tay PY, Lenton EA (June 2005). "The impact of luteal supplement on pregnancy outcome following stimulated IVF cycles" (PDF). Med. J. Malaysia. 60 (2): 151–7. PMID 16114155.
- ↑ van der Meer YG, van Loenen AC, Loendersloot EW, Jaszmann LJ (October 1982). "Plasma progesterone levels after using high dose suppositories. A preliminary report". Pharm Weekbl Sci. 4 (5): 135–6. doi:10.1007/BF01959031. PMID 7145597.
- ↑ Nillius SJ, Johansson ED (June 1971). "Plasma levels of progesterone after vaginal, rectal, or intramuscular administration of progesterone". Am. J. Obstet. Gynecol. 110 (4): 470–7. doi:10.1016/0002-9378(71)90686-7. PMID 5582003.
- 1 2 3 Bernardo-Escudero R, Cortés-Bonilla M, Alonso-Campero R, Francisco-Doce MT, Chavarín-González J, Pimentel-Martínez S, Zambrano-Tapia L (2012). "Observational study of the local tolerability of injectable progesterone microspheres". Gynecol. Obstet. Invest. 73 (2): 124–9. doi:10.1159/000330711. PMID 21997608.
- ↑ Tobías, G. M., Usabiaga, R. A. S., Riaño, J. D., Espinoza, A. B., Tovar, S. R., & Martínez, E. R. V. (2008). Progesterona en Microesferas para el Tratamiento en Infertilidad. Acta Médica Grupo Ángeles, 6(1), 8. http://www.medigraphic.com/pdfs/actmed/am-2008/am081b.pdf
- ↑ Tobías, G. M., & Martínez, E. R. V. (2009). Técnica para Aplicación de Fármacos con Microesferas en Suspensión. Acta Médica Grupo Ángeles, 7(1), 13. http://www.medigraphic.com/pdfs/actmed/am-2009/am091b.pdf
- ↑ Lockwood G, Griesinger G, Cometti B (2014). "Subcutaneous progesterone versus vaginal progesterone gel for luteal phase support in in vitro fertilization: a noninferiority randomized controlled study". Fertil. Steril. 101 (1): 112–119.e3. doi:10.1016/j.fertnstert.2013.09.010. PMID 24140033.
- 1 2 3 Baker VL, Jones CA, Doody K, Foulk R, Yee B, Adamson GD, et al. (2014). "A randomized, controlled trial comparing the efficacy and safety of aqueous subcutaneous progesterone with vaginal progesterone for luteal phase support of in vitro fertilization". Hum. Reprod. 29 (10): 2212–20. doi:10.1093/humrep/deu194. PMC 4164149. PMID 25100106.
- 1 2 3 4 Tommaso Falcone; William W. Hurd (1 January 2007). Clinical Reproductive Medicine and Surgery. Elsevier Health Sciences. pp. 406–. ISBN 0-323-03309-1.
- 1 2 Ethel Sloane (2002). Biology of Women. Cengage Learning. pp. 445–. ISBN 0-7668-1142-5.
- ↑ Rogerio A. Lobo (5 June 2007). Treatment of the Postmenopausal Woman: Basic and Clinical Aspects. Elsevier. pp. 210–. ISBN 978-0-08-055309-2.
- ↑ Ian S. Fraser (1998). Estrogens and Progestogens in Clinical Practice. Churchill Livingstone. p. 92. ISBN 978-0-443-04706-0.
Further reading
- Sitruk-Ware R, Bricaire C, De Lignieres B, Yaneva H, Mauvais-Jarvis P (October 1987). "Oral micronized progesterone. Bioavailability pharmacokinetics, pharmacological and therapeutic implications--a review". Contraception. 36 (4): 373–402. doi:10.1016/0010-7824(87)90088-6. PMID 3327648.
- Simon JA (December 1995). "Micronized progesterone: vaginal and oral uses". Clinical Obstetrics and Gynecology. 38 (4): 902–14. doi:10.1097/00003081-199538040-00024. PMID 8616985.
- Ruan X, Mueck AO (November 2014). "Systemic progesterone therapy--oral, vaginal, injections and even transdermal?". Maturitas. 79 (3): 248–55. doi:10.1016/j.maturitas.2014.07.009. PMID 25113944.