Niacin
| |||
| Names | |||
|---|---|---|---|
| Pronunciation | /ˈnaɪəsɪn/ | ||
| Preferred IUPAC name
Pyridine-3-carboxylic acid[1] | |||
Other names
| |||
| Identifiers | |||
3D model (JSmol) |
|||
| 3DMet | B00073 | ||
| 109591 | |||
| ChEBI | |||
| ChEMBL | |||
| ChemSpider | |||
| DrugBank | |||
| ECHA InfoCard | 100.000.401 | ||
| EC Number | 200-441-0 | ||
| 3340 | |||
| KEGG | |||
| MeSH | Niacin | ||
PubChem CID |
|||
| RTECS number | QT0525000 | ||
| UNII | |||
| |||
| |||
| Properties | |||
| C 6NH 5O 2 | |||
| Molar mass | 123.1094 g mol−1 | ||
| Appearance | White, translucent crystals | ||
| Density | 1.473 g cm−3 | ||
| Melting point | 237 °C; 458 °F; 510 K | ||
| 18 g L−1 | |||
| log P | 0.219 | ||
| Acidity (pKa) | 2.0, 4.85 | ||
| Isoelectric point | 4.75 | ||
Refractive index (nD) |
1.4936 | ||
| 0.1271305813 D | |||
| Thermochemistry | |||
Std enthalpy of formation (ΔfH |
−344.9 kJ mol−1 | ||
Std enthalpy of combustion (ΔcH |
−2.73083 MJ mol−1 | ||
| Pharmacology | |||
| C04AC01 (WHO) C10AD02 (WHO) | |||
| License data |
| ||
| Intramuscular, by mouth | |||
| Pharmacokinetics: | |||
| 20–45 min | |||
| Hazards | |||
EU classification (DSD) (outdated) |
|||
| R-phrases (outdated) | R36/37/38 | ||
| S-phrases (outdated) | S26, S36 | ||
| NFPA 704 | |||
| Flash point | 193 °C (379 °F; 466 K) | ||
| 365 °C (689 °F; 638 K) | |||
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). | |||
| Infobox references | |||
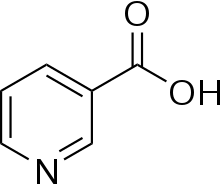
Niacin, also known as nicotinic acid, is an organic compound and a form of vitamin B3, an essential human nutrient. It has the formula C
6H
5NO
2 and belongs to the group of the pyridinecarboxylic acid.
Niacin is obtained in the diet from a variety of whole and processed foods, with highest contents in fortified packaged foods, tuna, some vegetable and other animal sources. Some countries require its addition to grains.[2] Medication and supplemental niacin are primarily used to treat high blood cholesterol and pellagra (niacin deficiency). Insufficient niacin in the diet can cause nausea, skin and mouth lesions, anemia, headaches, and tiredness. The lack of niacin may also be observed in pandemic deficiency diseases, which are caused by a lack of five crucial vitamins (niacin, vitamin C, thiamin, vitamin D, and vitamin A) and are usually found in areas of widespread poverty and malnutrition.
This colorless, water-soluble solid is a derivative of pyridine, with a carboxyl group (COOH) at the 3-position. Other forms of vitamin B3 include the corresponding amide nicotinamide (niacinamide), where the carboxyl group has been replaced by a carboxamide group (CONH
2), as well as more complex amides and a variety of esters.
Niacin and nicotinamide are both precursors of the coenzymes nicotinamide adenine dinucleotide (NAD) and nicotinamide adenine dinucleotide phosphate (NADP) in vivo.[3] NAD converts to NADP by phosphorylation in the presence of the enzyme NAD+ kinase. NADP and NAD are coenzymes for many dehydrogenases, participating in many hydrogen transfer processes.[4] NAD is important in catabolism of fat, carbohydrate, protein, and alcohol, as well as cell signaling and DNA repair, and NADP mostly in anabolism reactions such as fatty acid and cholesterol synthesis.[4] High energy requirements (brain) or high turnover rate (gut, skin) organs are usually the most susceptible to their deficiency.[5]
Niacin supplementation has not been found useful for decreasing the risk of cardiovascular disease in those already on a statin,[6] but appears to be effective in those not taking a statin.[7] Although niacin and nicotinamide are identical in their vitamin activity, nicotinamide does not have the same pharmacological effects (lipid-modifying effects) as niacin. Nicotinamide does not reduce cholesterol or cause flushing.[8] As the precursor for NAD and NADP, niacin is also involved in DNA repair.[9][10]
Medical uses
Treatment of deficiency
Niacin and niacinamide are used for prevention and treatment of pellagra.[11]
Abnormal lipids
Niacin has sometimes been used in addition to other lipid-lowering medications.[12] Systematic reviews found no effect of niacin on cardiovascular disease or death, in spite of raising HDL cholesterol, and reported side effects including an increased risk of diabetes.[6][13][14]
Contraindications
Niacin is contraindicated with active liver disease, persistent elevated serum transaminases, active peptic ulcer disease, or arterial bleeding.[15]
Side effects
The most common adverse effects are flushing (e.g., warmth, redness, itching or tingling), headache, pain, abdominal pain, diarrhea, dyspepsia, nausea, vomiting, rhinitis, pruritus and rash. These can be minimized by initiating therapy at low dosages, increasing dosage gradually, and avoiding administration on an empty stomach.[15] High doses of niacin often temporarily reduce blood pressure as a result of acute vasodilation.[16] In the longer term, high-dose niacin use may persistently lower blood pressure in individuals with hypertension, but more research is needed to determine the extent of this effect.[16]
Facial flushing
Flushing usually lasts for about 15 to 30 minutes, though it can sometimes last up to two hours. It is sometimes accompanied by a prickly or itching sensation, in particular, in areas covered by clothing. Flushing can be blocked by taking 300 mg of aspirin half an hour before taking niacin, by taking one tablet of ibuprofen per day or by co-administering the prostaglandin receptor antagonist laropiprant. Taking niacin with meals also helps reduce this side effect. Acquired tolerance will also help reduce flushing; after several weeks of a consistent dose, most patients no longer experience flushing.[17] Reduction of flushing focuses on altering or blocking the prostaglandin-mediated pathway.[18] Slow- or "sustained"-release forms of niacin have been developed to lessen these side effects.[19][20] One study showed the incidence of flushing was significantly lower with a sustained-release formulation,[21] though doses above 2 g per day have been associated with liver damage, in particular, with slow-release formulations.[22]
Prostaglandin (PGD2) is the primary cause of the flushing reaction, with serotonin appearing to have a secondary role in this reaction.[23] The effect is mediated by prostaglandin E2 and D2 due to GPR109A activation of epidermal Langerhans cells and keratinocytes.[24][25] Langerhans cells use cyclooxygenase type 1 (COX-1) for PGE2 production and are more responsible for acute flushing, while keratinocytes are COX-2 dependent and are in active continued vasodilation.[26][27] Flushing was often thought to involve histamine, but histamine has been shown not to be involved in the reaction.[23]
Gastrointestinal and hepatic
Gastrointestinal complaints, such as indigestion, nausea and liver failure, have also been reported. Hepatotoxicity is possibly related to metabolism via amidation resulting in NAD production.[28] The time-release form has a lower therapeutic index for lowering serum lipids relative to this form of toxicity.[29]
Diabetes
The high doses of niacin used to improve the lipid profile have been shown to elevate blood sugar by 5-10%, thereby worsening existing diabetes mellitus.[22] In a meta-analysis of 11 trials with non-diabetic participants, niacin therapy increased the relative risk of new-onset diabetes by 34%.[30]
Other
Side effects of heart arrhythmias have also been reported.[22] Increased prothrombin time and decreased platelet count have been reported; therefore, these should be monitored closely in patients who are also taking anticoagulants.[15]
Particularly the time-release variety, at extremely high doses, can cause acute toxic reactions.[31] Extremely high doses of niacin can also cause niacin maculopathy, a thickening of the macula and retina, which leads to blurred vision and blindness. This maculopathy is reversible after niacin intake ceases.[32]
Pregnancy
Niacin in doses used to lower cholesterol levels has been associated with birth defects in laboratory animals, with possible consequences for infant development in pregnant women.[22]
Deficiency

Between 1906 and 1940 more than 3 million Americans were affected by pellagra, with more than 100,000 deaths. Joseph Goldberger was assigned to study pellagra by the Surgeon General of the United States and produced good results. In the late 1930s, studies by Tom Spies, Marion Blankenhorn, and Clark Cooper established that niacin cured pellagra in humans. The disease was greatly reduced as a result.
At present, niacin deficiency is sometimes seen in developed countries, and it is usually apparent in conditions of poverty, malnutrition, and chronic alcoholism.[33] It also tends to occur in less developed areas where people eat maize (corn) as a staple food, as maize is the only grain low in digestible niacin. A cooking technique called nixtamalization i.e., pretreating with alkali ingredients, increases the bioavailability of niacin during maize meal/flour production. For this reason, people who consume corn as tortillas or hominy are not at risk of niacin deficiency.
Mild niacin deficiency has been shown to slow metabolism, causing decreased tolerance to cold.
Severe deficiency of niacin in the diet causes the disease pellagra, which is characterized by diarrhea, dermatitis, and dementia, as well as Casal's necklace lesions on the lower neck, hyperpigmentation, thickening of the skin, inflammation of the mouth and tongue, digestive disturbances, amnesia, delirium, and eventually death, if left untreated.[34] Common psychiatric symptoms of niacin deficiency include irritability, poor concentration, anxiety, fatigue, restlessness, apathy, and depression.[34] Studies have indicated that, in patients with alcoholic pellagra, niacin deficiency may be an important factor influencing both the onset and severity of this condition. Patients with alcoholism typically experience increased intestinal permeability, leading to negative health outcomes.
Hartnup disease is a hereditary nutritional disorder resulting in niacin deficiency.[34] This condition was first identified in the 1950s by the Hartnup family in London. It is due to a deficit in the intestines and kidneys, making it difficult for the body to break down and absorb dietary tryptophan (an essential amino acid that is utilized to synthesize niacin). The resulting condition is similar to pellagra, including symptoms of red, scaly rash, and sensitivity to sunlight. Oral niacin is given as a treatment for this condition in doses ranging from 40–200 mg, with a good prognosis if identified and treated early.[34] Niacin synthesis is also deficient in carcinoid syndrome, because of metabolic diversion of its precursor tryptophan to form serotonin.
Dietary recommendations
| Australia and New Zealand | ||
| Age group | RDI for niacin (mg NE/day)[35] | Upper level of intake[35] |
|---|---|---|
| Infants 0–6 months | 2 mg/d preformed niacin* | ND |
| Infants 7–12 months | 4 mg/d NE* | |
| 1–3 | 6 | 10 |
| 4–8 | 8 | 15 |
| 9–13 | 12 | 20 |
| 14–18 | - | 30 |
| 19+ | - | 35 |
| Females 14+ | 14 | - |
| Males 14+ | 16 | |
| Pregnant females 14–50 | 18 | - |
| Pregnant females 14–18 | - | 30 |
| Pregnant females 19–50 | - | 35 |
| Lactating females 14–50 | 17 | - |
| Lactating females 14–18 | - | 30 |
| Lactating females 19–50 | - | 35 |
| * Adequate Intake for infants[36] | ||
| Canada | ||
| Age group (years) | RDA of niacin (mg NE/d)[37] | Tolerable upper intake level[37] |
| 0–6 months | 2 mg/d preformed niacin* | ND |
| 7–12 months | 4 mg/d NE* | |
| 1–3 | 6 | 10 |
| 4–8 | 8 | 15 |
| 9–13 | 12 | 20 |
| Females 14–18 | 14 | 30 |
| Males 14–18 | 16 | |
| Females 19+ | 14 | 35 |
| Males 19+ | 16 | |
| Pregnant females <18 | 18 | 30 |
| Pregnant females 18–50 | 18 | 35 |
| Lactating females <18 | 17 | 30 |
| Lactating females 18–50 | 17 | 35 |
| European Food Safety Authority | ||
| Gender | Adequate Intake (mg NE/MJ)[38] | |
| Females | 1.3 | |
| Males | 1.6 | |
| Age (years) | Tolerable upper limit of Nicotinic acid (mg/day)[38] | Tolerable upper limit of Nicotinamide (mg/day)[38] |
| 1–3 | 2 | 150 |
| 4–6 | 3 | 220 |
| 7–10 | 4 | 350 |
| 11–14 | 6 | 500 |
| 15–17 | 8 | 700 |
| United States | ||
| Age group | RDA for niacin (mg NE/day) | Tolerable upper intake level[36] |
| Infants 0–6 months | 2* | ND** |
| Infants 6–12 months | 4* | |
| 1–3 years | 6 | 10 |
| 4–8 years | 8 | 15 |
| 9–13 years | 12 | 20 |
| Females 14–18 years | 14 | 30 |
| Males 14–18 years | 16 | 30 |
| Females 19+ years | 14 | 35 |
| Males 19+ years | 16 | 35 |
| Pregnant females 14–18 years | 18 | 30 |
| Pregnant females 19–50 years | 18 | 35 |
| Lactating females 14–18 years | 17 | 30 |
| Lactating females 19–50 years | 17 | 35 |
| * Adequate intake for infants, as an RDA has yet to be established ** Not possible to establish; source of intake should be formula and food only[36] | ||
The U.S. National Academy of Medicine (then the Institute of Medicine [IOM]) updated Estimated Average Requirements (EARs) and Recommended Dietary Allowances (RDAs) for B vitamins in 1998.
The European Food Safety Authority (EFSA) refers to the collective set of information as Dietary Reference Values (DRV), with Population Reference Intake (PRI) instead of RDA, and Average Requirement instead of EAR. AI and UL defined the same as in United States. For women (including those pregnant or lactating), men and children the PRI is 1.6 mg niacin per megajoule (MJ) of energy consumed. As the conversion is 1 MJ = 238.8 kcal, an adult consuming 2388 calories should be consuming 16 mg niacin. This is comparable to U.S. RDAs.[39] The niacin UL is set at 10 mg/day, which is much less than the U.S. value. The UL applies to niacin as a supplement consumed as one dose, and in intended to avoid the skin flush reaction. This explains why the PRI can be higher than the UL.[40]
Both the DRI and DRV describe amounts needed as niacin equivalents (NE), calculated as 1 mg NE = 1 mg niacin or 60 mg of the essential amino acid tryptophan. This is because the amino acid is utilized to synthesize the vitamin.[36][39]
For U.S. food and dietary supplement labeling purposes the amount in a serving is expressed as a percent of Daily Value (%DV). For niacin labeling purposes 100% of the Daily Value was 20 mg, but as of May 27, 2016 it was revised to 16 mg to bring it into agreement with the RDA.[41] A table of the old and new adult Daily Values is provided at Reference Daily Intake. The original deadline to be in compliance was July 28, 2018, but on September 29, 2017 the FDA released a proposed rule that extended the deadline to January 1, 2020 for large companies and January 1, 2021 for small companies.[42]
Food sources
Niacin is found in a variety of whole and processed foods, including fortified packaged foods, meat from various animal sources, seafoods, and spices.[43]
Among whole food sources with the highest niacin content per 100 grams:
- cooked skipjack tuna, 18.8 mg
- cooked light meat turkey, 11.8 mg
- cooked, lean ground pork, 11.1 mg
- cooked venison, 10.8 mg
- cooked, lean veal, 8.0 mg
Plant foods and spices
- sesame seed flour, 12.5 mg
- ground ginger, 9.6 mg
- dried tarragon, 9.0 mg
- dried, green sweet peppers, 7.4 mg
- grilled portobello mushrooms, 6.2 mg
- roasted sunflower seeds, 4.1 mg
- dehydrated apricots, 3.6 mg
- baked potato, 3.1 mg
Fortified breakfast cereals have among the highest niacin contents (more than 20 mg per 100 grams).[43] Whole grain flours, such as from wheat, rice, barley or corn, and pasta have niacin contents in a range of 3–10 mg per 100 grams.[43]
Pharmacology
Pharmacodynamics
The therapeutic effects of niacin are partly mediated through the activation of G protein-coupled receptors, including niacin receptor 1 (NIACR1) and niacin receptor 2 (NIACR2) which are highly expressed in adipose tissue, spleen, immune cells, and keratinocytes, but not in other expected organs such as liver, kidney, heart or intestine.[44][45] NIACR1 and NIACR2 inhibit cyclic adenosine monophosphate (cAMP) production and thus fat breakdown in adipose tissue and free fatty acids available for liver to produce triglycerides and very-low-density lipoproteins (VLDL) and consequently low-density lipoprotein (LDL).[28][46] A decrease in free fatty acids also suppresses liver expression of apolipoprotein C3 and PPARg coactivator-1b, thus increasing VLDL turnover and reducing its production.[47]
The mechanism behind niacin increasing HDL is not totally understood, but seems to occur in various ways. Niacin increases apolipoprotein A1 levels due to anticatabolic effects resulting in higher reverse cholesterol transport. It also inhibits HDL hepatic uptake, down-regulating production of the cholesterol ester transfer protein (CETP) gene.[48] Finally, it stimulates the ABCA1 transporter in monocytes and macrophages and upregulates peroxisome proliferator-activated receptor gamma, resulting in reverse cholesterol transport.[49]
Niacin reduces secondary outcomes associated with atherosclerosis, such as low-density lipoprotein cholesterol (LDL), very low-density lipoprotein cholesterol (VLDL-C), and triglycerides (TG), but increases high-density lipoprotein cholesterol (HDL).[48] Despite the importance of other cardiovascular risk factors, high HDL was associated with fewer cardiovascular events independent of LDL reduction.[50][51] Other effects include anti-thrombotic and vascular inflammation, improving endothelial function, and plaque stability.[52] As mediators produced from adipocytes, adipokines, such as tumor necrosis factor (TNF)-a, interleukins and chemokines, have pro-inflammatory effects, while others, such as adiponectin, have anti-inflammatory effects that influence the onset of atherosclerosis.[53] Niacin also appears to upregulate brain-derived neurotrophic factor and tropomyosin receptor kinase B (TrkB) expression.[54]
Research has been able to show the function of niacin in the pathway lipid metabolism. It is seen that this vitamin can decrease the synthesis of apoB-containing lipoproteins such as VLDL, LDL, IDL and lipoprotein (a) via several mechanisms: (1) directly inhibiting the action of DGAT2, a key enzyme for triglyceride synthesis; (2) influencing binding to the receptor HCAR2 thereby decreasing lipolysis and FFA flux to the liver for triglyceride synthesis; and (3) increasing apoB catabolism. HDL cholesterol levels are increased by niacin through direct and indirect pathways, such as by decreasing cholesterylester transfer protein activity and triglyceride levels, while increasing HDL cholesterol levels.[55]
Pharmacokinetics

Biosynthesis
The liver can synthesize niacin from the essential amino acid tryptophan, requiring 60 mg of tryptophan to make 1 mg of niacin. Riboflavin, vitamin B6 and iron are required for the process.[36]
Physical and chemical properties
Laboratory synthesis
Several thousand tons of niacin are manufactured each year, starting from 3-methylpyridine.
Preparations
Niacin is available as a prescription product, and in the United States as a dietary supplement. Prescription products can be immediate release (Niacor, 500 mg tablets) or extended release (Niaspan, 500 and 1000 mg tablets). Dietary supplement products can be immediate or slow release, the latter including inositol hexanicotinate.[56][57] The last has questionable clinical efficacy in reducing cholesterol levels.[58]
Nicotinamide
Nicotinamide may be obtained from the diet where it is present primarily as NAD+ and NADP+. These are hydrolysed in the intestine and the resulting nicotinamide is absorbed either as such, or following its hydrolysis to nicotinic acid. Nicotinamide is present in nature in only small amounts, however it is the main form of vitamin B3 in plasma. In unprepared foods, niacin is present mainly in the form of the cellular pyridine nucleotides NAD and NADP. Enzymatic hydrolysis of the co-enzymes can occur during the course of food preparation. Boiling releases most of the total niacin present in sweet corn as nicotinamide (up to 55 mg/kg).
Nicotinamide may be toxic to the liver at doses exceeding 3 g/day for adults.[59]
Extended release
A prescription extended release niacin, Niaspan, has a film coating that delays release of the niacin, resulting in an absorption over a period of 8–12 hours. The extended release formulations generally reduce vasodilation and flushing side effects, but increase the risk of hepatotoxicity compared to the immediate release forms.[60][61]
A formulation of laropiprant (Merck & Co., Inc.) and niacin had previously been approved for use in Europe and marketed as Tredaptive. Laropiprant is a prostaglandin D2 binding drug shown to reduce vasodilatation and flushing up to 73%.[48][62][63][64] The HPS2-THRIVE study,[65] a study sponsored by Merck, showed no additional efficacy of Tredaptive in lowering cholesterol when used together with other statin drugs, but did show an increase in other side effects. The study resulted in the complete withdrawal of Tredaptive from the international market.[66][67][68]
Inositol hexanicotinate
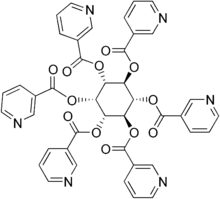
One form of dietary supplement is inositol hexanicotinate (IHN), which is inositol that has been esterified with niacin on all six of inositol's alcohol groups.[69] IHN is usually sold as "flush-free" or "no-flush" niacin in units of 250, 500, or 1000 mg/tablets or capsules. It is sold as an over-the-counter formulation, and often is marketed and labeled as niacin, thus misleading consumers into thinking they are getting the active form of the medication. While this form of niacin does not cause the flushing associated with the immediate-release products, the evidence that it has lipid-modifying functions is disputed. As the clinical trials date from the early 1960s (Dorner, Welsh) or the late 1970s (Ziliotto, Kruse, Agusti), it is difficult to assess them by today's standards.[70] One of the last of those studies affirmed the superiority of inositol and xantinol esters of nicotinic acid for reducing serum free fatty acid,[71] but other studies conducted during the same period found no benefit.[72] Studies explain that this is primarily because "flush-free" preparations do not contain any free nicotinic acid. A more recent placebo-controlled trial was small (n=11/group), but results after three months at 1500 mg/day showed no trend for improvements in total cholesterol, LDL-C, HDL-C or triglycerides.[73] Thus, so far there is not enough evidence to recommend IHN to treat dyslipidemia.
Rename
In 1942, when flour enrichment with nicotinic acid began, a headline in the popular press said "Tobacco in Your Bread." So the Council on Foods and Nutrition of the American Medical Association approved of the Food and Nutrition Board's new names niacin and niacin amide for use primarily by non-scientists. It was thought appropriate to choose a name to dissociate it from nicotine, to avoid the perception that vitamins or niacin-rich food contains nicotine, or that cigarettes contain vitamins.[74] The resulting name niacin was derived from nicotinic acid + vitamin.[75][76]
History
Niacin was first described by chemist Hugo Weidel in 1873 in his studies of nicotine.[77] The original preparation remains useful: the oxidation of nicotine using nitric acid.[78] For the first time, niacin was extracted by Casimir Funk, but he thought that it was thiamine and due to the discovered amine group he coined the term "vitamine". Niacin was extracted from livers by biochemist Conrad Elvehjem in 1937, who later identified the active ingredient, then referred to as the "pellagra-preventing factor" and the "anti-blacktongue factor."[79] Soon after, in studies conducted in Alabama and Cincinnati, Dr. Tom Spies found that nicotinic acid cured the sufferers of pellagra.[80]
Niacin is referred to as vitamin B3 because it was the third of the B vitamins to be discovered. It has historically been referred to as "vitamin PP", "vitamin P-P" and "PP-factor", that are derived from the term "pellagra-preventive factor".[75] Carpenter found in 1951 that niacin in corn is biologically unavailable, and can be released only in very alkaline lime water of pH 11.[81] In 1955, Altschul and colleagues described niacin as having a lipid-lowering property.[82] As such, niacin is the oldest lipid-lowering drug.
Research
In animal models and in vitro, niacin produces marked anti-inflammatory effects in a variety of tissues – including the brain, gastrointestinal tract, skin, and vascular tissue – through the activation of NIACR1.[83][84][85][86] Niacin has been shown to attenuate neuroinflammation and may have efficacy in treating neuroimmune disorders such as multiple sclerosis and Parkinson's disease.[83][86] Unlike niacin, nicotinamide does not activate NIACR1; however, both niacin and nicotinamide activate the G protein-coupled estrogen receptor (GPER) in vitro.[87]
In 2014, concurring with earlier work in 2001 by Arizona State University, researchers from Pennsylvania State University working with NASA found niacin, pyridine carboxylic acids and pyridine dicarboxylic acids inside meteorites.[88]
References
- ↑ Nomenclature of Organic Chemistry : IUPAC Recommendations and Preferred Names 2013 (Blue Book). Cambridge: The Royal Society of Chemistry. 2014. pp. 747, 750. doi:10.1039/9781849733069-FP001. ISBN 978-0-85404-182-4.
- ↑ "Why fortify?". Food Fortification Initiative. 2017. Retrieved 4 April 2017.
- ↑ Cox M, Lehninger AL, Nelson DR (2000). Lehninger principles of biochemistry. New York: Worth Publishers. ISBN 1-57259-153-6.
- 1 2 Wan P, Moat S, Anstey A (June 2011). "Pellagra: a review with emphasis on photosensitivity". The British Journal of Dermatology. 164 (6): 1188–200. doi:10.1111/j.1365-2133.2010.10163.x. PMID 21128910.
- ↑ Ishii N, Nishihara Y (March 1981). "Pellagra among chronic alcoholics: clinical and pathological study of 20 necropsy cases". Journal of Neurology, Neurosurgery, and Psychiatry. 44 (3): 209–15. doi:10.1136/jnnp.44.3.209. PMC 490893. PMID 7229643.
- 1 2 Keene D, Price C, Shun-Shin MJ, Francis DP (July 2014). "Effect on cardiovascular risk of high density lipoprotein targeted drug treatments niacin, fibrates, and CETP inhibitors: meta-analysis of randomised controlled trials including 117,411 patients". BMJ. 349: g4379. doi:10.1136/bmj.g4379. PMC 4103514. PMID 25038074.
- ↑ Bruckert E, Labreuche J, Amarenco P (June 2010). "Meta-analysis of the effect of nicotinic acid alone or in combination on cardiovascular events and atherosclerosis". Atherosclerosis. 210 (2): 353–61. doi:10.1016/j.atherosclerosis.2009.12.023. PMID 20079494.
- ↑ Jaconello P (October 1992). "Niacin versus niacinamide". CMAJ. 147 (7): 990. PMC 1336277. PMID 1393911.
- ↑ Kennedy DO (January 2016). "B Vitamins and the Brain: Mechanisms, Dose and Efficacy--A Review". Nutrients. 8 (2): 68. doi:10.3390/nu8020068. PMC 4772032. PMID 26828517.
- ↑ Kirkland JB (May 2012). "Niacin requirements for genomic stability". Mutation Research. 733 (1–2): 14–20. doi:10.1016/j.mrfmmm.2011.11.008. PMID 22138132.
- ↑ "Niacin and niacinamide (Vitamin B3)". MedlinePlus, US National Library of Medicine, National Institutes of Health. 2016. Retrieved 12 October 2016.
- ↑ Niacin tablet label Updated March 14, 2013. Page accessed Feb 11, 2016
- ↑ Schandelmaier S, Briel M, Saccilotto R, Olu KK, Arpagaus A, Hemkens LG, Nordmann AJ (June 2017). "Niacin for primary and secondary prevention of cardiovascular events". The Cochrane Database of Systematic Reviews. 6: CD009744. doi:10.1002/14651858.CD009744.pub2. PMID 28616955.
- ↑ Garg A, Sharma A, Krishnamoorthy P, Garg J, Virmani D, Sharma T, Stefanini G, Kostis JB, Mukherjee D, Sikorskaya E (February 2017). "Role of Niacin in Current Clinical Practice: A Systematic Review". The American Journal of Medicine. 130 (2): 173–187. doi:10.1016/j.amjmed.2016.07.038. PMID 27793642.
- 1 2 3 Kos Pharmaceuticals Inc. Niaspan® (niacin extended-release) tablets prescribing information. Cranbury, NJ; 2005 Oct.
- 1 2 Bays HE, Rader DJ (January 2009). "Does nicotinic acid (niacin) lower blood pressure?". International Journal of Clinical Practice. 63 (1): 151–9. doi:10.1111/j.1742-1241.2008.01934.x. PMC 2705821. PMID 19054161.
- ↑ "Guidelines for Niacin Therapy For the Treatment of Elevated Lipoprotein a (Lpa)" (PDF). Rush Hemophilia & Thrombophilia Center. 27 July 2005 [15 August 2002]. Retrieved 20 November 2009.
facial flushing is a common side effect of niacin therapy that usually subsides after several weeks of consistent niacin use
- ↑ Kamanna VS, Kashyap ML (April 2008). "Mechanism of action of niacin". The American Journal of Cardiology. 101 (8A): 20B–26B. doi:10.1016/j.amjcard.2008.02.029. PMID 18375237.
- ↑ Katzung, Bertram G. (2006). Basic and clinical pharmacology. New York: McGraw-Hill Medical Publishing Division. ISBN 0-07-145153-6.
- ↑ Barter, P (2006). "Options for therapeutic intervention: How effective are the different agents?". European Heart Journal Supplements. 8 (F): F47–F53. doi:10.1093/eurheartj/sul041.
- ↑ Chapman MJ, Assmann G, Fruchart JC, Shepherd J, Sirtori C (August 2004). "Raising high-density lipoprotein cholesterol with reduction of cardiovascular risk: the role of nicotinic acid--a position paper developed by the European Consensus Panel on HDL-C". Current Medical Research and Opinion. 20 (8): 1253–68. doi:10.1185/030079904125004402. PMID 15324528.
- 1 2 3 4 Brunton LL, Lazo JS, Parker K, eds. (2005). Goodman & Gilman's The Pharmacological Basis of Therapeutics (11th ed.). New York: McGraw-Hill. ISBN 0-07-142280-3.
- 1 2 Papaliodis D, Boucher W, Kempuraj D, Michaelian M, Wolfberg A, House M, Theoharides TC (December 2008). "Niacin-induced "flush" involves release of prostaglandin D2 from mast cells and serotonin from platelets: evidence from human cells in vitro and an animal model". The Journal of Pharmacology and Experimental Therapeutics. 327 (3): 665–72. doi:10.1124/jpet.108.141333. PMID 18784348.
- ↑ Benyó Z, Gille A, Kero J, Csiky M, Suchánková MC, Nüsing RM, Moers A, Pfeffer K, Offermanns S (December 2005). "GPR109A (PUMA-G/HM74A) mediates nicotinic acid-induced flushing". The Journal of Clinical Investigation. 115 (12): 3634–40. doi:10.1172/JCI23626. PMC 1297235. PMID 16322797.
- ↑ Benyó Z, Gille A, Bennett CL, Clausen BE, Offermanns S (December 2006). "Nicotinic acid-induced flushing is mediated by activation of epidermal langerhans cells". Molecular Pharmacology. 70 (6): 1844–9. doi:10.1124/mol.106.030833. PMID 17008386.
- ↑ Hanson J, Gille A, Zwykiel S, Lukasova M, Clausen BE, Ahmed K, Tunaru S, Wirth A, Offermanns S (August 2010). "Nicotinic acid- and monomethyl fumarate-induced flushing involves GPR109A expressed by keratinocytes and COX-2-dependent prostanoid formation in mice". The Journal of Clinical Investigation. 120 (8): 2910–9. doi:10.1172/JCI42273. PMC 2912194. PMID 20664170.
- ↑ Maciejewski-Lenoir D, Richman JG, Hakak Y, Gaidarov I, Behan DP, Connolly DT (December 2006). "Langerhans cells release prostaglandin D2 in response to nicotinic acid". The Journal of Investigative Dermatology. 126 (12): 2637–46. doi:10.1038/sj.jid.5700586. PMID 17008871.
- 1 2 Gille A, Bodor ET, Ahmed K, Offermanns S (2008). "Nicotinic acid: pharmacological effects and mechanisms of action". Annual Review of Pharmacology and Toxicology. 48 (1): 79–106. doi:10.1146/annurev.pharmtox.48.113006.094746. PMID 17705685.
- ↑ Rader JI, Calvert RJ, Hathcock JN (January 1992). "Hepatic toxicity of unmodified and time-release preparations of niacin". The American Journal of Medicine. 92 (1): 77–81. doi:10.1016/0002-9343(92)90018-7. PMID 1731514.
- ↑ Goldie C, Taylor AJ, Nguyen P, McCoy C, Zhao XQ, Preiss D (February 2016). "Niacin therapy and the risk of new-onset diabetes: a meta-analysis of randomised controlled trials". Heart. 102 (3): 198–203. doi:10.1136/heartjnl-2015-308055. PMC 4752613. PMID 26370223.
- ↑ Mittal MK, Florin T, Perrone J, Delgado JH, Osterhoudt KC (November 2007). "Toxicity from the use of niacin to beat urine drug screening". Annals of Emergency Medicine. 50 (5): 587–90. doi:10.1016/j.annemergmed.2007.01.014. PMID 17418450.
- ↑ Gass JD (December 2003). "Nicotinic acid maculopathy. 1973". Retina. 23 (6 Suppl): 500–10. PMID 15035390.
- ↑ Pitsavas S, Andreou C, Bascialla F, Bozikas VP, Karavatos A (2004). "Pellagra encephalopathy following B-complex vitamin treatment without niacin". International Journal of Psychiatry in Medicine. 34 (1): 91–5. doi:10.2190/29XV-1GG1-U17K-RGJH. PMID 15242145.
- 1 2 3 4 Prakash R, Gandotra S, Singh LK, Das B, Lakra A (2008). "Rapid resolution of delusional parasitosis in pellagra with niacin augmentation therapy". General Hospital Psychiatry. 30 (6): 581–4. doi:10.1016/j.genhosppsych.2008.04.011. PMID 19061687.
- 1 2 "Nutrient reference values for Australia and New Zealand" (PDF). National Health and Medical Research Council. September 9, 2005. Retrieved June 19, 2018.
- 1 2 3 4 5 Institute of Medicine (1998). "Niacin". Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, DC: The National Academies Press. pp. 123–149. ISBN 0-309-06554-2. Retrieved 2018-08-29.
- 1 2 Health Canada. "Dietary Reference Intakes". Government of Canada. Retrieved June 20, 2018.
- 1 2 3 European Food Safety Authority (February 2006). "Tolerable Upper Intake Levels for Vitamins and Minerals" (PDF). EFSA. Retrieved June 18, 2018.
- 1 2 "Overview on Dietary Reference Values for the EU population as derived by the EFSA Panel on Dietetic Products, Nutrition and Allergies" (PDF). 2017.
- ↑ "Tolerable Upper Intake Levels For Vitamins And Minerals" (PDF). European Food Safety Authority. 2006.
- ↑ "Federal Register May 27, 2016 Food Labeling: Revision of the Nutrition and Supplement Facts Labels" (PDF).
- ↑ "Changes to the Nutrition Facts Panel - Compliance Date"
- 1 2 3 "Niacin content per 100 grams; select food subset, abridged list by food groups". United States Department of Agriculture, Agricultural Research Service, USDA Branded Food Products Database v.3.6.4.1. 17 January 2017. Retrieved 23 January 2017.
- ↑ Soga T, Kamohara M, Takasaki J, Matsumoto S, Saito T, Ohishi T, Hiyama H, Matsuo A, Matsushime H, Furuichi K (March 2003). "Molecular identification of nicotinic acid receptor". Biochemical and Biophysical Research Communications. 303 (1): 364–9. doi:10.1016/S0006-291X(03)00342-5. PMID 12646212.
- ↑ Wise A, Foord SM, Fraser NJ, Barnes AA, Elshourbagy N, Eilert M, Ignar DM, Murdock PR, Steplewski K, Green A, Brown AJ, Dowell SJ, Szekeres PG, Hassall DG, Marshall FH, Wilson S, Pike NB (March 2003). "Molecular identification of high and low affinity receptors for nicotinic acid". The Journal of Biological Chemistry. 278 (11): 9869–74. doi:10.1074/jbc.M210695200. PMID 12522134.
- ↑ Wanders D, Judd RL (August 2011). "Future of GPR109A agonists in the treatment of dyslipidaemia". Diabetes, Obesity & Metabolism. 13 (8): 685–91. doi:10.1111/j.1463-1326.2011.01400.x. PMID 21418500.
- ↑ Hernandez C, Molusky M, Li Y, Li S, Lin JD (October 2010). "Regulation of hepatic ApoC3 expression by PGC-1β mediates hypolipidemic effect of nicotinic acid". Cell Metabolism. 12 (4): 411–9. doi:10.1016/j.cmet.2010.09.001. PMC 2950832. PMID 20889132.
- 1 2 3 Villines TC, Kim AS, Gore RS, Taylor AJ (February 2012). "Niacin: the evidence, clinical use, and future directions". Current Atherosclerosis Reports. 14 (1): 49–59. doi:10.1007/s11883-011-0212-1. PMID 22037771.
- ↑ Rubic T, Trottmann M, Lorenz RL (February 2004). "Stimulation of CD36 and the key effector of reverse cholesterol transport ATP-binding cassette A1 in monocytoid cells by niacin". Biochemical Pharmacology. 67 (3): 411–9. doi:10.1016/j.bcp.2003.09.014. PMID 15037193.
- ↑ Barter P, Gotto AM, LaRosa JC, Maroni J, Szarek M, Grundy SM, Kastelein JJ, Bittner V, Fruchart JC (September 2007). "HDL cholesterol, very low levels of LDL cholesterol, and cardiovascular events". The New England Journal of Medicine. 357 (13): 1301–10. doi:10.1056/NEJMoa064278. PMID 17898099.
- ↑ Jafri H, Alsheikh-Ali AA, Karas RH (December 2010). "Meta-analysis: statin therapy does not alter the association between low levels of high-density lipoprotein cholesterol and increased cardiovascular risk". Annals of Internal Medicine. 153 (12): 800–8. doi:10.7326/0003-4819-153-12-201012210-00006. PMID 21173414.
- ↑ Wu BJ, Yan L, Charlton F, Witting P, Barter PJ, Rye KA (May 2010). "Evidence that niacin inhibits acute vascular inflammation and improves endothelial dysfunction independent of changes in plasma lipids". Arteriosclerosis, Thrombosis, and Vascular Biology. 30 (5): 968–75. doi:10.1161/ATVBAHA.109.201129. PMID 20167660.
- ↑ Gustafson B (April 2010). "Adipose tissue, inflammation and atherosclerosis". Journal of Atherosclerosis and Thrombosis. 17 (4): 332–41. doi:10.5551/jat.3939. PMID 20124732.
- ↑ Fu L, Doreswamy V, Prakash R (August 2014). "The biochemical pathways of central nervous system neural degeneration in niacin deficiency". Neural Regeneration Research. 9 (16): 1509–13. doi:10.4103/1673-5374.139475. PMC 4192966. PMID 25317166.
- ↑ Creider JC, Hegele RA, Joy TR (September 2012). "Niacin: another look at an underutilized lipid-lowering medication". Nature Reviews. Endocrinology. 8 (9): 517–28. doi:10.1038/nrendo.2012.22. PMID 22349076.
- ↑ Dunatchik AP, Ito MK, Dujovne CA (2012-03-01). "A systematic review on evidence of the effectiveness and safety of a wax-matrix niacin formulation". Journal of Clinical Lipidology. 6 (2): 121–31. doi:10.1016/j.jacl.2011.07.003. PMID 22385545.
- ↑ Meyers CD, Carr MC, Park S, Brunzell JD (December 2003). "Varying cost and free nicotinic acid content in over-the-counter niacin preparations for dyslipidemia". Annals of Internal Medicine. 139 (12): 996–1002. doi:10.7326/0003-4819-139-12-200312160-00009. PMID 14678919.
- ↑ Keenan JM (2013-01-01). "Wax-matrix extended-release niacin vs inositol hexanicotinate: a comparison of wax-matrix, extended-release niacin to inositol hexanicotinate "no-flush" niacin in persons with mild to moderate dyslipidemia". Journal of Clinical Lipidology. 7 (1): 14–23. doi:10.1016/j.jacl.2012.10.004. PMID 23351578.
- ↑ Knip M, Douek IF, Moore WP, Gillmor HA, McLean AE, Bingley PJ, Gale EA (November 2000). "Safety of high-dose nicotinamide: a review". Diabetologia. 43 (11): 1337–45. doi:10.1007/s001250051536. PMID 11126400.
- ↑ Bassan M (2012). "A case for immediate-release niacin". Heart & Lung. 41 (1): 95–8. doi:10.1016/j.hrtlng.2010.07.019. PMID 21414665.
- ↑ Reiche I, Westphal S, Martens-Lobenhoffer J, Tröger U, Luley C, Bode-Böger SM (January 2011). "Pharmacokinetics and dose recommendations of Niaspan® in chronic kidney disease and dialysis patients". Nephrology, Dialysis, Transplantation. 26 (1): 276–82. doi:10.1093/ndt/gfq344. PMID 20562093.
- ↑ Lai E, De Lepeleire I, Crumley TM, Liu F, Wenning LA, Michiels N, Vets E, O'Neill G, Wagner JA, Gottesdiener K (June 2007). "Suppression of niacin-induced vasodilation with an antagonist to prostaglandin D2 receptor subtype 1". Clinical Pharmacology and Therapeutics. 81 (6): 849–57. doi:10.1038/sj.clpt.6100180. PMID 17392721.
- ↑ Paolini JF, Bays HE, Ballantyne CM, Davidson M, Pasternak R, Maccubbin D, Norquist JM, Lai E, Waters MG, Kuznetsova O, Sisk CM, Mitchel YB (November 2008). "Extended-release niacin/laropiprant: reducing niacin-induced flushing to better realize the benefit of niacin in improving cardiovascular risk factors". Cardiology Clinics. 26 (4): 547–60. doi:10.1016/j.ccl.2008.06.007. PMID 19031552.
- ↑ Kamanna VS, Vo A, Kashyap ML (July 2008). "Nicotinic acid: recent developments". Current Opinion in Cardiology. 23 (4): 393–8. doi:10.1097/HCO.0b013e3283021c82. PMID 18520725. .
- ↑ "Treatment of HDL to Reduce the Incidence of Vascular Events HPS2-THRIVE - Full Text View - ClinicalTrials.gov". clinicaltrials.gov. Retrieved 2017-02-20.
- ↑ Medscape: Medscape Access
- ↑ Nainggolan L (2013-01-11). "Niacin/Laropiprant Products to Be Suspended Worldwide". Medscape. Retrieved 2017-02-20.
- ↑ "Merck begins overseas recall of HDL cholesterol drug". Reuters. 11 January 2013.
- ↑ Aguilar F, Charrondiere UR, Dusemund B, Galtier PM, Gilbert J, Gott DM, et al. (2009). "Inositol hexanicotinate (inositol hexaniacinate) as a source of niacin (vitamin B3) added for nutritional purposes in food supplements". The EFSA Journal. 949: 1–20.
- ↑ Taheri, R (15 January 2003). "No-Flush Niacin for the Treatment of Hyperlipidemia". Medscape. Retrieved 31 March 2008.
- ↑ Kruse W, Raetzer H, Heuck CC, Oster P, Schellenberg B, Schlierf G (August 1979). "Nocturnal inhibition of lipolysis in man by nicotinic acid and derivatives". European Journal of Clinical Pharmacology. 16 (1): 11–5. doi:10.1007/BF00644960. PMID 499296.
- ↑ Meyers CD, Carr MC, Park S, Brunzell JD (December 2003). "Varying cost and free nicotinic acid content in over-the-counter niacin preparations for dyslipidemia". Annals of Internal Medicine. 139 (12): 996–1002. CiteSeerX 10.1.1.694.2773. doi:10.7326/0003-4819-139-12-200312160-00009. PMID 14678919.
- ↑ Benjó AM, Maranhão RC, Coimbra SR, Andrade AC, Favarato D, Molina MS, Brandizzi LI, da Luz PL (July 2006). "Accumulation of chylomicron remnants and impaired vascular reactivity occur in subjects with isolated low HDL cholesterol: effects of niacin treatment". Atherosclerosis. 187 (1): 116–22. doi:10.1016/j.atherosclerosis.2005.08.025. PMID 16458316.
- ↑ "Niacin and Nicotinic Acid". Journal of the American Medical Association. American Medical Association. 118 (10): 823. March 7, 1942. doi:10.1001/jama.1942.02830100053014. Retrieved May 7, 2016.
- 1 2 "Pellagra And Its Prevention And Control In Major Emergencies" (PDF). World Health Organization. World Health Organization. Retrieved 17 April 2015.
- ↑ "Niacin and Niacin Amide". Journal of the American Medical Association. American Medical Association. 118 (10): 819. March 7, 1942. doi:10.1001/jama.1942.02830100049011. Retrieved May 7, 2016.
- ↑ Weidel, H (1873). "Zur Kenntniss des Nicotins". Justus Liebigs Annalen der Chemie und Pharmacie. 165 (2): 330–349. doi:10.1002/jlac.18731650212.
- ↑ Samuel M. McElvain (1941). "Nicotinic Acid" (PDF). Organic Syntheses. ; Collective Volume, 1, p. 385
- ↑ Elvehjem CA, Madden RJ, Strongandd FM, Woolley DW (1938). "The isolation and identification of the anti-blacktongue factor J" (PDF). J. Biol. Chem. 123 (1): 137–149.
- ↑ Kraut A. "Dr. Joseph Goldberger and the War on Pellagra | Ashes on the Potomac". history.nih.gov. Retrieved 2017-02-20.
- ↑ Laguna J, Carpenter KJ (September 1951). "Raw versus processed corn in niacin-deficient diets". The Journal of Nutrition. 45 (1): 21–8. doi:10.1093/jn/45.1.21. PMID 14880960.
- ↑ Altschul R, Hoffer A, Stephen JD (February 1955). "Influence of nicotinic acid on serum cholesterol in man". Archives of Biochemistry and Biophysics. 54 (2): 558–9. doi:10.1016/0003-9861(55)90070-9. PMID 14350806.
- 1 2 Offermanns S, Schwaninger M (April 2015). "Nutritional or pharmacological activation of HCA(2) ameliorates neuroinflammation". Trends in Molecular Medicine. 21 (4): 245–55. doi:10.1016/j.molmed.2015.02.002. PMID 25766751.
Neuroinflammatory cells express HCA2, a receptor for the endogenous neuroprotective ketone body β-hydroxybutyrate (BHB) as well as for the drugs dimethyl fumarate (DMF) and nicotinic acid, which have established efficacy in the treatment of MS and experimental stroke, respectively. This review summarizes the evidence that HCA2 is involved in the therapeutic effects of DMF, nicotinic acid, and ketone bodies in reducing neuroinflammation.
- ↑ Chai JT, Digby JE, Choudhury RP (May 2013). "GPR109A and vascular inflammation". Current Atherosclerosis Reports. 15 (5): 325. doi:10.1007/s11883-013-0325-9. PMC 3631117. PMID 23526298.
As GPR109A's primary pharmacological ligand in clinical use, niacin has been used for over 50 years in the treatment of cardiovascular disease, mainly due to its favourable effects on plasma lipoproteins.
- ↑ Graff EC, Fang H, Wanders D, Judd RL (February 2016). "Anti-inflammatory effects of the hydroxycarboxylic acid receptor 2". Metabolism. 65 (2): 102–13. doi:10.1016/j.metabol.2015.10.001. PMID 26773933.
HCA2 is highly expressed on immune cells, including macrophages, monocytes, neutrophils and dermal dendritic cells, among other cell types. ... Recent studies demonstrate that HCA2 mediates profound anti-inflammatory effects in a variety of tissues.
- 1 2 Wakade C, Chong R (December 2014). "A novel treatment target for Parkinson's disease". Journal of the Neurological Sciences. 347 (1–2): 34–8. doi:10.1016/j.jns.2014.10.024. PMID 25455298.
- ↑ Santolla MF, De Francesco EM, Lappano R, Rosano C, Abonante S, Maggiolini M (July 2014). "Niacin activates the G protein estrogen receptor (GPER)-mediated signalling". Cellular Signalling. 26 (7): 1466–75. doi:10.1016/j.cellsig.2014.03.011. PMID 24662263.
- ↑ "Vitamin B3 Might Have Been Made in Space, Delivered to Earth by Meteorites". NASA. April 17, 2014. Retrieved April 27, 2018.