Nicotine
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Nicorette, Nicotrol |
| AHFS/Drugs.com | Monograph |
| Pregnancy category | |
| Dependence liability |
Physical: low–moderate Psychological: moderate–high[1][2] |
| Addiction liability | High[3] |
| Routes of administration | Inhalation; insufflation; oral – buccal, sublingual, and ingestion; transdermal; rectal |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Protein binding | <5% |
| Metabolism | Primarily hepatic: CYP2A6, CYP2B6, FMO3, others |
| Metabolites | Cotinine |
| Elimination half-life | 1-2 hours; 20 hours active metabolite |
| Excretion | Urine (10-20% (gum), pH-dependent; 30% (inhaled); 10-30% (intranasal)) |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| ECHA InfoCard |
100.152.478 |
| Chemical and physical data | |
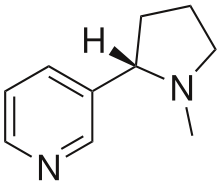
| Formula | C10H14N2 |
| Molar mass | 162.23 g/mol |
| 3D model (JSmol) | |
| Chirality | Chiral |
| Density | 1.01 g/cm3 |
| Melting point | −79 °C (−110 °F) |
| Boiling point | 247 °C (477 °F) |
| |
| |
| | |
Nicotine is a potent parasympathomimetic stimulant and an alkaloid found in the nightshade family of plants. Nicotine acts as an agonist at most nicotinic acetylcholine receptors (nAChRs),[4][5] except at two nicotinic receptor subunits (nAChRα9 and nAChRα10) where it acts as a receptor antagonist.[4] Nicotine is found in the leaves of Nicotiana rustica, in concentrations of 2–14%; in the tobacco plant, Nicotiana tabacum; in Duboisia hopwoodii; and in Asclepias syriaca.[6]
Nicotine constitutes approximately 0.6–3.0% of the dry weight of tobacco.[7] It also occurs in edible plants, such as those in the family Solanaceae, which include eggplants, potatoes, and tomatoes for example, but at trace levels generally under 200 nanograms per gram, dry weight (less than .00002%).[8][9][10] Nicotine functions as an antiherbivore chemical; consequently, nicotine was widely used as an insecticide in the past,[11][12] and neonicotinoids, such as imidacloprid, are widely used.
Nicotine is highly addictive.[13][14] An average cigarette yields about 2 mg of absorbed nicotine; in lesser doses of that order, the substance acts as a stimulant in mammals, while high amounts (50–100 mg) can be harmful.[15][16][17] Nicotine addiction and dependence involves drug-reinforced behavior, compulsive use, relapse after abstinence, physical dependence, psychological dependence, and drug tolerance.[1][2][18]
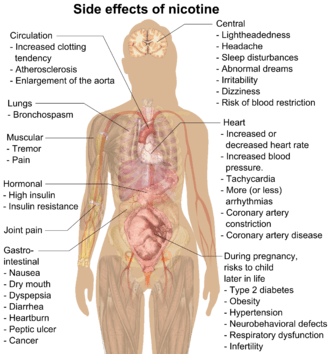
Beyond addiction, both short and long-term nicotine exposure have not been established as dangerous to adults,[19] except among certain vulnerable groups.[20] At sufficiently high doses, nicotine is associated with poisonings and is potentially lethal.[17][21] Nicotine as a tool for quitting smoking has a good safety history.[22] There is inadequate research to show that nicotine itself is associated with cancer in humans.[21] Nicotine in the form of nicotine replacement products poses less of a cancer risk than smoking.[21] Nicotine is linked to possible birth defects.[23] If exposed to nicotine during pregnancy, a child may have an increased risk later in life of type 2 diabetes, obesity, hypertension, neurobehavioral defects, respiratory dysfunction, and infertility.[22] The use of electronic cigarettes, which are designed to be refilled with nicotine-containing e-liquid, has raised concerns over nicotine overdoses, especially with regard to the possibility of young children ingesting the liquids.[24]
Psychoactive effects
Nicotine's mood-altering effects are different by report: in particular it is both a stimulant and a relaxant.[25] First causing a release of glucose from the liver and epinephrine (adrenaline) from the adrenal medulla, it causes stimulation. Users report feelings of relaxation, sharpness, calmness, and alertness.[26]
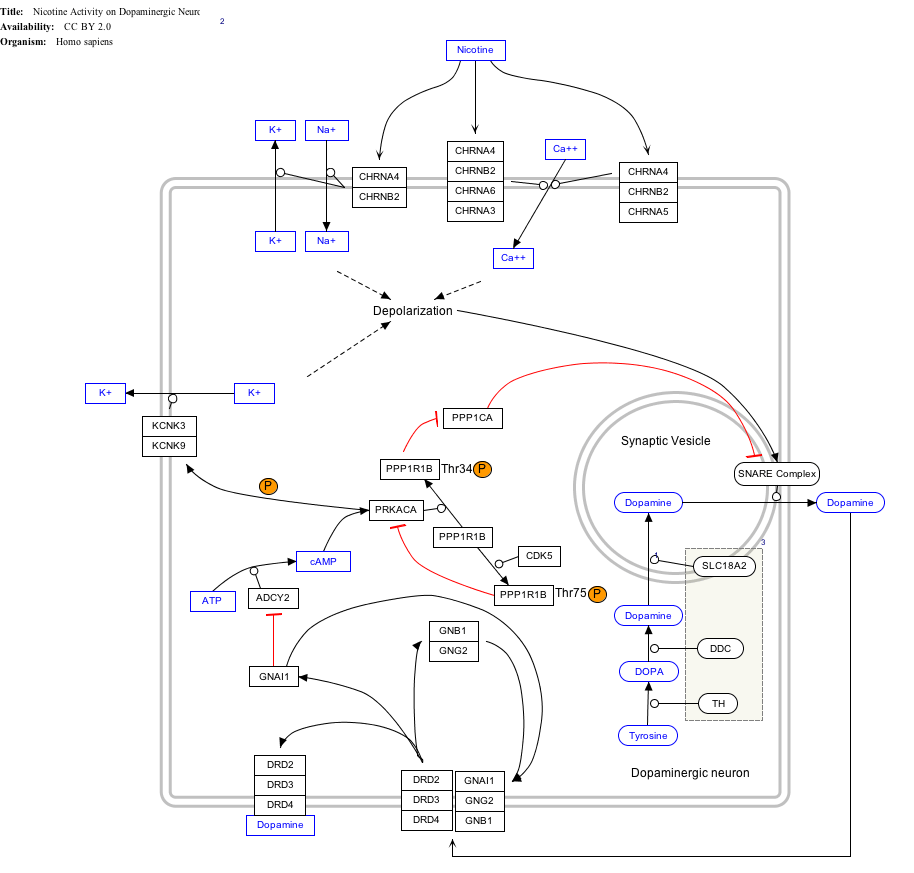
When a cigarette is smoked, nicotine-rich blood passes from the lungs to the brain within seven seconds and immediately stimulates nicotinic acetylcholine receptors;[27] this indirectly promotes the release of many chemical messengers such as acetylcholine, norepinephrine, epinephrine, arginine vasopressin, serotonin, dopamine, and beta-endorphin in parts of the brain.[27][28] Nicotine also extends the duration of positive effects of dopamine and increases the sensitivity of the brain's reward system to rewarding stimuli.[29][30] Most cigarettes contain 1–3 milligrams of inhalable nicotine.[31] Studies suggest that when smokers wish to achieve a stimulating effect, they take short quick puffs, which produce a low level of blood nicotine.[32]
Nicotine is unusual in comparison to most drugs, as its profile changes from stimulant to sedative with increasing dosages, a phenomenon known as "Nesbitt's paradox" after the doctor who first described it in 1969.[33][34] At very high doses it dampens neuronal activity.[35]
Uses
Medical
The primary therapeutic use of nicotine is in treating nicotine dependence in order to eliminate smoking with the damage it does to health. Controlled levels of nicotine are given to patients through gums, dermal patches, lozenges, electronic/substitute cigarettes or nasal sprays in an effort to wean them off their dependence. Studies have found that these therapies increase the chance of success of quitting by 50 to 70%,[36] though reductions in the population as a whole have not been demonstrated.[37]
Enhancing performance
Nicotine is frequently used for its performance-enhancing effects on cognition, alertness, and focus.[38] A meta-analysis of 41 double-blind, placebo-controlled studies concluded that nicotine or smoking had significant positive effects on aspects of fine motor abilities, alerting and orienting attention, and episodic and working memory.[39] A 2015 review noted that stimulation of the α4β2 nicotinic receptor is responsible for certain improvements in attentional performance;[40] among the nicotinic receptor subtypes, nicotine has the highest binding affinity at the α4β2 receptor (ki=1 nM), which is also the biological target that mediates nicotine's addictive properties.[41] Nicotine has potential beneficial effects, but it also has paradoxical effects, which may be due to its inverted U-shape or pharmacokinetic features.[42]
Recreational
Nicotine is commonly consumed as a recreational drug for its stimulant effects.[43] Recreational nicotine products include chewing tobacco, cigars, cigarettes, e-cigarettes, snuff, pipe tobacco, and snus.
Adverse effects
Limited data exists on the health effects of long-term use of pure nicotine, because nicotine is usually consumed via tobacco products.[44] The long-term use of nicotine in the form of snus incurs a slight risk of cardiovascular disease compared to tobacco smoking.[44] Nicotine is one of the most rigorously studied drugs.[45] The complex effects of nicotine are not entirely understood.[23] Studies of continued use of nicotine replacement products in those who have stopped smoking found no adverse effects from months to several years, and that people with cardiovascular disease were able to tolerate them for 12 weeks.[44] The general medical position is that nicotine itself, in small doses, poses few health risks, except among certain vulnerable groups.[20] A 2016 Royal College of Physicians report found "nicotine alone in the doses used by smokers represents little if any hazard to the user".[46] A 2014 American Heart Association policy statement found that some health concerns relate to nicotine.[44] Experimental research suggests that adolescent nicotine use may harm brain development.[21] Children exposed to nicotine may have a number of lifelong health issues.[14] Administration of nicotine to guinea pigs has been shown to cause harm to cells of the inner ear.[47] As medicine, nicotine is used to help with quitting smoking and has good safety in this form.[22]
Metabolism and body weight
By reducing the appetite and raising the metabolism, some smokers may lose weight as a consequence.[48][49] By increasing metabolic rate and inhibiting the usual compensatory increase in appetite, the body weight of smokers is lower on average than that of non-smokers. When smokers quit, they gain on average 5–6 kg weight, returning to the average weight of non-smokers.[50]
Vascular system
A 2014 review found that nicotine use is not a significant cause of cardiovascular disease.[51] A 2015 review found that nicotine is associated with cardiovascular disease.[23] A 2016 review suggests that "the risks of nicotine without tobacco combustion products (cigarette smoke) are low compared to cigarette smoking, but are still of concern in people with cardiovascular disease."[52] Some studies in people show the possibility that nicotine contributes to acute cardiovascular events in smokers with established cardiovascular disease, and induces pharmacologic effects that might contribute to increased atherosclerosis.[52] Prolonged nicotine use seems not to increase atherosclerosis.[52] Brief nicotine use, such as nicotine medicine, seems to incur a slight cardiovascular risk, even to people with established cardiovascular disease.[52] A 2015 review found "Nicotine in vitro and in animal models can inhibit apoptosis and enhance angiogenesis, effects that raise concerns about the role of nicotine in promoting the acceleration of atherosclerotic disease."[53] A 2012 Cochrane review found no evidence of an increased risk of cardiovascular disease with nicotine replacement products.[54] A 1996 randomized controlled trial using nicotine patches found that serious adverse events were not more frequent among smokers with cardiovascular disease.[54] A meta-analysis shows that snus consumption, which delivers nicotine at a dose equivalent to that of cigarettes, is not associated with heart attacks.[55] Hence, it is not nicotine, but tobacco smoke's other components which seem to be implicated in ischemic heart disease.[55] Nicotine increases heart rate and blood pressure[56] and induces abnormal heart rhythms.[57] Nicotine can also induce potentially atherogenic genes in human coronary artery endothelial cells.[58] Microvascular injury can result through its action on nicotinic acetylcholine receptors (nAChRs).[59] Nicotine does not adversely affect serum cholesterol levels,[51] but a 2015 review found it may elevate serum cholesterol levels.[23] Many quitting smoking studies using nicotine medicines report lowered dyslipidemia with considerable benefit in HDL/LDL ratios.[52] Nicotine supports clot formation and aids in plaque formation by enhancing vascular smooth muscle.[23]
Cancer
Although there is insufficient evidence to classify nicotine as a carcinogen, there is an ongoing debate about whether it functions as a tumor promoter.[61] In vitro studies have associated it with cancer, but carcinogenicity has not been demonstrated in vivo.[23] There is inadequate research to demonstrate that nicotine is associated with cancer in humans, but there is evidence indicating possible oral, esophageal, or pancreatic cancer risks.[21] Nicotine in the form of nicotine replacement products is less of a cancer risk than smoking.[21] Nicotine replacement products have not been shown to be associated with cancer in the real world.[23]
While no epidemiological evidence directly supports the notion that nicotine acts as a carcinogen in the formation of human cancer, research has identified nicotine's indirect involvement in cancer formation in animal models and cell cultures.[62][63][64] Nicotine increases cholinergic signalling and adrenergic signalling in the case of colon cancer,[65] thereby impeding apoptosis (programmed cell death), promoting tumor growth, and activating growth factors and cellular mitogenic factors such as 5-lipoxygenase (5-LOX), and epidermal growth factor (EGF). Nicotine also promotes cancer growth by stimulating angiogenesis and neovascularization.[66][67] In one study, nicotine administered to mice with tumors caused increases in tumor size (twofold increase), metastasis (nine-fold increase), and tumor recurrence (threefold increase).[68] N-Nitrosonornicotine (NNN), classified by the International Agency for Research on Cancer (IARC) as a Group 1 carcinogen, has been shown to form in vitro from nornicotine in human saliva, indicating nornicotine is a carcinogen precursor.[69] The IARC has not evaluated pure nicotine or assigned it to an official carcinogenic classification.
In cancer cells, nicotine promotes the epithelial–mesenchymal transition which makes the cancer cells more resistant to drugs that treat cancer.[70]
Fetal development
In pregnancy, a 2013 review noted that "nicotine is only 1 of more than 4000 compounds to which the fetus is exposed through maternal smoking. Of these, ∼30 compounds have been associated with adverse health outcomes. Although the exact mechanisms by which nicotine produces adverse fetal effects are unknown, it is likely that hypoxia, undernourishment of the fetus, and direct vasoconstrictor effects on the placental and umbilical vessels all play a role. Nicotine also has been shown to have significant deleterious effects on brain development, including alterations in brain metabolism and neurotransmitter systems and abnormal brain development." It also notes that "abnormalities of newborn neurobehavior, including impaired orientation and autonomic regulation and abnormalities of muscle tone, have been identified in a number of prenatal nicotine exposure studies" and that there is weak data associating fetal nicotine exposure with newborn facial clefts, and that there is no good evidence for newborns suffering nicotine withdrawal from fetal exposure to nicotine.[71]
Effective April 1, 1990, the Office of Environmental Health Hazard Assessment (OEHHA) of the California Environmental Protection Agency added nicotine to the list of chemicals known to cause developmental toxicity.[72]
Nicotine is not safe to use in any amount during pregnancy.[73] Questions exist regarding nicotine use during pregnancy and their potential consequences on fetal growth and mortality.[46] Nicotine negatively affects pregnancy outcomes and fetal brain development.[21] Risks to the child later in life via nicotine exposure during pregnancy include type 2 diabetes, obesity, hypertension, neurobehavioral defects, respiratory dysfunction, and infertility.[22] Nicotine crosses the placenta and is found in the breast milk of mothers who smoke as well as mothers who inhale passive smoke.[74]
Reinforcement disorders
Nicotine dependence involves aspects of both psychological dependence and physical dependence, since discontinuation of extended use has been shown to produce both affective (e.g., anxiety, irritability, craving, anhedonia) and somatic (mild motor dysfunctions such as tremor) withdrawal symptoms.[1] Withdrawal symptoms peak in the first day or two[75] and can persist for several weeks.[76] Nicotine has clinically significant cognitive-enhancing effects at low doses, particularly in fine motor skills, attention, and memory. These beneficial cognitive effects may play a role in the maintenance of tobacco dependence.[76]
Nicotine is highly addictive,[13][14][77] comparable to heroin or cocaine.[20] Nicotine activates the mesolimbic pathway and induces long-term ΔFosB expression in the nucleus accumbens when inhaled or injected at sufficiently high doses, but not necessarily when ingested.[78][79][80] Consequently, repeated daily exposure (possibly excluding oral route) to nicotine can result in accumbal ΔFosB overexpression, in turn causing nicotine addiction.[78][79]
In dependent smokers, smoking during withdrawal returns cognitive abilities to pre-withdrawal levels, but chronic use may not offer cognitive benefits over not smoking.[21][81]
Use of other drugs
In animals, it is relatively simple to determine if consumption of a certain drug increases the later attraction of another drug. In humans, where such direct experiments are not possible, longitudinal studies can show if the probability of a substance use is related to the earlier use of other substances.[82]
In mice nicotine increased the probability of later consumption of cocaine and the experiments permitted concrete conclusions on the underlying molecular biological alteration in the brain.[83] The biological changes in mice correspond to the epidemiological observations in humans that nicotine consumption is coupled to an increased probability of later use of cannabis and cocaine.[84]
In rats cannabis consumption – earlier in life – increased the later self-administration of nicotine.[85] A study of drug use of 14,577 US 12th graders showed that alcohol consumption was associated with an increased probability of later use of tobacco, cannabis, and illegal drugs.[86]
Overdose
Nicotine is regarded as a potentially lethal poison.[87] The LD50 of nicotine is 50 mg/kg for rats and 3 mg/kg for mice. 30–60 mg (0.5–1.0 mg/kg) can be a lethal dosage for adult humans.[15][88] However, the widely used human LD50 estimate of 0.5–1.0 mg/kg was questioned in a 2013 review, in light of several documented cases of humans surviving much higher doses; the 2013 review suggests that the lower limit causing fatal outcomes is 500–1000 mg of ingested nicotine, corresponding to 6.5–13 mg/kg orally.[17] Nevertheless, nicotine has a relatively high toxicity in comparison to many other alkaloids such as caffeine, which has an LD50 of 127 mg/kg when administered to mice.[89]
At high-enough doses, it is associated with nicotine poisoning.[21] Today nicotine is less commonly used in agricultural insecticides, which was a main source of poisoning. More recent cases of poisoning typically appear to be in the form of Green Tobacco Sickness or due to accidental ingestion of tobacco or tobacco products or ingestion of nicotine-containing plants.[90][91][92] People who harvest or cultivate tobacco may experience Green Tobacco Sickness (GTS), a type of nicotine poisoning caused by dermal exposure to wet tobacco leaves. This occurs most commonly in young, inexperienced tobacco harvesters who do not consume tobacco.[90][93] People can be exposed to nicotine in the workplace by breathing it in, skin absorption, swallowing it, or eye contact. The Occupational Safety and Health Administration (OSHA) has set the legal limit (permissible exposure limit) for nicotine exposure in the workplace as 0.5 mg/m3 skin exposure over an 8-hour workday. The US National Institute for Occupational Safety and Health (NIOSH) has set a recommended exposure limit (REL) of 0.5 mg/m3 skin exposure over an 8-hour workday. At environmental levels of 5 mg/m3, nicotine is immediately dangerous to life and health.[94]
It is unlikely that a person would overdose on nicotine through smoking alone. The US Food and Drug Administration (FDA) stated in 2013 that "There are no significant safety concerns associated with using more than one OTC NRT at the same time, or using an OTC NRT at the same time as another nicotine-containing product—including a cigarette."[95]
The rise in the use of electronic cigarettes, many forms of which are designed to be refilled with nicotine-containing e-liquid supplied in small plastic bottles, has raised concerns over nicotine overdoses, especially in the possibility of young children ingesting the liquids.[24] A 2015 Public Health England report noted an "unconfirmed newspaper report of a fatal poisoning of a two-year old child" and two published case reports of children of similar age who had recovered after ingesting e-liquid and vomiting.[24] They also noted case reports of suicides by nicotine.[24] Where adults drank liquid containing up to 1,500 mg of nicotine they recovered (helped by vomiting), but an ingestion apparently of about 10,000 mg was fatal, as was an injection.[24] They commented that "Serious nicotine poisoning seems normally prevented by the fact that relatively low doses of nicotine cause nausea and vomiting, which stops users from further intake."[24]
Pharmacology
Pharmacodynamics
Nicotine acts as a receptor agonist at most nicotinic acetylcholine receptors (nAChRs),[4][5] except at two nicotinic receptor subunits (nAChRα9 and nAChRα10) where it acts as a receptor antagonist.[4]
Central nervous system
By binding to nicotinic acetylcholine receptors in the brain, nicotine elicits its psychoactive effects and increases the levels of several neurotransmitters in various brain structures – acting as a sort of "volume control." Nicotine has a higher affinity for nicotinic receptors in the brain than those in skeletal muscle, though at toxic doses it can induce contractions and respiratory paralysis.[96] Nicotine's selectivity is thought to be due to a particular amino acid difference on these receptor subtypes.[97]
Nicotine activates nicotinic receptors (particularly α4β2 nicotinic receptors) on neurons that innervate the ventral tegmental area and within the mesolimbic pathway where it appears to cause the release of dopamine.[98][99] This nicotine-induced dopamine release occurs at least partially through activation of the cholinergic–dopaminergic reward link in the ventral tegmental area.[99] Nicotine also appears to induce the release of endogenous opioids that activate opioid pathways in the reward system, since naltrexone – an opioid receptor antagonist – blocks nicotine self-administration.[98] These actions are largely responsible for the strongly reinforcing effects of nicotine, which often occur in the absence of euphoria;[98] however, mild euphoria from nicotine use can occur in some individuals.[98] Chronic nicotine use inhibits class I and II histone deacetylases in the striatum, where this effect plays a role in nicotine addiction.[100][101]
Sympathetic nervous system
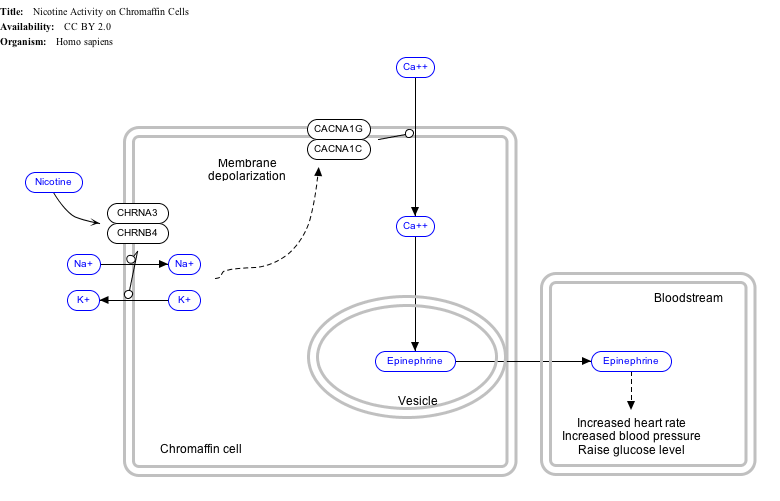
Nicotine also activates the sympathetic nervous system,[102] acting via splanchnic nerves to the adrenal medulla, stimulating the release of epinephrine. Acetylcholine released by preganglionic sympathetic fibers of these nerves acts on nicotinic acetylcholine receptors, causing the release of epinephrine (and norepinephrine) into the bloodstream.
Adrenal medulla
By binding to ganglion type nicotinic receptors in the adrenal medulla, nicotine increases flow of adrenaline (epinephrine), a stimulating hormone and neurotransmitter. By binding to the receptors, it causes cell depolarization and an influx of calcium through voltage-gated calcium channels. Calcium triggers the exocytosis of chromaffin granules and thus the release of epinephrine (and norepinephrine) into the bloodstream. The release of epinephrine (adrenaline) causes an increase in heart rate, blood pressure and respiration, as well as higher blood glucose levels.[103]
Pharmacokinetics
As nicotine enters the body, it is distributed quickly through the bloodstream and crosses the blood–brain barrier reaching the brain within 10–20 seconds after inhalation.[105] The elimination half-life of nicotine in the body is around two hours.[106]
The amount of nicotine absorbed by the body from smoking can depend on many factors, including the types of tobacco, whether the smoke is inhaled, and whether a filter is used. However, it has been found that the nicotine yield of individual products has only a small effect (4.4%) on the blood concentration of nicotine,[107] suggesting "the assumed health advantage of switching to lower-tar and lower-nicotine cigarettes may be largely offset by the tendency of smokers to compensate by increasing inhalation".
Nicotine has a half-life of 1–2 hours. Cotinine is an active metabolite of nicotine that remains in the blood with a half-life of 18–20 hours, making it easier to analyze.[108]
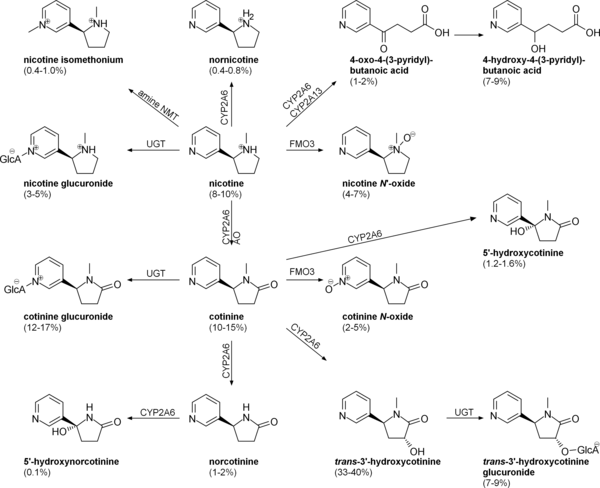
Nicotine is metabolized in the liver by cytochrome P450 enzymes (mostly CYP2A6, and also by CYP2B6) and FMO3, which selectively metabolizes (S)-nicotine. A major metabolite is cotinine. Other primary metabolites include nicotine N'-oxide, nornicotine, nicotine isomethonium ion, 2-hydroxynicotine and nicotine glucuronide.[109] Under some conditions, other substances may be formed such as myosmine.[110]
Glucuronidation and oxidative metabolism of nicotine to cotinine are both inhibited by menthol, an additive to mentholated cigarettes, thus increasing the half-life of nicotine in vivo.[111]
Chemistry
| NFPA 704 fire diamond | |
|---|---|
|
The fire diamond hazard sign for nicotine.[112] |
Nicotine is a hygroscopic, colorless to yellow-brown, oily liquid, that is readily soluble in alcohol, ether or light petroleum. It is miscible with water in its base form between 60 °C and 210 °C. As a nitrogenous base, nicotine forms salts with acids that are usually solid and water-soluble. Its flash point is 95 °C and its auto-ignition temperature is 244 °C.[113]
Nicotine is readily volatile (vapor pressure 5.5 ㎩ at 25 ℃) and dibasic (Kb1 = 1×10⁻⁶, Kb2 = 1×10⁻¹¹).[6]
Nicotine is optically active, having two enantiomeric forms. The naturally occurring form of nicotine is levorotatory with a specific rotation of [α]D = –166.4° ((−)-nicotine). The dextrorotatory form, (+)-nicotine is physiologically less active than (−)-nicotine. (−)-nicotine is more toxic than (+)-nicotine.[114] The salts of (+)-nicotine are usually dextrorotatory. The hydrochloride and sulphate salts become optically inactive if heated in a closed vessel above 180 °C.[115]
On exposure to ultraviolet light or various oxidizing agents, nicotine is converted to nicotine oxide, nicotinic acid (vitamin B3), and methylamine.[115]
Occurrence and biosynthesis

Nicotine is a natural product of tobacco, occurring in the leaves in a range of 0.5 to 7.5% depending on variety.[116] Nicotine also naturally occurs in smaller amounts in plants from the family Solanaceae (such as potatoes, tomatoes, and eggplant, and peppers[8]).[9]
The biosynthetic pathway of nicotine involves a coupling reaction between the two cyclic structures that compose nicotine. Metabolic studies show that the pyridine ring of nicotine is derived from niacin (nicotinic acid) while the pyrrolidone is derived from N-methyl-Δ1-pyrrollidium cation.[117][118] Biosynthesis of the two component structures proceeds via two independent syntheses, the NAD pathway for niacin and the tropane pathway for N-methyl-Δ1-pyrrollidium cation.
The NAD pathway in the genus Nicotiana begins with the oxidation of aspartic acid into α-imino succinate by aspartate oxidase (AO). This is followed by a condensation with glyceraldehyde-3-phosphate and a cyclization catalyzed by quinolinate synthase (QS) to give quinolinic acid. Quinolinic acid then reacts with phosphoriboxyl pyrophosphate catalyzed by quinolinic acid phosphoribosyl transferase (QPT) to form niacin mononucleotide (NaMN). The reaction now proceeds via the NAD salvage cycle to produce niacin via the conversion of nicotinamide by the enzyme nicotinamidase.
The N-methyl-Δ1-pyrrollidium cation used in the synthesis of nicotine is an intermediate in the synthesis of tropane-derived alkaloids. Biosynthesis begins with decarboxylation of ornithine by ornithine decarboxylase (ODC) to produce putrescine. Putrescine is then converted into N-methyl putrescine via methylation by SAM catalyzed by putrescine N-methyltransferase (PMT). N-methylputrescine then undergoes deamination into 4-methylaminobutanal by the N-methylputrescine oxidase (MPO) enzyme, 4-methylaminobutanal then spontaneously cyclize into N-methyl-Δ1-pyrrollidium cation.
The final step in the synthesis of nicotine is the coupling between N-methyl-Δ1-pyrrollidium cation and niacin. Although studies conclude some form of coupling between the two component structures, the definite process and mechanism remains undetermined. The current agreed theory involves the conversion of niacin into 2,5-dihydropyridine through 3,6-dihydronicotinic acid. The 2,5-dihydropyridine intermediate would then react with N-methyl-Δ1-pyrrollidium cation to form enantiomerically pure (−)-nicotine.[119]
Detection in body fluids
Nicotine can be quantified in blood, plasma, or urine to confirm a diagnosis of poisoning or to facilitate a forensic autopsy. Urinary or salivary cotinine concentrations are frequently measured for the purposes of pre-employment and health insurance medical screening programs. Careful interpretation of results is important, since passive exposure to cigarette smoke can result in significant accumulation of nicotine, followed by the appearance of its metabolites in various body fluids.[120][121] Nicotine use is not regulated in competitive sports programs.[122]
History
Nicotine is named after the tobacco plant Nicotiana tabacum, which in turn is named after the French ambassador in Portugal, Jean Nicot de Villemain, who sent tobacco and seeds to Paris in 1560, presented to the French King,[123] and who promoted their medicinal use. Smoking was believed to protect against illness, particularly the plague.[123]
Tobacco was introduced to Europe in 1559, and by the late 17th century, it was used not only for smoking but also as an insecticide. After World War II, over 2,500 tons of nicotine insecticide were used worldwide, but by the 1980s the use of nicotine insecticide had declined below 200 tons. This was due to the availability of other insecticides that are cheaper and less harmful to mammals.[12]
Currently, nicotine, even in the form of tobacco dust, is prohibited as a pesticide for organic farming in the United States.[124][125]
In 2008, the EPA received a request, from the registrant, to cancel the registration of the last nicotine pesticide registered in the United States.[126] This request was granted, and since 1 January 2014, this pesticide has not been available for sale.[127]
Chemical identification
Nicotine was first isolated from the tobacco plant in 1828 by physician Christian Wilhelm Posselt and chemist Karl Ludwig Reimann of Germany, who considered it a poison.[128][129][130] Its chemical empirical formula was described by Melsens in 1843,[131] its structure was discovered by Adolf Pinner and Richard Wolffenstein in 1893,[132][133][134] and it was first synthesized by Amé Pictet and A. Rotschy in 1904.[135]
Society and culture
The nicotine content of popular American-brand cigarettes has increased over time, and one study found that there was an average increase of 1.78% per year between the years of 1998 and 2005.[136]
Research
While acute/initial nicotine intake causes activation of nicotine receptors, chronic low doses of nicotine use leads to desensitisation of nicotine receptors (due to the development of tolerance) and results in an antidepressant effect, with early research showing low dose nicotine patches could be an effective treatment of major depressive disorder in non-smokers.[137] However, the original research concluded that: "Nicotine patches produced short-term improvement of depression with minor side effects. Because of nicotine's high risk to health, nicotine patches are not recommended for clinical use in depression."[138]
Though tobacco smoking is associated with an increased risk of Alzheimer's disease,[139] there is evidence that nicotine itself has the potential to prevent and treat Alzheimer's disease.[140]
Research into nicotine's most predominant metabolite, cotinine, suggests that some of nicotine's psychoactive effects are mediated by cotinine.[141][142]
Little research is available in humans but animal research suggests there is potential benefit from nicotine in Parkinson's disease.[143] In humans, there is epidemiologic evidence for a reduced risk of Parkinson's associated with tobacco use,[143] consumption of Solanaceae vegetables in general,[144] and consumption of peppers in particular.[144]
See also
References
- 1 2 3 D'Souza MS, Markou A (2011). "Neuronal mechanisms underlying development of nicotine dependence: implications for novel smoking-cessation treatments". Addict Sci Clin Pract. 6 (1): 4–16. PMC 3188825. PMID 22003417.
Withdrawal symptoms upon cessation of nicotine intake: Chronic nicotine use induces neuroadaptations in the brain’s reward system that result in the development of nicotine dependence. Thus, nicotine-dependent smokers must continue nicotine intake to avoid distressing somatic and affective withdrawal symptoms. Newly abstinent smokers experience symptoms such as depressed mood, anxiety, irritability, difficulty concentrating, craving, bradycardia, insomnia, gastrointestinal discomfort, and weight gain (Shiffman and Jarvik, 1976; Hughes et al., 1991). Experimental animals, such as rats and mice, exhibit a nicotine withdrawal syndrome that, like the human syndrome, includes both somatic signs and a negative affective state (Watkins et al., 2000; Malin et al., 2006). The somatic signs of nicotine withdrawal include rearing, jumping, shakes, abdominal constrictions, chewing, scratching, and facial tremors. The negative affective state of nicotine withdrawal is characterized by decreased responsiveness to previously rewarding stimuli, a state called anhedonia.
- 1 2 Cosci, F; Pistelli, F; Lazzarini, N; Carrozzi, L (2011). "Nicotine dependence and psychological distress: outcomes and clinical implications in smoking cessation". Psychology Research and Behavior Management. 4: 119–28. doi:10.2147/prbm.s14243. PMC 3218785. PMID 22114542.
- ↑ Mannfred A. Hollinger (19 October 2007). Introduction to Pharmacology, Third Edition. Abingdon: CRC Press. pp. 222–223. ISBN 978-1-4200-4742-4.
- 1 2 3 4 "Nicotinic acetylcholine receptors: Introduction". IUPHAR Database. International Union of Basic and Clinical Pharmacology. Retrieved 1 September 2014.
- 1 2 Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 9: Autonomic Nervous System". In Sydor A, Brown RY. Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. p. 234. ISBN 9780071481274.
Nicotine ... is a natural alkaloid of the tobacco plant. Lobeline is a natural alkaloid of Indian tobacco. Both drugs are agonists are nicotinic cholinergic receptors ...
- 1 2 Robert L. Metcalf (2007), "Insect Control", Ullmann's Encyclopedia of Industrial Chemistry (7th ed.), Wiley, p. 9
- ↑ "Smoking and Tobacco Control Monograph No. 9" (PDF). Retrieved 2012-12-19.
- 1 2 Siegmund, Barbara; Leitner, Erich; Pfannhauser, Werner (1999-07-23). "Determination of the Nicotine Content of Various Edible Nightshades (Solanaceae) and Their Products and Estimation of the Associated Dietary Nicotine Intake". J. Agric. Food Chem. 47 (8): 3113–3120. doi:10.1021/jf990089w. Retrieved 2017-04-25.
- 1 2 Domino, Edward F.; Hornbach, Erich; Demana, Tsenge (August 1993). "The Nicotine Content of Common Vegetables". The New England Journal of Medicine. 329 (6): 437. doi:10.1056/NEJM199308053290619. PMID 8326992.
- ↑ Moldoveanu, Serban C.; Scott, Wayne A.; Lawson, Darlene M. (2016-04-01). "Nicotine Analysis in Several Non-Tobacco Plant Materials". Beiträge zur Tabakforschung International/Contributions to Tobacco Research. 27 (2): 54–59. doi:10.1515/cttr-2016-0008. ISSN 1612-9237. Retrieved 2017-05-05.
- ↑ Rodgman, Alan; Perfetti, Thomas A. (2009). The chemical components of tobacco and tobacco smoke. Boca Raton, FL: CRC Press. ISBN 978-1-4200-7883-1. LCCN 2008018913.
- 1 2 Ujváry, István (1999). "Nicotine and Other Insecticidal Alkaloids". In Yamamoto, Izuru; Casida, John. Nicotinoid Insecticides and the Nicotinic Acetylcholine Receptor. Tokyo: Springer-Verlag. pp. 29–69.
- 1 2 Grana, R; Benowitz, N; Glantz, SA (13 May 2014). "E-cigarettes: a scientific review". Circulation. 129 (19): 1972–86. doi:10.1161/circulationaha.114.007667. PMC 4018182. PMID 24821826.
- 1 2 3 Holbrook, Bradley D. (2016). "The effects of nicotine on human fetal development". Birth Defects Research Part C: Embryo Today: Reviews. 108 (2): 181–92. doi:10.1002/bdrc.21128. ISSN 1542-975X. PMID 27297020.
- 1 2 "Nicotine (PIM)". Inchem.org. Retrieved 2012-12-19.
- ↑ Genetic Science Learning Center. "How Drugs Can Kill".
- 1 2 3 Mayer B (January 2014). "How much nicotine kills a human? Tracing back the generally accepted lethal dose to dubious self-experiments in the nineteenth century". Archives of Toxicology. 88 (1): 5–7. doi:10.1007/s00204-013-1127-0. PMC 3880486. PMID 24091634.
- ↑ Caponnetto, Pasquale; Campagna, Davide; Papale, Gabriella; Russo, Cristina; Polosa, Riccardo (2012). "The emerging phenomenon of electronic cigarettes". Expert Review of Respiratory Medicine. 6 (1): 63–74. doi:10.1586/ers.11.92. ISSN 1747-6348. PMID 22283580.
- ↑ Dinakar C, O'Connor GT (2016). "The Health Effects of Electronic Cigarettes". NEJM. 375 (14): 1372–1381. doi:10.1056/NEJMra1502466. PMID 27705269.
- 1 2 3 de Andrade, Marisa; Hastings, Gerald. "Tobacco Harm Reduction and Nicotine Containing Products" (PDF). Cancer Research UK. Cancer Research UK. p. 8. Retrieved 10 March 2016.
- 1 2 3 4 5 6 7 8 9 National Center for Chronic Disease Prevention Health Promotion (US) Office on Smoking Health (2014). "The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General, Chapter 5 - Nicotine" (PDF). Surgeon General of the United States: 107–138. PMID 24455788.
- 1 2 3 4 Schraufnagel, Dean E.; Blasi, Francesco; Drummond, M. Bradley; Lam, David C. L.; Latif, Ehsan; Rosen, Mark J.; Sansores, Raul; Van Zyl-Smit, Richard (2014). "Electronic Cigarettes. A Position Statement of the Forum of International Respiratory Societies". American Journal of Respiratory and Critical Care Medicine. 190 (6): 611–618. doi:10.1164/rccm.201407-1198PP. ISSN 1073-449X. PMID 25006874.
- 1 2 3 4 5 6 7 Jerry JM, Collins GB, Streem D (2015). "E-cigarettes: Safe to recommend to patients?". Cleve Clin J Med. 82 (8): 521–6. doi:10.3949/ccjm.82a.14054. PMID 26270431.
Nicotine plays a direct role in carcinogenesis through a variety of mechanisms, including increasing the activity of tumor growth-promoting transcription factors, decreasing apoptosis, and increasing angiogenesis in tumors. Additionally, specific types of nicotinic acetylcholine receptors— eg, alpha 7 receptors, which are stimulated by nicotine—are found in many malignant tumors and are thought to play a role in tumor progression.12 Blockade of alpha 7 nicotinic acetylcholine receptors has been shown to decrease the growth of certain cancers. However, these findings were from in vitro studies, and the concerns they raised have not been reflected in in vivo studies. Despite having been on the market for 30 years, nicotine replacement therapy has as yet not been associated with any “real world” increase in cancer risk.
- 1 2 3 4 5 6 McNeill, A, SC (2015). "E - cigarettes: an evidence update A report commissioned by Public Health England" (PDF). www.gov.uk. UK: Public Health England. p. 63–64. Retrieved 20 August 2015.
- ↑ "Effective Clinical Tobacco Intervention". Therapeutics Letter (21): 1–4. September–October 1997.
- ↑ Lagrue, Gilbert; Cormier, Anne (June 2001). "Des récepteurs nicotiniques à la dépendance tabagique: Perspectives thérapeutiques" [From nicotinic receptors to smoking dependence: Therapeutic prospects]. Alcoologie et Addictologie (in French). 23 (2): 39S–42S. ISSN 1620-4522. INIST:1081618.
- 1 2 Pomerleau, Ovide F.; Pomerleau, Cynthia S. (1984). "Neuroregulators and the reinforcement of smoking: Towards a biobehavioral explanation". Neuroscience & Biobehavioral Reviews. 8 (4): 503–513. doi:10.1016/0149-7634(84)90007-1. PMID 6151160.
- ↑ Pomerleau, Ovide F.; Rosecrans, John (1989). "Neuroregulatory effects of nicotine". Psychoneuroendocrinology. 14 (6): 407–423. doi:10.1016/0306-4530(89)90040-1.
- ↑ Easton, John (March 28, 2002). "Nicotine extends duration of pleasant effects of dopamine". The University of Chicago Chronicle. 21 (12).
- ↑ Kenny PJ, Markou A (Jun 2006). "Nicotine self-administration acutely activates brain reward systems and induces a long-lasting increase in reward sensitivity". Neuropsychopharmacology. 31 (6): 1203–11. doi:10.1038/sj.npp.1300905. PMID 16192981.
- ↑ "Erowid Nicotine Vault: Dosage". Erowid.org. 2011-10-14. Retrieved 2012-12-19.
- ↑ Golding, J. F.; Mangan, G. L. (1989). "Factors Governing Recruitment to and Maintenance of Smoking". In Einstein, Stanley. Drug and Alcohol Use. pp. 101–17. doi:10.1007/978-1-4899-0888-9_9. ISBN 978-1-4899-0890-2.
- ↑ Nesbitt P (1969). Smoking, physiological arousal, and emotional response. Unpublished doctoral dissertation, Columbia University.
- ↑ Parrott AC (January 1998). "Nesbitt's Paradox resolved? Stress and arousal modulation during cigarette smoking" (PDF). Addiction. 93 (1): 27–39. CiteSeerX 10.1.1.465.2496. doi:10.1046/j.1360-0443.1998.931274.x. PMID 9624709.
- ↑ Wadgave, U; Nagesh, L (2016). "Nicotine Replacement Therapy: An Overview". International Journal of Health Sciences. 10 (3): 425–435. PMC 5003586. PMID 27610066.
- 1 2 Stead LF, Perera R, Bullen C, Mant D, Lancaster T (2008). Stead, Lindsay F, ed. "Nicotine replacement therapy for smoking cessation". Cochrane Database Syst Rev (1): CD000146. doi:10.1002/14651858.CD000146.pub3. PMID 18253970.
- ↑ Pierce, John P.; Cummins, Sharon E.; White, Martha M.; Humphrey, Aimee; Messer, Karen (2012). "Quitlines and Nicotine Replacement for Smoking Cessation: Do We Need to Change Policy?". Annual Review of Public Health. 33: 341–56. doi:10.1146/annurev-publhealth-031811-124624. PMID 22224888.
- ↑ Jasinska, Agnes J.; Zorick, Todd; Brody, Arthur L.; Stein, Elliot A. (September 2014). "Dual role of nicotine in addiction and cognition: A review of neuroimaging studies in humans". Neuropharmacology. 84: 111–122. doi:10.1016/j.neuropharm.2013.02.015. PMC 3710300. PMID 23474015.
- ↑ Heishman SJ, Kleykamp BA, Singleton EG (June 2010). "Meta-analysis of the acute effects of nicotine and smoking on human performance". Psychopharmacology. 210 (4): 453–69. doi:10.1007/s00213-010-1848-1. PMC 3151730. PMID 20414766.
- ↑ Sarter M (August 2015). "Behavioral-cognitive targets for cholinergic enhancement". Current Opinion in Behavioral Sciences. 4: 22–26. doi:10.1016/j.cobeha.2015.01.004. PMC 5466806. PMID 28607947.
- ↑ "Nicotine: Biological activity". IUPHAR/BPS Guide to Pharmacology. International Union of Basic and Clinical Pharmacology. Retrieved 7 February 2016.
Kis as follows; α2β4=9900nM [5], α3β2=14nM [1], α3β4=187nM [1], α4β2=1nM [4,6]. Due to the heterogeneity of nACh channels we have not tagged a primary drug target for nicotine, although the α4β2 is reported to be the predominant high affinity subtype in the brain which mediates nicotine addiction [2-3].
- ↑ Majdi, A; Kamari, F; Vafaee, M.S.; Sadigh-Eteghad, S (June 2017). "Revisiting nicotine's role in the ageing brain and cognitive impairment". Reviews in the Neurosciences. 28 (7): 767–781. doi:10.1515/revneuro-2017-0008. PMID 28586306.
- ↑ "DrugFacts: Cigarettes and Other Tobacco Products". National Institute on Drug Abuse. December 2014. Retrieved 28 April 2015.
- 1 2 3 4 Bhatnagar, A.; Whitsel, L. P.; Ribisl, K. M.; Bullen, C.; Chaloupka, F.; Piano, M. R.; Robertson, R. M.; McAuley, T.; Goff, D.; Benowitz, N. (2014). "Electronic Cigarettes: A Policy Statement From the American Heart Association". Circulation. 130 (16): 1418–1436. doi:10.1161/CIR.0000000000000107. ISSN 0009-7322. PMID 25156991.
- ↑ Rodu, Brad (2011). "The scientific foundation for tobacco harm reduction, 2006-2011". Harm Reduction Journal. 8 (1): 19. doi:10.1186/1477-7517-8-19. PMC 3161854. PMID 21801389.
- 1 2 Wilder, Natalie; Daley, Claire; Sugarman, Jane; Partridge, James (April 2016). "Nicotine without smoke: Tobacco harm reduction". UK: Royal College of Physicians. p. 125.
- ↑ Abdel-Hafez, AMM; Elgayar, SAM; Husain, OA; Thabet, HSA (2014). "Effect of nicotine on the structure of cochlea of guinea pigs". Anatomy & Cell Biology. 47.3 (2014 Sep): 162–170. doi:10.5115/acb.2014.47.3.162. PMC 4178191. PMID 25276475.
- ↑ Orsini, Jean-Claude (June 2001). "Dépendance tabagique et contrôle central de la glycémie et de l'appétit" [Dependence on tobacco smoking and brain systems controlling glycemia and appetite]. Alcoologie et Addictologie (in French). 23 (2 Suppl): 28S–36S. ISSN 1620-4522. INIST:1081638.
- ↑ Chen, Hui; Vlahos, Ross; Bozinovski, Steve; Jones, Jessica; Anderson, Gary P; Morris, Margaret J (2004). "Effect of Short-Term Cigarette Smoke Exposure on Body Weight, Appetite and Brain Neuropeptide Y in Mice". Neuropsychopharmacology. 30 (4): 713–9. doi:10.1038/sj.npp.1300597. PMID 15508020. Lay summary – The University of Melbourne (1 November 2004).
- ↑ Audrain-McGovern, J; Benowitz, NL (July 2011). "Cigarette smoking, nicotine, and body weight". Clinical Pharmacology and Therapeutics. 90 (1): 164–8. doi:10.1038/clpt.2011.105. PMC 3195407. PMID 21633341.
- 1 2 Farsalinos, K. E.; Polosa, R. (2014). "Safety evaluation and risk assessment of electronic cigarettes as tobacco cigarette substitutes: a systematic review". Therapeutic Advances in Drug Safety. 5 (2): 67–86. doi:10.1177/2042098614524430. ISSN 2042-0986. PMC 4110871. PMID 25083263.
- 1 2 3 4 5 Benowitz, Neal L.; Burbank, Andrea D. (2016). "Cardiovascular toxicity of nicotine: Implications for electronic cigarette use". Trends in Cardiovascular Medicine. 26 (6): 515–523. doi:10.1016/j.tcm.2016.03.001. ISSN 1050-1738. PMC 4958544. PMID 27079891.
- ↑ Morris, Pamela B.; Ference, Brian A.; Jahangir, Eiman; Feldman, Dmitriy N.; Ryan, John J.; Bahrami, Hossein; El-Chami, Mikhael F.; Bhakta, Shyam; Winchester, David E.; Al-Mallah, Mouaz H.; Sanchez Shields, Monica; Deedwania, Prakash; Mehta, Laxmi S.; Phan, Binh An P.; Benowitz, Neal L. (2015). "Cardiovascular Effects of Exposure to Cigarette Smoke and Electronic Cigarettes". Journal of the American College of Cardiology. 66 (12): 1378–1391. doi:10.1016/j.jacc.2015.07.037. ISSN 0735-1097. PMID 26383726.
- 1 2 Lindsay F. Stead, Rafael Perera, Chris Bullen, David Mant, Jamie Hartmann-Boyce, Kate Cahill & Tim Lancaster (November 2012). "Nicotine replacement therapy for smoking cessation". The Cochrane Database of Systematic Reviews. 11: CD000146. doi:10.1002/14651858.CD000146.pub4. PMID 23152200.
- 1 2 Hansson, Jenny; Galanti, Maria Rosaria; Hergens, Maria-Pia; Fredlund, Peeter; Ahlbom, Anders; Alfredsson, Lars; Bellocco, Rino; Eriksson, Marie; Hallqvist, Johan; Hedblad, Bo; Jansson, Jan-Håkan; Nilsson, Peter; Pedersen, Nancy; Trolle Lagerros, Ylva; Östergren, Per-Olof; Magnusson, Cecilia (2012). "Use of snus and acute myocardial infarction: pooled analysis of eight prospective observational studies". European Journal of Epidemiology. 27 (10): 771–779. doi:10.1007/s10654-012-9704-8. ISSN 0393-2990. PMID 22722951.
- ↑ "Nicotine". National Institute on Drug Abuse. June 2007.
- ↑ "WHO Right to Call for E-Cigarette Regulation". World Lung Federation. 26 August 2014.
- ↑ Zhang S, Day I, Ye S (February 2001). "Nicotine induced changes in gene expression by human coronary artery endothelial cells". Atherosclerosis. 154 (2): 277–83. doi:10.1016/S0021-9150(00)00475-5. PMID 11166759.
- ↑ Hawkins BT, Brown RC, Davis TP (February 2002). "Smoking and ischemic stroke: a role for nicotine?". Trends in Pharmacological Sciences. 23 (2): 78–82. doi:10.1016/S0165-6147(02)01893-X. PMID 11830264.
- ↑ Detailed reference list is located on a separate image page.
- ↑ Cardinale A, Nastrucci C, Cesario A, Russo P (January 2012). "Nicotine: specific role in angiogenesis, proliferation and apoptosis". Critical Reviews in Toxicology. 42 (1): 68–89. doi:10.3109/10408444.2011.623150. PMID 22050423.
- ↑ Hecht SS (July 1999). "Tobacco smoke carcinogens and lung cancer". J. Natl. Cancer Inst. 91 (14): 1194–210. doi:10.1093/jnci/91.14.1194. PMID 10413421.
- ↑ Wu WK, Cho CH (April 2004). "The pharmacological actions of nicotine on the gastrointestinal tract". J. Pharmacol. Sci. 94 (4): 348–58. doi:10.1254/jphs.94.348. PMID 15107574.
- ↑ Chowdhury P, Udupa KB (December 2006). "Nicotine as a mitogenic stimulus for pancreatic acinar cell proliferation". World J. Gastroenterol. 12 (46): 7428–32. PMC 4087586. PMID 17167829.
- ↑ Wong HP, Yu L, Lam EK, Tai EK, Wu WK, Cho CH (June 2007). "Nicotine promotes colon tumor growth and angiogenesis through beta-adrenergic activation". Toxicol. Sci. 97 (2): 279–87. doi:10.1093/toxsci/kfm060. PMID 17369603.
- ↑ Natori T, Sata M, Washida M, Hirata Y, Nagai R, Makuuchi M (October 2003). "Nicotine enhances neovascularization and promotes tumor growth". Mol. Cells. 16 (2): 143–6. PMID 14651253.
- ↑ Ye YN, Liu ES, Shin VY, Wu WK, Luo JC, Cho CH (January 2004). "Nicotine promoted colon cancer growth via epidermal growth factor receptor, c-Src, and 5-lipoxygenase-mediated signal pathway". J. Pharmacol. Exp. Ther. 308 (1): 66–72. doi:10.1124/jpet.103.058321. PMID 14569062.
- ↑ Davis R, Rizwani W, Banerjee S, et al. (2009). Pao W, ed. "Nicotine promotes tumor growth and metastasis in mouse models of lung cancer". PLoS ONE. 4 (10): e7524. Bibcode:2009PLoSO...4.7524D. doi:10.1371/journal.pone.0007524. PMC 2759510. PMID 19841737.
- ↑ Knezevich, A; Muzic, J; Hatsukami, D. K.; Hecht, S. S.; Stepanov, I (2013). "Nornicotine nitrosation in saliva and its relation to endogenous synthesis of N'-nitrosonornicotine in humans". Nicotine & Tobacco Research. 15 (2): 591–5. doi:10.1093/ntr/nts172. PMC 3611998. PMID 22923602.
- ↑ Kothari, AN; Mi, Z; Zapf, M; Kuo, PC (2014). "Novel clinical therapeutics targeting the epithelial to mesenchymal transition". Clinical and Translational Medicine. 3: 35. doi:10.1186/s40169-014-0035-0. PMC 4198571. PMID 25343018.
- ↑ Behnke M, Smith VC (March 2013). "Prenatal substance abuse: short- and long-term effects on the exposed fetus". Pediatrics. 131 (3): e1009–24. doi:10.1542/peds.2012-3931. PMID 23439891.
- ↑ http://oehha.ca.gov/prop65/prop65_list/files/P65single121809.pdf%5Bfull+citation+needed%5D
- ↑ Alawsi, F.; Nour, R.; Prabhu, S. (2015). "Are e-cigarettes a gateway to smoking or a pathway to quitting?". BDJ. 219 (3): 111–115. doi:10.1038/sj.bdj.2015.591. ISSN 0007-0610. PMID 26271862.
- ↑ "State Health Officer's Report on E-Cigarettes: A Community Health Threat" (PDF). California Tobacco Control Program. California Department of Public Health. January 2015. Archived from the original (PDF) on 29 January 2015.
- ↑ Hughes, John (2007). "Effects of abstinence from tobacco: Etiology, animal models, epidemiology, and significance: A subjective review". Nicotine & Tobacco Research. 9 (3): 329–339. doi:10.1080/14622200701188927. ISSN 1462-2203. PMID 17365765.
- 1 2 Heishman, SJ, Kleykamp, BA, Singleton, EG (July 2010). "Meta-analysis of the acute effects of nicotine and smoking on human performance". Pharmacology. 210 (4): 453–69. doi:10.1007/s00213-010-1848-1. PMC 3151730. PMID 20414766.
The significant effects of nicotine on motor abilities, attention, and memory likely represent true performance enhancement because they are not confounded by withdrawal relief. The beneficial cognitive effects of nicotine have implications for initiation of smoking and maintenance of tobacco dependence.
- ↑ Siqueira, Lorena M. (2016). "Nicotine and Tobacco as Substances of Abuse in Children and Adolescents". Pediatrics. 139 (1): e20163436. doi:10.1542/peds.2016-3436. ISSN 0031-4005. PMID 27994114.
- 1 2 Nestler EJ (December 2013). "Cellular basis of memory for addiction". Dialogues Clin Neurosci. 15 (4): 431–443. PMC 3898681. PMID 24459410.
- 1 2 Ruffle JK (November 2014). "Molecular neurobiology of addiction: what's all the (Δ)FosB about?". Am J Drug Alcohol Abuse. 40 (6): 428–437. doi:10.3109/00952990.2014.933840. PMID 25083822.
The knowledge of ΔFosB induction in chronic drug exposure provides a novel method for the evaluation of substance addiction profiles (i.e. how addictive they are). Xiong et al. used this premise to evaluate the potential addictive profile of propofol (119). Propofol is a general anaesthetic, however its abuse for recreational purpose has been documented (120). Using control drugs implicated in both ΔFosB induction and addiction (ethanol and nicotine), ...
Conclusions
ΔFosB is an essential transcription factor implicated in the molecular and behavioral pathways of addiction following repeated drug exposure. The formation of ΔFosB in multiple brain regions, and the molecular pathway leading to the formation of AP-1 complexes is well understood. The establishment of a functional purpose for ΔFosB has allowed further determination as to some of the key aspects of its molecular cascades, involving effectors such as GluR2 (87,88), Cdk5 (93) and NFkB (100). Moreover, many of these molecular changes identified are now directly linked to the structural, physiological and behavioral changes observed following chronic drug exposure (60,95,97,102). New frontiers of research investigating the molecular roles of ΔFosB have been opened by epigenetic studies, and recent advances have illustrated the role of ΔFosB acting on DNA and histones, truly as a ‘‘molecular switch’’ (34). As a consequence of our improved understanding of ΔFosB in addiction, it is possible to evaluate the addictive potential of current medications (119), as well as use it as a biomarker for assessing the efficacy of therapeutic interventions (121,122,124). - ↑ Marttila K, Raattamaa H, Ahtee L (July 2006). "Effects of chronic nicotine administration and its withdrawal on striatal FosB/DeltaFosB and c-Fos expression in rats and mice". Neuropharmacology. 51 (1): 44–51. doi:10.1016/j.neuropharm.2006.02.014. PMID 16631212.
- ↑ Bruijnzeel, Adrie W. (2012). "Tobacco addiction and the dysregulation of brain stress systems". Neuroscience & Biobehavioral Reviews. 36 (5): 1418–1441. doi:10.1016/j.neubiorev.2012.02.015. ISSN 0149-7634. PMC 3340450. PMID 22405889.
- ↑ D. B. Kandel (Ed.): Stages and Pathways of Drug Involvement: Examining the Gateway Hypothesis, Cambridge University Press, 2002, ISBN 978-0-521-78969-1, pp. 3-10.
- ↑ E. R. Kandel; D. B. Kandel (2014). "A Molecular Basis for Nicotine as a Gateway Drug". New England Journal of Medicine. 371 (10): 932–943. doi:10.1056/NEJMsa1405092. PMC 4353486. PMID 25184865.
- ↑ Keyes, K. M.; Hamilton, A; Kandel, D. B. (2016). "Birth Cohorts Analysis of Adolescent Cigarette Smoking and Subsequent Marijuana and Cocaine Use". American Journal of Public Health. 106 (6): 1143–9. doi:10.2105/AJPH.2016.303128. PMC 4880234. PMID 27077359.
- ↑ Panlilio, L. V.; Zanettini, C; Barnes, C; Solinas, M; Goldberg, S. R. (2013). "Prior Exposure to THC Increases the Addictive Effects of Nicotine in Rats". Neuropsychopharmacology. 38 (7): 1198–1208. doi:10.1038/npp.2013.16. PMC 3656362. PMID 23314220.
- ↑ Kirby, T; Barry, A. E. (2012). "Alcohol as a gateway drug: A study of US 12th graders" (PDF). Journal of School Health. 82 (8): 371–9. doi:10.1111/j.1746-1561.2012.00712.x. PMID 22712674.
- ↑ Brandon, T. H.; Goniewicz, M. L.; Hanna, N. H.; Hatsukami, D. K.; Herbst, R. S.; Hobin, J. A.; Ostroff, J. S.; Shields, P. G.; Toll, B. A.; Tyne, C. A.; Viswanath, K.; Warren, G. W. (2015). "Electronic Nicotine Delivery Systems: A Policy Statement from the American Association for Cancer Research and the American Society of Clinical Oncology". Clinical Cancer Research. 21 (3): 514–525. doi:10.1158/1078-0432.CCR-14-2544. ISSN 1078-0432. PMID 25573384.
- ↑ Okamoto M, Kita T, Okuda H, Tanaka T, Nakashima T (Jul 1994). "Effects of aging on acute toxicity of nicotine in rats". Pharmacol Toxicol. 75 (1): 1–6. doi:10.1111/j.1600-0773.1994.tb00316.x. PMID 7971729.
- ↑ Toxicology and Applied Pharmacology. Vol. 44, Pg. 1, 1978.
- 1 2 Schep LJ, Slaughter RJ, Beasley DM (September–October 2009). "Nicotinic plant poisoning". Clinical Toxicology. 47 (8): 771–81. doi:10.1080/15563650903252186. PMID 19778187.
- ↑ Smolinske SC, Spoerke DG, Spiller SK, Wruk KM, Kulig K, Rumack BH (January 1988). "Cigarette and nicotine chewing gum toxicity in children". Human Toxicology. 7 (1): 27–31. doi:10.1177/096032718800700105. PMID 3346035.
- ↑ Furer V, Hersch M, Silvetzki N, Breuer GS, Zevin S (March 2011). "Nicotiana glauca (tree tobacco) intoxication--two cases in one family". Journal of Medical Toxicology. 7 (1): 47–51. doi:10.1007/s13181-010-0102-x. PMC 3614112. PMID 20652661.
- ↑ Gehlbach SH, Williams WA, Perry LD, Woodall JS (September 1974). "Green-tobacco sickness. An illness of tobacco harvesters". JAMA. 229 (14): 1880–3. doi:10.1001/jama.1974.03230520022024. PMID 4479133.
- ↑ "CDC - NIOSH Pocket Guide to Chemical Hazards - Nicotine". www.cdc.gov. Retrieved 2015-11-20.
- ↑ "Consumer Updates: Nicotine Replacement Therapy Labels May Change". FDA. April 1, 2013.
- ↑ Katzung, Bertram G. (2006). Basic and Clinical Pharmacology. New York: McGraw-Hill Medical. pp. 99–105.
- ↑ Xiu X, Puskar NL, Shanata JA, Lester HA, Dougherty DA (March 2009). "Nicotine binding to brain receptors requires a strong cation-pi interaction". Nature. 458 (7237): 534–7. Bibcode:2009Natur.458..534X. doi:10.1038/nature07768. PMC 2755585. PMID 19252481.
- 1 2 3 4 Malenka RC, Nestler EJ, Hyman SE (2009). Sydor A, Brown RY, eds. Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 369, 372–373. ISBN 9780071481274.
- 1 2 Dickson, Suzanne L.; Egecioglu, Emil; Landgren, Sara; Skibicka, Karolina P.; Engel, Jörgen A.; Jerlhag, Elisabet (2011). "The role of the central ghrelin system in reward from food and chemical drugs". Molecular and Cellular Endocrinology. 340 (1): 80–7. doi:10.1016/j.mce.2011.02.017. hdl:2077/26318. PMID 21354264.
This reward link comprises a dopamine projection from the ventral tegmental area (VTA) to the nucleus accumbens together with a cholinergic input, arising primarily from the laterodorsal tegmental area.
- ↑ Amir Levine; et al. (2011). "Molecular Mechanism for a Gateway Drug: Epigenetic Changes Initiated by Nicotine Prime Gene Expression by Cocaine". Sci Transl Med. 3 (107): 107ra109. doi:10.1126/scitranslmed.3003062. PMC 4042673. PMID 22049069.
- ↑ Volkow ND (November 2011). "Epigenetics of nicotine: another nail in the coughing". Sci Transl Med. 3 (107): 107ps43. doi:10.1126/scitranslmed.3003278. PMC 3492949. PMID 22049068.
- ↑ Yoshida T, Sakane N, Umekawa T, Kondo M (Jan 1994). "Effect of nicotine on sympathetic nervous system activity of mice subjected to immobilization stress". Physiol. Behav. 55 (1): 53–7. doi:10.1016/0031-9384(94)90009-4. PMID 8140174.
- ↑ Elaine N. Marieb; Katja Hoehn (2007). Human Anatomy & Physiology (7th Ed.). Pearson. pp. ?. ISBN 978-0-8053-5909-1.
- ↑ Henningfield, Jack E.; Calvento, Emma; Pogun, Sakire (2009). Nicotine Psychopharmacology. Springer. pp. 35, 37. ISBN 978-3-540-69248-5.
- ↑ Le Houezec J (September 2003). "Role of nicotine pharmacokinetics in nicotine addiction and nicotine replacement therapy: a review". The International Journal of Tuberculosis and Lung Disease. 7 (9): 811–9. PMID 12971663.
- ↑ Benowitz NL, Jacob P, Jones RT, Rosenberg J (May 1982). "Interindividual variability in the metabolism and cardiovascular effects of nicotine in man". The Journal of Pharmacology and Experimental Therapeutics. 221 (2): 368–72. PMID 7077531.
- ↑ Russell MA, Jarvis M, Iyer R, Feyerabend C. Relation of nicotine yield of cigarettes to blood nicotine concentrations in smokers. Br Med J. 1980 April 5; 280(6219): 972–976.
- ↑ Bhalala, Oneil (Spring 2003). "Detection of Cotinine in Blood Plasma by HPLC MS/MS". MIT Undergraduate Research Journal. 8: 45–50. Archived from the original on 2013-12-24.
- ↑ Hukkanen J, Jacob P, Benowitz NL (March 2005). "Metabolism and disposition kinetics of nicotine". Pharmacological Reviews. 57 (1): 79–115. doi:10.1124/pr.57.1.3. PMID 15734728.
- ↑ "The danger of third-hand smoke". Chromatography Online. 7 (3). 22 February 2011. Archived from the original on 7 July 2012.
- ↑ Benowitz, N. L.; Herrera, B; Jacob p, 3rd (2004). "Mentholated Cigarette Smoking Inhibits Nicotine Metabolism". Journal of Pharmacology and Experimental Therapeutics. 310 (3): 1208–15. doi:10.1124/jpet.104.066902. PMID 15084646.
- ↑ "Archived copy". Archived from the original on 2015-02-17. Retrieved 2015-03-15.
- ↑ www.sciencelab.com/msds.php?msdsId=9926222 Material Safety Data Sheet L-Nicotine MSDS
- ↑ Gause, G. F. (1941). "Chapter V: Analysis of various biological processes by the study of the differential action of optical isomers". In Luyet, B. J. Optical Activity and Living Matter. A series of monographs on general physiology. 2. Normandy, Missouri: Biodynamica.
- 1 2 http://library.sciencemadness.org/library/books/the_plant_alkaloids.pdf
- ↑ "Tobacco (leaf tobacco)". Transportation Information Service.
- ↑ Lamberts, Burton L.; Dewey, Lovell J.; Byerrum, Richard U. (1959). "Ornithine as a precursor for the pyrrolidine ring of nicotine". Biochimica et Biophysica Acta. 33 (1): 22–6. doi:10.1016/0006-3002(59)90492-5. PMID 13651178.
- ↑ Dawson, R. F.; Christman, D. R.; d'Adamo, A.; Solt, M. L.; Wolf, A. P. (1960). "The Biosynthesis of Nicotine from Isotopically Labeled Nicotinic Acids1". Journal of the American Chemical Society. 82 (10): 2628–2633. doi:10.1021/ja01495a059.
- ↑ Ashihara, Hiroshi; Crozier, Alan; Komamine, Atsushi, eds. (2011-06-07). Plant metabolism and biotechnology. Cambridge: Wiley. ISBN 978-0-470-74703-2.
- ↑ Benowitz, Neal L.; Hukkanen, Janne; Jacob, Peyton (2009-01-01). Nicotine Chemistry, Metabolism, Kinetics and Biomarkers. Handbook of Experimental Pharmacology. 192. pp. 29–60. doi:10.1007/978-3-540-69248-5_2. ISBN 978-3-540-69246-1. ISSN 0171-2004. PMC 2953858. PMID 19184645.
- ↑ Baselt, Randall Clint (2014). Disposition of Toxic Drugs and Chemicals in Man (10th ed.). Biomedical Publications. pp. 1452–6. ISBN 978-0-9626523-9-4.
- ↑ Mündel T, Jones DA (July 2006). "Effect of transdermal nicotine administration on exercise endurance in men". Experimental Physiology. 91 (4): 705–13. doi:10.1113/expphysiol.2006.033373. PMID 16627574.
- 1 2 Rang H. P et al., Rang and Dale's Pharmacology 6th Edition, 2007, Elsevier, page 598
- ↑ US Code of Federal Regulations. 7 CFR 205.602 - Nonsynthetic substances prohibited for use in organic crop production
- ↑ Staff, IFOAM. Criticisms and Frequent Misconceptions about Organic Agriculture: The Counter-Arguments: Misconception Number 7 Archived October 16, 2013, at the Wayback Machine.
- ↑ USEPA (29 October 2008). "Nicotine; Notice of Receipt of Request to Voluntarily Cancel a Pesticide Registration". Federal Register: 64320–64322. Retrieved 8 April 2012.
- ↑ USEPA (3 June 2009). "Nicotine; Product Cancellation Order". Federal Register: 26695–26696. Retrieved 8 April 2012.
- ↑ Posselt, W.; Reimann, L. (1828). "Chemische Untersuchung des Tabaks und Darstellung eines eigenthümlich wirksamen Prinzips dieser Pflanze" [Chemical investigation of tobacco and preparation of a characteristically active constituent of this plant]. Magazin für Pharmacie (in German). 6 (24): 138–161.
- ↑ Henningfield JE, Zeller M (March 2006). "Nicotine psychopharmacology research contributions to United States and global tobacco regulation: a look back and a look forward". Psychopharmacology. 184 (3–4): 286–91. doi:10.1007/s00213-006-0308-4. PMID 16463054.
- ↑ Bugge (October 26, 1940). "Die Entdeckung des reinen Nikotins im Jahre 1828 an der Universität Heidelberg durch Reimann und Posselt, mit einer Beschreibung ihrer Vorläufer und mit Abb. Von P. Koenig 90 S., 29 Abb., 8. Verl. A. Geist, Bremen 1940, Pr. kart. RM. 5,——". Angewandte Chemie. 53 (43‐44): 515. doi:10.1002/ange.19400534320.
- ↑ Melsens, Louis-Henri-Frédéric (1843) "Note sur la nicotine," Annales de chimie et de physique, third series, vol. 9, pages 465-479; see especially page 470. [Note: The empirical formula that Melsens provides is incorrect because at that time, chemists used the wrong atomic mass for carbon (6 instead of 12).]
- ↑ Pinner, A.; Wolffenstein, R. (1891). "Ueber Nicotin". Berichte der Deutschen Chemischen Gesellschaft. 24: 1373–1377. doi:10.1002/cber.189102401242.
- ↑ Pinner, A. (1893). "Ueber Nicotin. Die Constitution des Alkaloïds". Berichte der Deutschen Chemischen Gesellschaft. 26: 292–305. doi:10.1002/cber.18930260165.
- ↑ Pinner, A. (1893). "Ueber Nicotin. I. Mitteilung". Archiv der Pharmazie. 231 (5–6): 378–448. doi:10.1002/ardp.18932310508.
- ↑ Pictet, Amé; Rotschy, A. (1904). "Synthese des Nicotins". Berichte der Deutschen Chemischen Gesellschaft. 37 (2): 1225–1235. doi:10.1002/cber.19040370206.
- ↑ Connolly, G. N; Alpert, H. R; Wayne, G. F.; Koh, H. (October 2007). "Trends in nicotine yield in smoke and its relationship with design characteristics among popular US cigarette brands, 1997-2005". Tobacco Control. 16 (5): e5. doi:10.1136/tc.2006.019695. PMC 2598548. PMID 17897974.
- ↑ Mineur YS, Picciotto MR (December 2010). "Nicotine receptors and depression: revisiting and revising the cholinergic hypothesis". Trends Pharmacol. Sci. 31 (12): 580–6. doi:10.1016/j.tips.2010.09.004. PMC 2991594. PMID 20965579.
- ↑ Salín-Pascual RJ1, Rosas M, Jimenez-Genchi A, Rivera-Meza BL, Delgado-Parra V (September 1996). "Antidepressant effect of transdermal nicotine patches in nonsmoking patients with major depression". J Clin Psychiatry. 57 (9): 387–9. PMID 9746444.
- ↑ Peters R, Poulter R, Warner J, Beckett N, Burch L, Bulpitt C (2008). "Smoking, dementia and cognitive decline in the elderly, a systematic review". BMC Geriatr. 8: 36. doi:10.1186/1471-2318-8-36. PMC 2642819. PMID 19105840.
- ↑ Henningfield JE, Zeller M (2009). Nicotine psychopharmacology: policy and regulatory. Handb Exp Pharmacol. Handbook of Experimental Pharmacology. 192. pp. 511–34. doi:10.1007/978-3-540-69248-5_18. ISBN 978-3-540-69246-1. PMID 19184661.
- ↑ Grizzell, JA; Echeverria, V (Jun 2014). "New insights into the mechanisms of action of cotinine and its distinctive effects from nicotine". Neurochemical Research. 40 (10): 2032–46. doi:10.1007/s11064-014-1359-2. PMID 24970109.
- ↑ Crooks, PA; Dwoskin, LP (Oct 1997). "Contribution of CNS nicotine metabolites to the neuropharmacological effects of nicotine and tobacco smoking". Biochem Pharmacol. 54 (7): 743–53. doi:10.1016/s0006-2952(97)00117-2. PMID 9353128.
- 1 2 Barreto, George E.; Iarkov, Alexander; Moran, Valentina Echeverria (Jan 2015). "Beneficial effects of nicotine, cotinine and its metabolites as potential agents for Parkinson's disease". Frontiers in Aging Neuroscience. 6: 340. doi:10.3389/fnagi.2014.00340. PMC 4288130. PMID 25620929.
- 1 2 Nielsen, Susan Searles; Franklin, Gary M.; Longstreth, W. T.; Swanson, Phillip D.; Checkoway, Harvey (2013). "Nicotine from edible Solanaceae and risk of Parkinson disease". Annals of Neurology. 74 (3): 472–477. doi:10.1002/ana.23884. PMC 4864980. PMID 23661325.
Further reading
- Bilkei-Gorzo A; Rácz I; Michel K; Darvas M; Rafael Maldonado López; Zimmer A. (2008). "A common genetic predisposition to stress sensitivity and stress-induced nicotine craving". Biol. Psychiatry. 63 (2): 164–71. doi:10.1016/j.biopsych.2007.02.010. PMID 17570348.
- Gorrod, John W.; Peyton, Jacob, III, eds. (November 16, 1999). Analytical Determination of Nicotine and Related Compounds and their Metabolites. Amsterdam: Elsevier. ISBN 978-0-08-052551-8.
- Willoughby JO, Pope KJ, Eaton V (Sep 2003). "Nicotine as an antiepileptic agent in ADNFLE: an N-of-one study". Epilepsia. 44 (9): 1238–40. doi:10.1046/j.1528-1157.2003.11903.x. PMID 12919397.
- Minna JD (Jan 2003). "Nicotine exposure and bronchial epithelial cell nicotinic acetylcholine receptor expression in the pathogenesis of lung cancer". J Clin Invest. 111 (1): 31–3. doi:10.1172/JCI17492. PMC 151841. PMID 12511585.
- Fallon JH, Keator DB, Mbogori J, Taylor D, Potkin SG (Mar 2005). "Gender: a major determinant of brain response to nicotine". Int J Neuropsychopharmacol. 8 (1): 17–26. doi:10.1017/S1461145704004730. PMID 15579215.
- West KA, Brognard J, Clark AS, et al. (Jan 2003). "Rapid Akt activation by nicotine and a tobacco carcinogen modulates the phenotype of normal human airway epithelial cells". J Clin Invest. 111 (1): 81–90. doi:10.1172/JCI16147. PMC 151834. PMID 12511591.
- National Institute on Drug Abuse
- Mayer B (2014). "How much nicotine kills a human? Tracing back the generally accepted lethal dose to dubious self-experiments in the nineteenth century". Arch. Toxicol. 88 (1): 5–7. doi:10.1007/s00204-013-1127-0. PMC 3880486. PMID 24091634.
External links
| Wikimedia Commons has media related to Nicotine. |
- Description of nicotine mechanisms
- Erowid Nicotine Vault : Nicotine Material Safety Data Sheet
- Thomas, Gareth AO; Rhodes, John; Ingram, John R (2005). "Mechanisms of Disease: Nicotine – a review of its actions in the context of gastrointestinal disease". Nature Clinical Practice Gastroenterology & Hepatology. 2 (11): 536–44. doi:10.1038/ncpgasthep0316. PMID 16355159.
- CDC – NIOSH Pocket Guide to Chemical Hazards

