Arketamine
 | |
| Clinical data | |
|---|---|
| ATC code |
|
| Legal status | |
| Legal status |
|
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| UNII | |
| Chemical and physical data | |
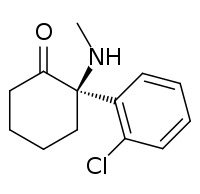
| Formula | C13H16ClNO |
| Molar mass | 237.725 g/mol |
| 3D model (JSmol) | |
| |
| |
Arketamine, also (R)-ketamine or (R)-(−)-ketamine, is the (R)-(−) enantiomer of ketamine.[1][2][3][4] Similarly to racemic ketamine and esketamine, the S(+) enantiomer of ketamine, arketamine is biologically active; however, it is less potent as an NMDA receptor antagonist and anesthetic and thus has never been approved or marketed for clinical use as an enantiopure drug.[1][4]
Relative to esketamine, arketamine possesses 4–5 times lower affinity for the PCP site of the NMDA receptor.[2][3][5] In accordance, arketamine is significantly less potent than racemic ketamine and especially esketamine in terms of anesthetic, analgesic, and sedative-hypnotic effects.[2][5] Racemic ketamine has weak affinity for the sigma receptor, where it acts as an agonist, whereas esketamine binds negligibly to this receptor, and so the sigma receptor activity of racemic ketamine lies in arketamine.[6] It has been suggested that this action of arketamine may play a role in the hallucinogenic effects of racemic ketamine and that it may be responsible for the lowering of the seizure threshold seen with racemic ketamine.[2][6] Esketamine inhibits the dopamine transporter about 8-fold more potently than does arketamine, and so is about 8 times more potent as a dopamine reuptake inhibitor.[7] Arketamine and esketamine possess similar potency for interaction with the muscarinic acetylcholine receptors.[8]
Novel antidepressant
Arketamine appears to be more effective as a rapid-acting antidepressant than esketamine.[9]
In rodent studies, esketamine produced hyperlocomotion, prepulse inhibition deficits, and rewarding effects, while arketamine did not, in accordance with its lower potency as an NMDA receptor antagonist and dopamine reuptake inhibitor.[10] As such, arketamine may have a lower propensity for producing psychotomimetic effects and a lower abuse potential in addition to superior antidepressant efficacy.[10]
A study conducted in mice found that ketamine's antidepressant activity is not caused by ketamine inhibiting NMDAR, but rather by sustained activation of a different glutamate receptor, the AMPA receptor, by a metabolite, (2R,6R)-hydroxynorketamine; as of 2017 it was unknown if this was happening in humans.[11][12] Arketamine is a AMPA receptor agonist.[13]
Paradoxically, arketamine shows greater and longer-lasting rapid antidepressant effects in animal models of depression relative to esketamine.[9][14][10] It has been suggested that this difference may have due to with the possibility of different activity of arketamine and esketamine and their respective metabolites at the α7-nicotinic receptor, as norketamine and hydroxynorketamine are potent antagonists of this receptor and markers of potential rapid antidepressant effects (specifically, increased mammalian target of rapamycin function) correlate closely with their affinity for it.[15][16][17] The picture is unclear however, and other mechanisms have also been implicated.[10]
References
- 1 2 C.R. Ganellin; David J. Triggle (21 November 1996). Dictionary of Pharmacological Agents. CRC Press. pp. 1188–. ISBN 978-0-412-46630-4.
- 1 2 3 4 John D. Current, M.D. Pharmacology for Anesthetists. PediaPress. pp. 263–. GGKEY:6RRHEC392UN.
- 1 2 David T. Yew (6 March 2015). Ketamine: Use and Abuse. Taylor & Francis. pp. 269–. ISBN 978-1-4665-8340-5.
- 1 2 Singh, Jaskaran B.; Fedgchin, Maggie; Daly, Ella; Xi, Liwen; Melman, Caroline; De Bruecker, Geert; Tadic, Andre; Sienaert, Pascal; Wiegand, Frank; Manji, Husseini; Drevets, Wayne C.; Van Nueten, Luc (2015). "Intravenous Esketamine in Adult Treatment-Resistant Depression: A Double-Blind, Double-Randomization, Placebo-Controlled Study". Biological Psychiatry. 80: 424–31. doi:10.1016/j.biopsych.2015.10.018. ISSN 0006-3223. PMID 26707087.
- 1 2 Paul G. Barash; Bruce F. Cullen; Robert K. Stoelting; Michael Cahalan; M. Christine Stock (28 March 2012). Clinical Anesthesia. Lippincott Williams & Wilkins. pp. 456–. ISBN 978-1-4511-4795-7.
- 1 2 Joris C. Verster; Kathleen Brady; Marc Galanter; Patricia Conrod (6 July 2012). Drug Abuse and Addiction in Medical Illness: Causes, Consequences and Treatment. Springer Science & Business Media. pp. 205–. ISBN 978-1-4614-3375-0.
- ↑ Nishimura M, Sato K (1999). "Ketamine stereoselectively inhibits rat dopamine transporter". Neurosci. Lett. 274 (2): 131–4. doi:10.1016/s0304-3940(99)00688-6. PMID 10553955.
- ↑ J. Vuyk; Stefan Schraag (6 December 2012). Advances in Modelling and Clinical Application of Intravenous Anaesthesia. Springer Science & Business Media. pp. 270–. ISBN 978-1-4419-9192-8.
- 1 2 Zhang JC, Li SX, Hashimoto K (2014). "R (-)-ketamine shows greater potency and longer-lasting antidepressant effects than S (+)-ketamine". Pharmacol. Biochem. Behav. 116: 137–41. doi:10.1016/j.pbb.2013.11.033. PMID 24316345.
- 1 2 3 4 Yang C, Shirayama Y, Zhang JC, Ren Q, Yao W, Ma M, Dong C, Hashimoto K (2015). "R-ketamine: a rapid-onset and sustained antidepressant without psychotomimetic side effects". Transl Psychiatry. 5: e632. doi:10.1038/tp.2015.136. PMC 5068814. PMID 26327690.
- ↑ Tyler, Marshall W.; Yourish, Harmony B.; Ionescu, Dawn F.; Haggarty, Stephen J. (2017-04-21). "Classics in Chemical Neuroscience: Ketamine". ACS chemical neuroscience. doi:10.1021/acschemneuro.7b00074. ISSN 1948-7193. PMID 28418641.
- ↑ Zanos, Panos; Moaddel, Ruin; Morris, Patrick J.; Georgiou, Polymnia; Fischell, Jonathan; Elmer, Greg I.; Alkondon, Manickavasagom; Yuan, Peixiong; Pribut, Heather J.; Singh, Nagendra S.; Dossou, Katina S. S.; Fang, Yuhong; Huang, Xi-Ping; Mayo, Cheryl L.; Wainer, Irving W.; Albuquerque, Edson X.; Thompson, Scott M.; Thomas, Craig J.; Zarate Jr, Carlos A.; Gould, Todd D. (2016). "NMDAR inhibition-independent antidepressant actions of ketamine metabolites". Nature. 533: 481–486. doi:10.1038/nature17998. ISSN 0028-0836. PMC 4922311. PMID 27144355.
- ↑ Yang, Chun; Zhou, Wei; Li, Xiaomin; Yang, Jianjun; Szewczyk, Bernadeta; Pałucha-Poniewiera, Agnieszka; Poleszak, Ewa; Pilc, Andrzej; Nowak, Gabriel (2012). "A bright future of researching AMPA receptor agonists for depression treatment". Expert Opinion on Investigational Drugs. 21: 583–585. doi:10.1517/13543784.2012.667399.
- ↑ Hashimoto, Kenji (2014). "The R-Stereoisomer of Ketamine as an Alternative for Ketamine for Treatment-resistant Major Depression". Clinical Psychopharmacology and Neuroscience. 12 (1): 72–73. doi:10.9758/cpn.2014.12.1.72. ISSN 1738-1088.
- ↑ van Velzen, Monique; Dahan, Albert (2014). "Ketamine Metabolomics in the Treatment of Major Depression". Anesthesiology. 121 (1): 4–5. doi:10.1097/ALN.0000000000000286. ISSN 0003-3022.
- ↑ Paul RK, Singh NS, Khadeer M, Moaddel R, Sanghvi M, Green CE, O'Loughlin K, Torjman MC, Bernier M, Wainer IW (2014). "(R,S)-Ketamine metabolites (R,S)-norketamine and (2S,6S)-hydroxynorketamine increase the mammalian target of rapamycin function". Anesthesiology. 121 (1): 149–59. doi:10.1097/ALN.0000000000000285. PMC 4061505. PMID 24936922.
- ↑ Singh NS, Zarate CA, Moaddel R, Bernier M, Wainer IW (2014). "What is hydroxynorketamine and what can it bring to neurotherapeutics?". Expert Rev Neurother. 14 (11): 1239–42. doi:10.1586/14737175.2014.971760. PMID 25331415.