Transgender hormone therapy (male-to-female)
| Part of a series on |
| Transgender topics |
|---|
 |
|
Health care and medicine
|
|
Rights issues |
|
Society and culture |
|
By country
|
|
|
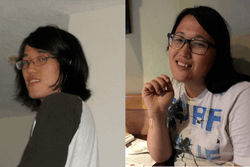
Transgender hormone therapy of the male-to-female (MTF) type, also known as feminizing hormone therapy, is hormone therapy and sex reassignment therapy to change the secondary sexual characteristics of transgender people from masculine (or androgynous) to feminine.[1][2][3][4][5][6] It is one of two types of transgender hormone therapy (the other being female-to-male) and is predominantly used to treat transgender women and other transfeminine individuals. Some intersex people also take this form of therapy, according to their personal needs and preferences.
The purpose of the therapy is to cause the development of the secondary sex characteristics of the desired sex, such as breasts and a feminine pattern of hair, fat, and muscle distribution. It cannot undo many of the changes produced by naturally occurring puberty, which may necessitate surgery and other treatments to reverse (see below). The medications used for the MTF therapy include estrogens, antiandrogens, progestogens, and gonadotropin-releasing hormone modulators (GnRH modulators).
While the therapy cannot undo the effects of a person's first puberty, developing secondary sex characteristics associated with a different gender can relieve some or all of the distress and discomfort associated with gender dysphoria, and can help the person to "pass" or be seen as the gender they identify with. Introducing exogenous hormones into the body impacts it at every level and many patients report changes in energy levels, mood, appetite, etc. The goal of the therapy, and indeed all somatic treatments, is to provide patients with a more satisfying body that is more congruent with their gender identity.
Medical uses
- To produce feminization and/or demasculinization in transgender women and transfeminine non-binary individuals.
- To produce feminization and/or demasculinization in intersex people.
Requirements and accessibility
Contraindications
Some medical conditions may be a reason to withhold hormone replacement therapy because of the harm it could cause to the patient. Such interfering factors are described in medicine as contraindications.
Absolute contraindications – those that can cause life-threatening complications, and in which hormone replacement therapy should never be used – include histories of estrogen-sensitive cancer (e.g., breast cancer), thrombosis or embolism (unless the patient receives concurrent anticoagulants), or macroprolactinoma. In such cases, the patient should be monitored by an oncologist, hematologist or cardiologist, or neurologist, respectively.
Relative contraindications – in which the benefits of HRT may outweigh the risks, but caution should be used – include:
- Liver disease, kidney disease, heart disease, or stroke
- Risk factors for heart disease, such as high cholesterol, diabetes, obesity, or smoking
- Family history of breast cancer or thromboembolic disease
- Gallbladder disease
- Circulation or clotting conditions, such as peripheral vascular disease, polycythemia vera, sickle-cell anemia, paroxysmal nocturnal hemoglobinuria, hyperlipidemia, hypertension, factor V Leiden, prothrombin mutation, antiphospholipid antibodies, anticardiolipin antibodies, lupus anticoagulants, plasminogen or fibrinolysis disorders, protein C deficiency, protein S deficiency, or antithrombin III deficiency.
As dosages increase, risks increase as well. Therefore, patients with relative contraindications may start at low dosages and increase gradually.
Safety
Hormone therapy for transgender individuals has been shown in medical literature to be safe when supervised by a qualified medical professional.[7]
Interactions
Inducers of CYP3A4 and other cytochrome P450 enzymes can reduce the effects of MTF HRT.
Types of therapy
A variety of different sex-hormonal medications are used in feminizing hormone therapy for transgender women.[1][2][3][4] These include estrogens to induce feminization and suppress testosterone levels; antiandrogens such as androgen receptor antagonists, antigonadotropins, GnRH modulators, and 5α-reductase inhibitors to further oppose the effects of androgens like testosterone; and progestogens for various possible though uncertain benefits.[1][2][3][4]
| Medication | Brand names | Type | Route | Dosage | |||||
|---|---|---|---|---|---|---|---|---|---|
| Estradiol | Various | Estrogen | Oral | 0.25–8 mg/day | |||||
| Various | Sublingual | 0.25–8 mg/day | |||||||
| Climara, Vivelle, others | Transdermal (patches) | 6.25–400 μg/day | |||||||
| Divigel, EstroGel, Sandrena | Transdermal (gel) | 0.5–4.5 mg/day | |||||||
| Estradiol valerate | Progynova | Estrogen | Oral | 0.25–8 mg/day | |||||
| Delestrogen, Progynon Depot | Injection (IM or SC) | 2–10 mg/week or 5–30 mg/2 weeks | |||||||
| Estradiol cypionate | Depo-Estradiol | Estrogen | Injection (IM or SC) | 2–10 mg/week or 5–30 mg/2 weeks | |||||
| Estradiol benzoate | Progynon-B | Estrogen | Injection (IM or SC) | 0.5–1.5 mg/2–3 days | |||||
| Conjugated estrogensa | Premarin | Estrogen | Oral | 0.625–10 mg/day | |||||
| Ethinylestradiola | Various | Estrogen | Oral | 20–100 μg/day | |||||
| Estriol | Ovestin, Synapause | Estrogen | Oral | 4–6 mg/day | |||||
| Spironolactone | Aldactone | Antiandrogen | Oral | 100–400 mg/day | |||||
| Cyproterone acetate | Androcur | Antiandrogen; Progestogen | Oral | 25–50 mg/day | |||||
| Flutamidea | Eulexin | Antiandrogen | Oral | 125–750 mg/day (divided doses) | |||||
| Nilutamidea | Anandron, Nilandron | Antiandrogen | Oral | 300 mg/day | |||||
| Bicalutamide | Casodex | Antiandrogen | Oral | 50 mg/day | |||||
| GnRH analogue | Various | GnRH modulator | Parenteral (various) | Variable | |||||
| Elagolix | Orilissa | GnRH antagonist | Oral | 150 mg/day or 200 mg/twice a day[8] | |||||
| Finasteride | Propecia | 5α-Reductase inhibitor | Oral | 1–5 mg/day | |||||
| Dutasteride | Avodart | 5α-Reductase inhibitor | Oral | 0.25–0.5 mg/day | |||||
| Progesterone | Prometrium, Utrogestan | Progestogen | Oral | 100–400 mg/day | |||||
| Medroxyprogesterone acetate | Provera | Progestogen | Oral | 2.5–40 mg/day | |||||
| Depo-Provera | Injection (IM) | 150 mg/3 months | |||||||
| Depo-SubQ Provera 104 | Injection (SC) | 104 mg/3 months | |||||||
| Hydroxyprogesterone caproate | Proluton | Progestogen | Injection (IM) | 250 mg/week | |||||
| Dydrogesterone | Duphaston | Progestogen | Oral | 20 mg/day | |||||
| Footnotes: a = No longer recommended for use in transgender women. Miscellaneous: Direct link to table. Sources: Guidelines: [1][3][5][6][9] Reviews/book chapters: [4][10][11][12][13][14][15][16][17][18][19][20][21][22][23][24][25][26] | |||||||||
Estrogens
Estrogens are the major sex hormones in women, and are responsible for the development and maintenance of feminine secondary sexual characteristics, such as breasts, wide hips, and a feminine pattern of fat distribution.[4] Estrogens act by binding to and activating the estrogen receptor (ER), their biological target in the body.[29] A variety of different forms of estrogens are available and used medically.[29] The most common estrogens used in transgender women include estradiol, which is the predominant natural estrogen in women, and estradiol esters such as estradiol valerate and estradiol cypionate, which are prodrugs of estradiol.[1][4][29] Conjugated estrogens (Premarin), which are used in menopausal hormone therapy, and ethinylestradiol, which is used in birth control pills, have been used in transgender women in the past, but are no longer recommended and are rarely used today due to their higher risks of blood clots and cardiovascular problems.[4][1][2][5] Estrogens may be administered orally, sublingually, transdermally/topically (via patch or gel), rectally, by intramuscular or subcutaneous injection, or by an implant.[29][10][30][31][32] Parenteral (non-oral) routes are preferred, owing to a minimal or negligible risk of blood clots and cardiovascular issues.[5][33][34][35][36]
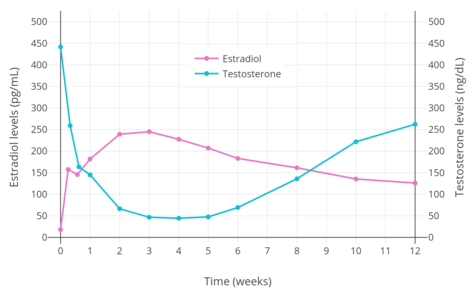
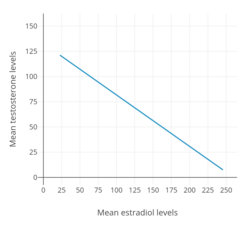
In addition to producing feminization, estrogens have antigonadotropic effects and suppress gonadal sex hormone production.[10][28][16] They are mainly responsible for the suppression of testosterone levels in transgender women.[10][16] Levels of estradiol of 200 pg/mL and above suppress testosterone levels by about 90%, while estradiol levels of 500 pg/mL and above suppress testosterone levels by about 95%, or to an equivalent extent as surgical castration and GnRH modulators.[37][38] Lower levels of estradiol can also considerably but incompletely suppress testosterone production.[28] When testosterone levels are insufficiently suppressed by estradiol alone, antiandrogens can be used to suppress or block the effects of residual testosterone.[10] Oral estradiol often has difficulty adequately suppressing testosterone levels, due to the relatively low estradiol levels achieved with it.[28][39][40]
Prior to orchiectomy or sex reassignment surgery, the doses of estrogens used in transgender women are often higher than replacement doses used in cisgender women.[17][41][42] This is to help suppress testosterone levels.[41] The Endocrine Society (2017) recommends maintaining estradiol levels roughly within the normal average range for premenopausal women of about 100 to 200 pg/mL.[1] However, it notes that physiological levels of estradiol are unable to suppress testosterone levels into the female range.[1] In addition, the Endocrine Society recommends dosages of injected estradiol esters that result in estradiol levels that can markedly exceed the normal female range (e.g., 10 mg/week estradiol valerate, which results in peak estradiol levels of 1,250 pg/mL on average).[1][43][44] Dosages of estrogens can be reduced after an orchiectomy (surgical removal of the gonads) or sex reassignment surgery, when testosterone suppression is no longer needed.[5]
Antiandrogens
Androgens, such as testosterone and dihydrotestosterone (DHT), are the major sex hormones in people with testes, and are responsible for the development and maintenance of masculine secondary sexual characteristics, such as a deep voice, broad shoulders, and a masculine pattern of hair, muscle, and fat distribution. In addition, they stimulate sex drive and the frequency of spontaneous erections and are responsible for acne, body odor, and scalp hair loss. Androgens act by binding to and activating the androgen receptor, their biological target in the body.
In contrast to androgens, antiandrogens are medications that prevent the effects of androgens in the body.[45][46] They do this by blocking androgens from binding to the androgen receptor and/or by inhibiting or suppressing the production of androgens.[45] Antiandrogens that directly block the androgen receptor are known as androgen receptor antagonists, while antiandrogens that inhibit the enzymatic synthesis of androgens are known as androgen synthesis inhibitors and antiandrogens that suppress androgen production in the gonads are known as antigonadotropins.[46] Estrogens and progestogens are antigonadotropins and hence are functional antiandrogens.[10][47][48][49]
The purpose of antiandrogens is to suppress or block residual testosterone that is not suppressed by estrogens alone.[10][45][16] Antiandrogens are not necessarily needed if testosterone levels are in the normal female range with an estrogen alone.[10][45][16]
Steroidal antiandrogens
Steroidal antiandrogens are antiandrogens that resemble steroid hormones like testosterone and progesterone in chemical structure.[50] They are the most commonly used antiandrogens in transgender women.[2] Spironolactone (Aldactone), which is relatively safe and inexpensive, is the most frequently used antiandrogen in the United States.[51][52] Cyproterone acetate (Androcur), which is unavailable in the United States, is widely used in Europe, Canada, and the rest of the world.[2][45][51][53] Medroxyprogesterone acetate (Provera, Depo-Provera), a similar medication, is sometimes used in place of cyproterone acetate in the United States.[54][55]
Spironolactone is an antimineralocorticoid (antagonist of the mineralocorticoid receptor) and potassium-sparing diuretic, which is mainly used to treat high blood pressure, edema, high aldosterone levels, and low potassium levels caused by other diuretics, among other uses.[56] Spironolactone is an antiandrogen as a secondary and originally unintended action.[56] It works as an antiandrogen mainly by acting as an androgen receptor antagonist.[57] The medication is also a weak steroidogenesis inhibitor, and inhibits the enzymatic synthesis of androgens.[58][57][59] However, this action is of very low potency, and spironolactone has mixed and highly inconsistent effects on hormone levels.[58][57][59][60][61] In any case, testosterone levels are usually unchanged by spironolactone.[58][57][59][60][61] In accordance, a relatively large study found no effect of spironolactone on testosterone levels in transgender women.[28] Spironolactone is described as a relatively weak antiandrogen.[62][63][64] It is widely used in the treatment of acne, excessive hair growth, and hyperandrogenism in women, who have much lower testosterone levels than men.[60][61] Because of its antimineralocorticoid activity, spironolactone has antimineralocorticoid side effects[65] and can cause high potassium levels.[66][67] Hospitalization and/or death can result from high potassium levels,[66][67][68] but the risk of high potassium levels in people taking spironolactone appears to be minimal in those without risk factors for it.[61][69][70] As such, monitoring of potassium levels may not be necessary in most cases.[61][69][70] Spironolactone has been found to decrease the bioavailability of oral estradiol.[28] Although widely employed, the use of spironolactone as an antiandrogen in transgender women has recently been questioned due to its various shortcomings.[28]
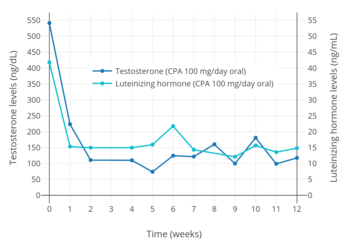
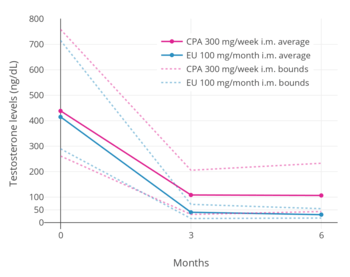
Cyproterone acetate is an antiandrogen and progestin which is used in the treatment of numerous androgen-dependent conditions and is also used as a progestogen in birth control pills.[73][74] It works primarily as an antigonadotropin, secondarily to its potent progestogenic activity, and strongly suppresses gonadal androgen production.[73][16] Cyproterone acetate at a dosage of 10 mg/day has been found to lower testosterone levels in men by about 50 to 70%,[75][76][77][78] while a dosage of 100 mg/day has been found to lower testosterone levels in men by about 75%.[79][72] The combination of 25 mg/day cyproterone acetate and a moderate dosage of estradiol has been found to suppress testosterone levels in transgender women by about 95%.[80] In addition to its actions as an antigonadotropin, cyproterone acetate is an androgen receptor antagonist.[73][45] However, this action is relatively insignificant at low dosages, and is more important at the high doses of cyproterone acetate that are used in the treatment of prostate cancer (100–300 mg/day).[81][82] Cyproterone acetate can cause elevated liver enzymes and liver damage, including liver failure.[45][83] However, this occurs mostly in prostate cancer patients who take very high doses of cyproterone acetate, and liver toxicity has not been reported in transgender women.[45] Cyproterone acetate also has a variety of other adverse effects and risks, such as depression, blood clots, benign brain tumors, glucocorticoid side effects, and cardiovascular side effects, among others.[16][45][84] Periodic monitoring of liver enzymes and prolactin levels may be advisable during cyproterone acetate therapy.
Medroxyprogesterone acetate is a progestin that is related to cyproterone acetate and is sometimes used as an alternative to it.[54][55] It is specifically used as an alternative to cyproterone acetate in the United States, where cyproterone acetate is not approved for medical use and is unavailable.[54][55] Medroxyprogesterone acetate suppresses testosterone levels in transgender women similarly to cyproterone acetate.[55][28] Oral medroxyprogesterone acetate has been found to suppress testosterone levels in men by about 30 to 75% across a dosage range of 20 to 100 mg/day.[85][86][87][88][89] In contrast to cyproterone acetate however, medroxyprogesterone acetate is not an androgen receptor antagonist, and instead has very weak androgenic activity.[29][90] However, the clinical relevance of this androgenic activity is doubtful at typical clinical dosages.[90] Medroxyprogesterone acetate has similar side effects and risks as cyproterone acetate, but lacks the liver issues of cyproterone acetate and does not seem to share its risk of depression.[91][92][65]
Numerous other progestogens and by extension antigonadotropins have been used to suppress testosterone levels in men and are likely useful for such purposes in transgender women as well.[93][94][95][96][97][98][99] Progestogens alone are in general able to suppress testosterone levels in men by a maximum of about 70 to 80%, or to just above female/castrate levels when used at sufficiently high doses.[100][101][102]
Nonsteroidal antiandrogens
Nonsteroidal antiandrogens are antiandrogens that are nonsteroidal and hence unrelated to steroid hormones in terms of chemical structure.[50][103] These medications are primarily used in the treatment of prostate cancer,[103] but are also used for other purposes such as the treatment of acne, excessive facial/body hair growth, and high androgen levels in women.[104][105][106] Unlike steroidal antiandrogens, nonsteroidal antiandrogens are highly selective for the androgen receptor and act as pure androgen receptor antagonists.[103][107] Similarly to spironolactone however, they do not lower androgen levels, and instead work exclusively by preventing androgens from activating the androgen receptor.[103][107] The nonsteroidal antiandrogens are more efficacious androgen receptor antagonists than are the steroidal antiandrogens,[50][108] and for this reason, in conjunction with GnRH modulators, have largely replaced steroidal antiandrogens in the treatment of prostate cancer.[103][109]
The nonsteroidal antiandrogens that have been used in transgender women include the first-generation medications flutamide (Eulexin), nilutamide (Anandron, Nilandron), and bicalutamide (Casodex).[11][5][3][110]:477 Newer and even more efficacious second-generation nonsteroidal antiandrogens like enzalutamide (Xtandi) and apalutamide (Erleada) have also been introduced, but are very expensive due to generics being unavailable, and have not been used in transgender women.[111][112] Flutamide and nilutamide have relatively high toxicity, including considerable risks of liver damage and lung disease.[113][104] Due to its risks, the use of flutamide in cisgender and transgender women is now discouraged.[104][5] Flutamide and nilutamide have largely been superseded by bicalutamide in clinical practice,[114][115] with it accounting for almost 90% of nonsteroidal antiandrogen prescriptions in the United States by the mid-2000s.[116][107] Bicalutamide is said to have excellent tolerability and safety relative to flutamide and nilutamide, as well as in comparison to cyproterone acetate.[117][118][119] It has few to no side effects in women.[105][106] The medication does have a small risk of elevated liver enzymes and has been associated with very rare cases of liver damage and lung disease however.[113][120]
Nonsteroidal antiandrogens like bicalutamide may be a favorable option in particular for transgender women who wish to preserve sex drive, sexual function, and/or fertility, relative to antiandrogens that suppress testosterone levels and can greatly disrupt these functions like cyproterone acetate and GnRH modulators.[121][122][123]
GnRH modulators
GnRH modulators are powerful antigonadotropins and hence functional antiandrogens.[124] In both males and females, gonadotropin-releasing hormone (GnRH) is produced in the hypothalamus and induces the secretion of the gonadotropins luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the pituitary gland.[124] The gonadotropins signal the gonads to make sex hormones such as testosterone and estradiol.[124] GnRH modulators bind to and inhibit the GnRH receptor, thereby preventing gonadotropin release.[124] As a result of this, GnRH modulators are able to completely shut-down gonadal sex hormone production, and can decrease testosterone levels in men and transgender women by about 95%, or to an equivalent extent as surgical castration.[124][125][126] GnRH modulators are also commonly known as GnRH analogues.[124] However, not all clinically used GnRH modulators are analogues of GnRH.[127][128]
There are two types of GnRH modulators: GnRH agonists and GnRH antagonists.[124] These medications have the opposite action on the GnRH receptor but paradoxically have the same therapeutic effects.[124] GnRH agonists, such as leuprorelin (Lupron), goserelin (Zoladex), and buserelin (Suprefact), are GnRH receptor superagonists, and work by producing profound desensitization of the GnRH receptor such that the receptor becomes non-functional.[124][125] This occurs because GnRH is normally released in pulses, but GnRH agonists are continuously present, and this results in excessive downregulation of the receptor and ultimately a complete loss of function.[129][130][124] At the initiation of treatment, GnRH agonists are associated with a "flare" effect on hormone levels due to acute overstimulation of the GnRH receptor.[124][131] In men, LH levels increase by up to 800%, while testosterone levels increase to about 140 to 200% of baseline.[132][131] Gradually however, the GnRH receptor desensitizes; testosterone levels peak after about 2 to 4 days, return to baseline after about 7 to 8 days, and are reduced to castrate levels within 2 to 4 weeks.[131] Antigonadotropins such as estrogens and cyproterone acetate can be used to diminish or prevent the testosterone flare caused by GnRH agonists.[133][134][10][135] In contrast to GnRH agonists, GnRH antagonists, such as degarelix (Firmagon) and elagolix (Orilissa), work by binding to the GnRH receptor without activating it, thereby displacing GnRH from the receptor and preventing its activation.[124] Unlike with GnRH agonists, there is no initial surge effect with GnRH antagonists, and the therapeutic effects are immediate; sex hormone levels are reduced to castrate levels within a few days.[124][125]
GnRH modulators are highly effective for testosterone suppression in transgender women and have few or no side effects when sex hormone deficiency is avoided with concomitant estrogen therapy.[1][136] However, GnRH modulators tend to be very expensive, and are often denied by medical insurance.[1][137] GnRH modulator therapy is much less economical than surgical castration, and is less convenient than surgical castration in the long-term as well.[138] Because of their costs, many transgender women cannot afford GnRH modulators and must use other, often less effective options for testosterone suppression.[1][137] GnRH agonists are prescribed as standard practice for transgender women in the United Kingdom however, where the National Health Service (NHS) covers them.[137] Another drawback of GnRH modulators is that most of them are peptides and are not orally active, requiring administration by injection, implant, or nasal spray.[133] However, the first non-peptide and orally active GnRH antagonist, elagolix (Orilissa), has recently been introduced for medical use.[128] As with other GnRH modulators, it is currently very expensive.[139]
In adolescents of either sex with relevant indicators, GnRH modulators can be used to stop undesired pubertal changes for a period without inducing any changes toward the sex with which the patient currently identifies. There is considerable controversy over the earliest age at which it is clinically, morally, and legally safe to use GnRH modulators, and for how long. The sixth edition of the World Professional Association for Transgender Health's Standards of Care permit it from Tanner stage 2 but do not allow the addition of hormones until age 16, which could be five or more years later. Sex steroids have important functions in addition to their role in puberty, and some skeletal changes (such as increased height) that may be considered masculine are not hindered by GnRH modulators.
5α-Reductase inhibitors
5α-Reductase inhibitors, a type of androgen synthesis inhibitor, work not by decreasing testosterone levels but rather by preventing the conversion and hence potentiation of testosterone into the more potent androgen dihydrotestosterone (DHT) in certain tissues such as the skin, hair follicles, and prostate gland. They are used in the treatment of prostate disorders and pattern hair loss in men, and have also been found to be effective in the treatment of excessive hair growth in women. Since they do not decrease testosterone levels however, they do not affect the actions of testosterone in most of the body. The two main 5α-reductase inhibitors that are used clinically are finasteride (Propecia) and dutasteride (Avodart). DHT levels can be lowered up to about 70% with finasteride and by up to about 99% or more with dutasteride.[140][141] Dutasteride has been found to be more effective than finasteride in the treatment of pattern hair loss.[142][143]
Progestogens
Progesterone, a progestogen, is the other of the two major sex hormones in women.[133] It is mainly involved in the regulation of the female reproductive system, the menstrual cycle, pregnancy, and lactation.[133] The non-reproductive effects of progesterone are fairly insignificant.[144] Unlike estrogens, progesterone is not known to be involved in the development of female secondary sexual characteristics, and hence is not believed to contribute to feminization in women.[2][55] One area of particular interest in terms of the effects of progesterone in women is breast development.[145][146][147] Estrogens are responsible for the development of the ductal and connective tissues of the breasts and the deposition of fat into the breasts during puberty in girls.[145][146] Conversely, high levels of progesterone, in conjunction with other hormones such as prolactin, are responsible for the lobuloalveolar maturation of the mammary glands during pregnancy.[145][146] This allows for lactation and breastfeeding after childbirth.[145][146] Although progesterone causes the breasts to change during pregnancy, the breasts undergo involution and revert to their pre-pregnancy composition and size after the cessation of breastfeeding.[145][148][146] Every pregnancy, lobuloalveolar maturation occurs again anew.[145][146]
There are two types of progestogens: progesterone, which is the natural and bioidentical hormone in the body; and progestins, which are synthetic progestogens.[29] There are dozens of clinically used progestins.[29][149][150] Certain progestins, namely cyproterone acetate and medroxyprogesterone acetate, and as described previously, are used at high doses as functional antiandrogens due to their antigonadotropic effects to help suppress testosterone levels in transgender women.[54][55] Aside from the specific use of testosterone suppression however, there are no other indications of progestogens in transgender women at present.[2] In relation to this, the use of progestogens in transgender women is controversial, and they are not otherwise routinely prescribed or recommended.[2][5][6][14][18][151] Besides progesterone, cyproterone acetate, and medroxyprogesterone acetate, other progestogens that have been reported to have been used in transgender women include hydroxyprogesterone caproate, dydrogesterone, and norethisterone acetate.[152][153][18][154][5] Progestins in general largely have the same progestogenic effects however, and in theory, any progestin could be used in transgender women.[29]
The clinical research that has studied the use of progestogens in transgender women is very limited.[2][147] Some patients and clinicians believe, on the basis of anecdotal and subjective claims, that progestogens may provide benefits such as improved breast and/or nipple development, mood, and libido in transgender women.[4][3][147] There are no clinical studies to support such reports at present.[2][4][147] No clinical study has assessed the use of progesterone in transgender women, and only a couple of studies have compared the use of progestins (specifically cyproterone acetate and medroxyprogesterone acetate) versus the use of no progestogen in transgender women.[147][155][136] These studies, albeit limited in the quality of their findings, found no benefit of progestogens on breast development in transgender women.[147][136][14] This has also been the case in limited clinical experience.[156] These reports are in accordance with the normal and even above-average breast development in women with complete androgen insensitivity syndrome, who lack progesterone and have no lobuloalveolar development of the mammary glands on histological examination.[157][158] It is noteworthy that epithelial tissue, which makes up lobuloalveolar tissue, normally comprises only about 10 to 15% of the tissue of the breasts.[159][160][161][162] Progestogens have some antiestrogenic effects in the breasts, for instance decreasing expression of the estrogen receptor and increasing expression of estrogen-metabolizing enzymes,[163][164][165][166] and for this reason, have been used to treat breast pain and benign breast disorders.[167][168][169][170] Progesterone levels during female puberty do not normally increase importantly until near the end of puberty in cisgender girls,[171] a point by which most or all breast development has already been completed, and there has been some concern that premature exposure to progestogens is unphysiological and might compromise ultimate breast growth.[147][172] Although the influence of progesterone on breast development is uncertain, progesterone is thought to cause reversible breast enlargement during the menstrual cycle due to local fluid retention in the breasts.[173][174] This may give a misleading appearance of breast growth, and might contribute to anecdotal reports of improved breast size and/or shape with progesterone in transgender women.[173][174] In terms of the effects of progestogens on sex drive, one study assessed the use of dydrogesterone to improve sexual desire in transgender women and found no benefit.[154] Another study likewise found that oral progesterone did not improve sexual function in cisgender women.[175]
Though the role of progestogens in visible breast development is uncertain, progestogens are essential for lobuloalveolar maturation of the mammary glands, and hence are required for any transgender woman who wishes to lactate or breastfeed.[145][176][147] A study found full lobuloalveolar maturation of the mammary glands on histological examination in transgender women treated with an estrogen and high-dose cyproterone acetate.[177][178][179]
Progestogens can have adverse effects.[14][18][29][149][180][31] Oral progesterone has inhibitory neurosteroid effects and can produce side effects such as sedation, mood changes, and alcohol-like effects.[29][181][182] Many progestins have off-target activity, such as androgenic, antiandrogenic, glucocorticoid, and antimineralocorticoid activity, and these activities likewise can contribute unwanted side effects.[29][149] Furthermore, the addition of a progestin to estrogen therapy has been found to increase the risk of blood clots, cardiovascular disease (e.g., coronary heart disease and stroke), and breast cancer compared to estrogen therapy alone in postmenopausal women.[20][18][14][183] Although it is unknown if these health risks of progestins occur in transgender women similarly, it cannot be ruled out that they do.[20][18][14] High-dose progestogens increase the risk of benign brain tumors including prolactinomas and meningiomas as well.[184][185] Because of their potential detrimental effects and lack of supported benefits, some researchers have argued that, aside from the purpose of testosterone suppression, progestogens should not generally be used or advocated in transgender women or should only be used for a limited duration (e.g., 2–3 years).[20][14][5][6][20][151] Conversely, other researchers have argued that the risks of progestogens in transgender women are likely minimal, and that in light of potential albeit hypothetical benefits, should be used if desired.[3] In general, some transgender women respond favorably to the effects of progestogens, while others respond negatively.[3]
Progesterone is most commonly taken orally.[29][183] However, oral progesterone has very low bioavailability, and produces only weak and inadequate progestogenic effects even at high doses.[186][187][183][188][189] In accordance, and in contrast to progestins, oral progesterone has no antigonadotropic effects in men even at high doses.[181][190] Progesterone can also be taken by various parenteral (non-oral) routes, including sublingually, rectally, and by intramuscular or subcutaneous injection.[29][169][191] These routes do not have the bioavailability issues of oral progesterone, and accordingly, can produce considerable antigonadotropic and other progestogenic effects.[29][188][192] Transdermal progesterone is poorly effective, owing to absorption issues.[29][169][189] Progestins are usually taken orally.[29] In contrast to progesterone, most progestins have high oral bioavailability, and can produce full progestogenic effects with oral administration.[29] Some progestins, such as medroxyprogesterone acetate and hydroxyprogesterone caproate, are or can be used by intramuscular or subcutaneous injection instead.[193][169] Almost all progestins, with the exception of dydrogesterone, have antigonadotropic effects.[29]
Effects
The main effects of hormone therapy in transgender women are feminization and demasculinization, and are as follows:
| Effect | Time to expected onset of effecta | Time to expected maximum effecta,b | Permanency if hormone therapy is stopped | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Breast development and nipple/areolar enlargement | 2–6 months | 1–3 years | Permanent | ||||||
| Thinning/slowed growth of facial/body hair | 4–12 months | >3 yearsc | Reversible | ||||||
| Cessation/reversal of male-pattern scalp hair loss | 1–3 months | 1–2 yearsd | Reversible | ||||||
| Softening of skin/decreased oiliness and acne | 3–6 months | Unknown | Reversible | ||||||
| Redistribution of body fat in a feminine pattern | 3–6 months | 2–5 years | Reversible | ||||||
| Decreased muscle mass/strength | 3–6 months | 1–2 yearse | Reversible | ||||||
| Widening and rounding of the pelvisf | Unspecified | Unspecified | Permanent | ||||||
| Changes in mood, emotionality, and behavior | Unspecified | Unspecified | Reversible | ||||||
| Decreased sex drive | 1–3 months | 3–6 months | Reversible | ||||||
| Decreased spontaneous/morning erections | 1–3 months | 3–6 months | Reversible | ||||||
| Erectile dysfunction and decreased ejaculate volume | 1–3 months | Variable | Reversible | ||||||
| Decreased sperm production/fertility | Unknown | >3 years | Reversible or permanentg | ||||||
| Decreased testicle size | 3–6 months | 2–3 years | Unknown | ||||||
| Decreased penis size | Noneh | Not applicable | Not applicable | ||||||
| Decreased prostate gland size | Unspecified | Unspecified | Unspecified | ||||||
| Voice changes | Nonei | Not applicable | Not applicable | ||||||
| Footnotes: a = Estimates represent published and unpublished clinical observations. b = Time at which further changes are unlikely at maximum maintained dose. Maximum effects vary widely depending on genetics, body habitus, age, and status of gonad removal. Generally, older individuals with intact gonads may have less feminization overall. c = Complete removal of male facial and body hair requires electrolysis, laser hair removal, or both. Temporary hair removal can be achieved with shaving, epilating, waxing, and other methods. d = Familial scalp hair loss may occur if estrogens are stopped. e = Varies significantly depending on the amount of physical exercise. f = Occurs only in individuals of pubertal age who have not yet completed epiphyseal closure. g = Additional research is needed to determine permanency, but a permanent impact of estrogen therapy on sperm quality is likely and sperm preservation options should be counseled on and considered before initiation of therapy h = Conflicting reports, with none reported observed in transgender women but significant albeit minor reduction of penis size reported in men with prostate cancer on androgen deprivation therapy.[194][195][196][197] i = Treatment by speech pathologists for voice training is effective. Miscellaneous: Direct link to table. Sources: Guidelines: [1][2][6] Reviews/book chapters: [4][198][14][199][16][20][23][24] Studies: [200][201] | |||||||||
Physical changes
Breast development

Breast, nipple, and areolar development varies considerably depending on genetics, body composition, age of HRT initiation, and many other factors. Development can take a couple years to nearly a decade for some. However, many transgender women report there is often a "stall" in breast growth during transition, or significant breast asymmetry. Transgender women on HRT often experience less breast development than cisgender women (especially if started after young adulthood). For this reason, many seek breast augmentation. Transgender patients opting for breast reduction are rare. Shoulder width and the size of the rib cage also play a role in the perceivable size of the breasts; both are usually larger in transgender women, causing the breasts to appear proportionally smaller. Thus, when a transgender woman opts to have breast augmentation, the implants used tend to be larger than those used by cisgender women.[203]
In clinical trials, cisgender women have used stem cells from fat to regrow their breasts after mastectomies. This could someday eliminate the need for implants for transgender women.[204]
In transgender women on HRT, as in cisgender women during puberty, breast ducts and Cooper's ligaments develop under the influence of estrogen. Progesterone causes the milk sacs (mammary alveoli) to develop, and with the right stimuli, a transgender woman may lactate. Additionally, HRT often makes the nipples more sensitive to stimulation.
Skin changes
The uppermost layer of skin, the stratum corneum, becomes thinner and more translucent. Spider veins may appear or be more noticeable as a result. Collagen decreases, and tactile sensation increases. The skin becomes softer,[205] more susceptible to tearing and irritation from scratching or shaving, and slightly lighter in color because of a slight decrease in melanin.
Sebaceous gland activity (which is triggered by androgens) lessens, reducing oil production on the skin and scalp. Consequently, the skin becomes less prone to acne. It also becomes drier, and lotions or oils may be necessary.[203][206] The pores become smaller because of the lower quantities of oil being produced. Many apocrine glands – a type of sweat gland – become inactive, and body odor decreases. Remaining body odor becomes less metallic, sharp, or acrid, and more sweet and musky.
As subcutaneous fat accumulates,[203] dimpling, or cellulite, becomes more apparent on the thighs and buttocks. Stretch marks (striae distensae) may appear on the skin in these areas. Susceptibility to sunburn increases, possibly because the skin is thinner and less pigmented.
Hair changes
Antiandrogens affect existing facial hair only slightly; patients may see slower growth and some reduction in density and coverage. Those who are less than a decade past puberty and/or lack a significant amount of facial hair may have better results. Patients taking antiandrogens tend to have better results with electrolysis and laser hair removal than those who are not. In patients in their teens or early twenties, antiandrogens prevent new facial hair from developing if testosterone levels are within the normal female range.[203][206]
Body hair (on the chest, shoulders, back, abdomen, buttocks, thighs, tops of hands, and tops of feet) turns, over time, from terminal ("normal") hairs to tiny, blonde vellus hairs. Arm, perianal, and perineal hair is reduced but may not turn to vellus hair on the latter two regions (some cisgender women also have hair in these areas). Underarm hair changes slightly in texture and length, and pubic hair becomes more typically female in pattern. Lower leg hair becomes less dense. All of these changes depend to some degree on genetics.[203][206]
Head hair may change slightly in texture, curl, and color. This is especially likely with hair growth from previously bald areas. Eyebrows do not change because they are not androgenic.[207]
Eye changes
The lens of the eye changes in curvature.[208][209][210][211] Because of decreased androgen levels, the meibomian glands (the sebaceous glands on the upper and lower eyelids that open up at the edges) produce less oil. Because oil prevents the tear film from evaporating, this change may cause dry eyes.[212][213][214][215][216]
Fat changes
The distribution of adipose (fat) tissue changes slowly over months and years. HRT causes the body to accumulate new fat in a typically feminine pattern, including in the hips, thighs, buttocks, pubis, upper arms, and breasts. (Fat on the hips, thighs, and buttocks has a higher concentration of omega-3 fatty acids and is meant to be used for lactation.) The body begins to burn old adipose tissue in the waist, shoulders, and back, making those areas smaller.[203]
Subcutaneous fat increases in the cheeks and lips, making the face appear rounder, with slightly less emphasis on the jaw as the lower portion of the cheeks fills in.
Muscle changes
HRT causes a reduction in muscle mass and distribution towards female proportions.
Bone/skeletal changes
Male-to-female hormone therapy causes the hips to rotate slightly forward because of changes in the tendons. Hip discomfort is not uncommon. This can cause a reduction in total body height.
If estrogen therapy is begun prior to pelvis ossification, which occurs around the age of 25, the pelvic outlet and inlet open slightly. The femora also widen, because they are connected to the pelvis. The pelvis retains some masculine characteristics, but the end result of HRT is wider hips than a cisgender man and closer to those of a cisgender woman.
Unaffected characteristics
HRT does not reverse bone changes that have already been established by puberty. Consequently, it does not affect height; the length of the arms, legs, hands, and feet; or the width of the shoulders and rib cage. However, details of bone shape change throughout life, with bones becoming heavier and more deeply sculptured under the influence of androgens, and HRT does prevent such changes from progressing further.
The width of the hips is not affected in individuals for whom epiphyseal closure (fusion and closure of the ends of bones, which prevents any further lengthening) has taken place. This occurs in most people between 18 and 25 years of age. Already-established changes to the shape of the hips cannot be reversed by HRT whether epiphyseal closure has taken place or not.
Established changes to the bone structure of the face are also unaffected by HRT. A significant majority of craniofacial changes occur during adolescence. Post-adolescent growth is considerably slower and minimal by comparison.[217] Also unaffected is the prominence of the thyroid cartilage (Adam's apple). These changes may be reversed by surgery (facial feminization surgery and tracheal shave, respectively).
During puberty, the voice deepens in pitch and becomes more resonant. These changes are permanent and are not affected by HRT. Voice therapy and/or surgery may be used instead to achieve a more female-sounding voice.
Facial hair develops during puberty and is only slightly affected by HRT. It may, however, be eliminated nearly permanently with laser hair removal, or permanently with electrolysis.
Psychological changes
The psychological effects of feminizing hormone therapy are harder to define than physical changes. Because hormone therapy is usually the first physical step taken to transition, the act of beginning it has a significant psychological effect, which is difficult to distinguish from hormonally induced changes.
Mood changes
Mood changes, including depression, may occur with feminizing hormone therapy. However, many transgender women report mood benefits as well.
Sexual changes
Some transgender women report a significant reduction in libido, depending on the dosage of antiandrogens. A small number of post-operative transgender women take low doses of testosterone to boost their libido. Many pre-operative transgender women wait until after reassignment surgery to begin an active sex life. Raising the dosage of estrogen or adding a progestogen raises the libido of some transgender women.
Spontaneous and morning erections decrease significantly in frequency, although some patients who have had an orchiectomy still experience morning erections. Voluntary erections may or may not be possible, depending on the amount of hormones and/or antiandrogens being taken.
Managing long-term hormonal regimens have not been studied and are difficult to estimate because research on the long-term use of hormonal therapy has not been noted.[20] However, it is possible to speculate the outcomes of these therapies on transgender people based on the knowledge of the current effects of gonadal hormones on sexual functioning in cisgender men and women.[218]
Firstly, if one is to decrease testosterone in male-to-female gender transition, it is likely that sexual desire and arousal would be inhibited; alternatively, if high doses of estrogen negatively impact sexual desire, which has been found in some research with cisgender women, it is hypothesized that combining androgens with high levels of estrogen would intensify this outcome.[218] Unfortunately, to date there haven’t been any randomized clinical trials looking at the relationship between type and dose of transgender hormone therapy, so the relationship between them remains unclear.[218] Typically, the estrogens given for male-to-female gender transition are 2 to 3 times higher than the recommended dose for HRT in postmenopausal women.[20] Pharmacokinetic studies indicate taking these increased doses may lead to a higher boost in plasma estradiol levels; however, the long-term side effects haven’t been studied and the safety of this route is unclear.[20]
As with any pharmacological or hormone therapy, there are potential side effects, which in the case of transgender hormone therapy include changes in sexual functioning. These have the ability to significantly impact sexual functioning, either directly or indirectly through the various side effects, such as cerebrovascular disorders, obesity, and mood fluctuations.[218] In addition, some research has found an onset of diabetes following feminizing hormone therapy, which impairs sexual response. Whatever route an individual and their doctor choose to take, it is important to consider both the medical risks of hormone therapy as well as the psychological needs of the patient.
Neurological changes
Recent studies have indicated that hormone therapy in transgender women may reduce brain volume toward female proportions.[219]
All aforementioned physical changes can, and reportedly do, change the experience of sensation compared to prior to HRT. Areas affected include, but aren't limited to, the basic senses, erogenous stimulus, perception of emotion, perception of social interaction, and processing of feelings and experiences.
Health-related changes
Cardiovascular effects
The most significant cardiovascular risk for transgender women is the pro-thrombotic effect (increased blood clotting) of estrogens. This manifests most significantly as an increased risk for thromboembolic disease: deep vein thrombosis (DVT) and pulmonary embolism, which occurs when blood clots from DVT break off and migrate to the lungs. Symptoms of DVT include pain or swelling of one leg, especially the calf. Symptoms of pulmonary embolism include chest pain, shortness of breath, fainting, and heart palpitations, sometimes without leg pain or swelling.
Deep vein thrombosis occurs more frequently in the first year of treatment with estrogens. The risk is higher with oral estrogens (particularly ethinylestradiol and conjugated estrogens) than with injectable, transdermal, implantable, and nasal formulations.[220] DVT risk also increases with age and in patients who smoke, so many clinicians advise using the safer estrogen formulations in smokers and patients older than 40.
Because the risks of warfarin – which is used to treat blood clots – in a relatively young and otherwise healthy population are low, while the risk of adverse physical and psychological outcomes for untreated transgender patients is high, pro-thrombotic mutations (such as factor V Leiden, antithrombin III, and protein C or S deficiency) are not absolute contraindications for hormonal therapy.[221]
Gastrointestinal/metabolic changes
Estrogens may increase the risk of gallbladder disease, especially in older and obese people.[222] They may also increase transaminase levels, indicating liver toxicity, especially when taken in oral form.
A patient's metabolic rate may change, causing an increase or decrease in weight and energy levels, changes to sleep patterns, and temperature sensitivity. Androgen deprivation leads to slower metabolism and a loss of muscle tone. Building muscle takes more work. The addition of a progestogen may increase energy, although it may increase appetite as well.
Bone changes
Both estrogens and androgens are necessary in all humans for bone health. Young, healthy women produce about 10 mg of testosterone monthly, and higher bone mineral density in males is associated with higher serum estrogen. Both estrogen and testosterone help to stimulate bone formation, especially during puberty. Estrogen is the predominant sex hormone that slows bone loss, even in men.
Risk of hormone-sensitive cancers
In spite of the induction of breast development, transgender women who undergo HRT do not have an increased risk of breast cancer.[1][223][224] Only a handful of cases of breast cancer have ever been described in transgender women who have undergone male-to-female HRT.[223][224] This is in accordance with research in cisgender men in which gynecomastia has been found not to be associated with an increased risk of breast cancer, suggesting a protective role of the male sex-determination chromosome.[225] On the other hand, men with Klinefelter's syndrome (two X chromosomes and one Y chromosome), which causes hypoandrogenism, hyperestrogenism, and a very high incidence of gynecomastia (80%), have a dramatically (20- to 58-fold) increased risk of breast cancer compared to men with one X chromosome, closer to the rate of homogametic females.[225][226][227] The incidences of breast cancer in karyotypical men (46,XY karyotype), men with Klinefelter's syndrome (47,XXY karyotype), and karyotypical women (46,XX karyotype) are approximately 0.1%,[228] 3%,[226] and 12.5%,[229] respectively. Individuals with the 46,XY karyotype affected by complete androgen insensitivity syndrome never develop male sex characteristics and have normal and complete female morphology, and accelerated breast growth during puberty,[230][231] but appear to have little (or possibly even no) incidence of breast cancer.[232][233] The risk of breast cancer in women with Turner syndrome (45,XO karyotype) also appears to be significantly decreased, though this may be related to ovarian failure/hypogonadism rather necessarily than to genetics.[234]
Prostate cancer is extremely rare in orchidectomized transgender women who have been treated with estrogens for a prolonged period of time.[1][235][236] Whereas as many as 70% of men show prostate cancer by their 80's,[237] only a handful of cases of prostate cancer in transgender women have been reported in the literature.[1][235][236] As such, and in accordance with the fact that androgens are responsible for the development of prostate cancer, HRT appears to be highly protective against prostate cancer in transgender women.[1][235][236]
Other changes
Migraines can be made worse or unmasked by estrogen therapy.
Estrogens can also cause prolactinomas. Milk discharge from the nipples can be a sign of elevated prolactin levels. If a prolactinoma becomes large enough, it can cause visual changes (especially decreased peripheral vision), headaches, depression or other mood changes, dizziness, nausea, vomiting, and symptoms of pituitary failure, like hypothyroidism.
Hormone levels
Especially in the early stages of hormone replacement therapy, blood work is done frequently to assess hormone levels and liver function. The Endocrine Society recommends that patients have blood tests every three months in the first year of HRT for estradiol and testosterone, and that spironolactone, if used, be monitored every 2 to 3 months in the first year.[1] The optimal ranges for estradiol and testosterone are not limited to but include the following:
| Hormone | Endocrine Society[1] | Royal College of Psychiatry[9] |
|---|---|---|
| Estradiol | 100–200 pg/mL | 80–140 pg/mL |
| Testosterone | <50 ng/dL | "Well below normal male range" |
The optimal ranges for estrogen apply only to individuals taking estradiol (or an ester of estradiol), and not to those taking synthetic or other non-bioidentical preparations (e.g., CEEs or ethinylestradiol).[1]
Physicians also recommend broader medical monitoring, including complete blood counts; tests of renal function, liver function, and lipid and glucose metabolism; and monitoring of prolactin levels, body weight, and blood pressure.[1]
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 Hembree WC, Cohen-Kettenis PT, Gooren L, Hannema SE, Meyer WJ, Murad MH, Rosenthal SM, Safer JD, Tangpricha V, T'Sjoen GG (November 2017). "Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline" (PDF). J. Clin. Endocrinol. Metab. 102 (11): 3869–3903. doi:10.1210/jc.2017-01658. PMID 28945902.
- 1 2 3 4 5 6 7 8 9 10 11 12 Coleman, E.; Bockting, W.; Botzer, M.; Cohen-Kettenis, P.; DeCuypere, G.; Feldman, J.; Fraser, L.; Green, J.; Knudson, G.; Meyer, W. J.; Monstrey, S.; Adler, R. K.; Brown, G. R.; Devor, A. H.; Ehrbar, R.; Ettner, R.; Eyler, E.; Garofalo, R.; Karasic, D. H.; Lev, A. I.; Mayer, G.; Meyer-Bahlburg, H.; Hall, B. P.; Pfaefflin, F.; Rachlin, K.; Robinson, B.; Schechter, L. S.; Tangpricha, V.; van Trotsenburg, M.; Vitale, A.; Winter, S.; Whittle, S.; Wylie, K. R.; Zucker, K. (2012). "Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, Version 7" (PDF). International Journal of Transgenderism. 13 (4): 165–232. doi:10.1080/15532739.2011.700873. ISSN 1553-2739.
- 1 2 3 4 5 6 7 8 Deutsch M (17 June 2016). "Guidelines for the Primary and Gender-Affirming Care of Transgender and Gender Nonbinary People" (pdf) (2nd ed.). University of California, San Francisco: Center of Excellence for Transgender Health. p. 28.
- 1 2 3 4 5 6 7 8 9 10 Wesp LM, Deutsch MB (March 2017). "Hormonal and Surgical Treatment Options for Transgender Women and Transfeminine Spectrum Persons". Psychiatr. Clin. North Am. 40 (1): 99–111. doi:10.1016/j.psc.2016.10.006. PMID 28159148.
- 1 2 3 4 5 6 7 8 9 10 Dahl, M; Feldman, JL; Goldberg, J; Jaberi, A (2015). "Endocrine Therapy for Transgender Adults in British Columbia: Suggested Guidelines" (PDF). Vancouver Coastal Health. Retrieved 15 August 2018.
- 1 2 3 4 5 Bourns, Amy (2015). "Guidelines and Protocols for Comprehensive Primary Care for Trans Clients" (PDF). Sherbourne Health Centre. Retrieved 15 August 2018.
- ↑ "Weinand J, Safer J. Feb 2015. "Hormone therapy in transgender adults is safe with provider supervision; A review of hormone therapy sequelae for transgender individuals." Journal of Clinical & Translational Endocrinology (2015)".
- ↑ "Orilissa (elagolix) FDA Label" (PDF). 24 July 2018. Retrieved 31 July 2018.
- 1 2 Wylie, Kevan; Barrett, James; Besser, Mike; Bouman, Walter Pierre; Bridgman, Michelle; Clayton, Angela; Green, Richard; Hamilton, Mark; Hines, Melissa; Ivbijaro, Gabriel; Khoosal, Deenesh; Lawrence, Alex; Lenihan, Penny; Loewenthal, Del; Ralph, David; Reed, Terry; Stevens, John; Terry, Tim; Thom, Ben; Thornton, Jane; Walsh, Dominic; Ward, David; Coleman, Eli; Di Ceglie, Domenico; Martin, Emma; McGarry, Philip; Messenger, Andrew; Reid, Russell; Sethi, Su; Sutcliffe, Paul; Wilson, Daniel; Carr, Susan; Davies, Dai; Dean, Tracey; Ellis, Michelle; Ferguson, Brian; Skinner, Darren; Williams, Vicky; Brechin, Susan; Lucey, Jim; Rathbone, Maxine (2014). "Good Practice Guidelines for the Assessment and Treatment of Adults with Gender Dysphoria" (PDF). Sexual and Relationship Therapy. 29 (2): 154–214. doi:10.1080/14681994.2014.883353. ISSN 1468-1994.
- 1 2 3 4 5 6 7 8 9 Unger CA (December 2016). "Hormone therapy for transgender patients". Transl Androl Urol. 5 (6): 877–884. doi:10.21037/tau.2016.09.04. PMC 5182227. PMID 28078219.
- 1 2 Gooren LJ (March 2011). "Clinical practice. Care of transsexual persons". N. Engl. J. Med. 364 (13): 1251–7. doi:10.1056/NEJMcp1008161. PMID 21449788.
- ↑ James Barrett (29 September 2017). Transsexual and Other Disorders of Gender Identity: A Practical Guide to Management. CRC Press. pp. 216–. ISBN 978-1-315-34513-0.
- ↑ Carlo Trombetta; Giovanni Liguori; Michele Bertolotto (3 March 2015). Management of Gender Dysphoria: A Multidisciplinary Approach. Springer. pp. 85–. ISBN 978-88-470-5696-1.
- 1 2 3 4 5 6 7 8 Fabris B, Bernardi S, Trombetta C (March 2015). "Cross-sex hormone therapy for gender dysphoria". J. Endocrinol. Invest. 38 (3): 269–82. doi:10.1007/s40618-014-0186-2. PMID 25403429.
- ↑ Kristen Eckstrand; Jesse M. Ehrenfeld (17 February 2016). Lesbian, Gay, Bisexual, and Transgender Healthcare: A Clinical Guide to Preventive, Primary, and Specialist Care. Springer. pp. 357–. ISBN 978-3-319-19752-4.
- 1 2 3 4 5 6 7 8 Tangpricha V, den Heijer M (April 2017). "Oestrogen and anti-androgen therapy for transgender women". Lancet Diabetes Endocrinol. 5 (4): 291–300. doi:10.1016/S2213-8587(16)30319-9. PMC 5366074. PMID 27916515.
- 1 2 Gooren LJ, Giltay EJ, Bunck MC (January 2008). "Long-term treatment of transsexuals with cross-sex hormones: extensive personal experience". J. Clin. Endocrinol. Metab. 93 (1): 19–25. doi:10.1210/jc.2007-1809. PMID 17986639.
- 1 2 3 4 5 6 Meriggiola MC, Gava G (November 2015). "Endocrine care of transpeople part II. A review of cross-sex hormonal treatments, outcomes and adverse effects in transwomen". Clin. Endocrinol. (Oxf). 83 (5): 607–15. doi:10.1111/cen.12754. PMID 25692882.
- ↑ Costa EM, Mendonca BB (March 2014). "Clinical management of transsexual subjects". Arq Bras Endocrinol Metabol. 58 (2): 188–96. doi:10.1590/0004-2730000003091. PMID 24830596.
- 1 2 3 4 5 6 7 8 9 Moore E, Wisniewski A, Dobs A (August 2003). "Endocrine treatment of transsexual people: a review of treatment regimens, outcomes, and adverse effects". The Journal of Clinical Endocrinology and Metabolism. 88 (8): 3467–73. doi:10.1210/jc.2002-021967. PMID 12915619.
- ↑ Rosenthal SM (December 2014). "Approach to the patient: transgender youth: endocrine considerations". J. Clin. Endocrinol. Metab. 99 (12): 4379–89. doi:10.1210/jc.2014-1919. PMID 25140398.
- ↑ Bourgeois AL, Auriche P, Palmaro A, Montastruc JL, Bagheri H (February 2016). "Risk of hormonotherapy in transgender people: Literature review and data from the French Database of Pharmacovigilance". Ann. Endocrinol. (Paris). 77 (1): 14–21. doi:10.1016/j.ando.2015.12.001. PMID 26830952.
- 1 2 Asscheman, Henk; Gooren, Louis J.G. (1993). "Hormone Treatment in Transsexuals". Journal of Psychology & Human Sexuality. 5 (4): 39–54. doi:10.1300/J056v05n04_03. ISSN 0890-7064.
- 1 2 Levy A, Crown A, Reid R (October 2003). "Endocrine intervention for transsexuals". Clin. Endocrinol. (Oxf). 59 (4): 409–18. doi:10.1046/j.1365-2265.2003.01821.x. PMID 14510900.
- ↑ Vincenzo Mirone (12 February 2015). Clinical Uro-Andrology. Springer. pp. 17–. ISBN 978-3-662-45018-5.
- ↑ Gianna E. Israel (March 2001). Transgender Care: Recommended Guidelines, Practical Information, and Personal Accounts. Temple University Press. pp. 56–. ISBN 978-1-56639-852-7.
- ↑ Stege R, Gunnarsson PO, Johansson CJ, Olsson P, Pousette A, Carlström K (1996). "Pharmacokinetics and testosterone suppression of a single dose of polyestradiol phosphate (Estradurin) in prostatic cancer patients". Prostate. 28 (5): 307–10. doi:10.1002/(SICI)1097-0045(199605)28:5<307::AID-PROS6>3.0.CO;2-8. PMID 8610057.
- 1 2 3 4 5 6 7 8 Leinung MC, Feustel PJ, Joseph J (2018). "Hormonal Treatment of Transgender Women with Oral Estradiol". Transgend Health. 3 (1): 74–81. doi:10.1089/trgh.2017.0035. PMC 5944393. PMID 29756046.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Kuhl H (2005). "Pharmacology of estrogens and progestogens: influence of different routes of administration" (PDF). Climacteric. 8 Suppl 1: 3–63. doi:10.1080/13697130500148875. PMID 16112947.
- ↑ Alfred S. Wolf; H.P.G. Schneider (12 March 2013). Östrogene in Diagnostik und Therapie. Springer-Verlag. pp. 79, 81. ISBN 978-3-642-75101-1.
- 1 2 Lauritzen C (September 1990). "Clinical use of oestrogens and progestogens". Maturitas. 12 (3): 199–214. doi:10.1016/0378-5122(90)90004-P. PMID 2215269.
- ↑ Lauritzen C (December 1986). "Die Behandlung der klimakterischen Beschwerden durch vaginale, rektale und transdermale Ostrogensubstitution" [Treatment of disorders of the climacteric by vaginal, rectal and transdermal estrogen substitution]. Gynakologe (in German). 19 (4): 248–53. ISSN 0017-5994. PMID 3817597.
- ↑ Irwig MS (August 2018). "Cardiovascular health in transgender people". Rev Endocr Metab Disord. doi:10.1007/s11154-018-9454-3. PMID 30073551.
- ↑ Getahun D, Nash R, Flanders WD, Baird TC, Becerra-Culqui TA, Cromwell L, Hunkeler E, Lash TL, Millman A, Quinn VP, Robinson B, Roblin D, Silverberg MJ, Safer J, Slovis J, Tangpricha V, Goodman M (July 2018). "Cross-sex Hormones and Acute Cardiovascular Events in Transgender Persons: A Cohort Study". Ann. Intern. Med. doi:10.7326/M17-2785. PMID 29987313.
- ↑ Ockrim J, Lalani EN, Abel P (October 2006). "Therapy Insight: parenteral estrogen treatment for prostate cancer—a new dawn for an old therapy". Nat Clin Pract Oncol. 3 (10): 552–63. doi:10.1038/ncponc0602. PMID 17019433.
- ↑ Lycette JL, Bland LB, Garzotto M, Beer TM (December 2006). "Parenteral estrogens for prostate cancer: can a new route of administration overcome old toxicities?". Clin Genitourin Cancer. 5 (3): 198–205. doi:10.3816/CGC.2006.n.037. PMID 17239273.
- ↑ Stege R, Carlström K, Collste L, Eriksson A, Henriksson P, Pousette A (1988). "Single drug polyestradiol phosphate therapy in prostatic cancer". Am. J. Clin. Oncol. 11 Suppl 2: S101–3. doi:10.1097/00000421-198801102-00024. PMID 3242384.
- ↑ Ockrim JL, Lalani EN, Laniado ME, Carter SS, Abel PD (May 2003). "Transdermal estradiol therapy for advanced prostate cancer--forward to the past?". J. Urol. 169 (5): 1735–7. doi:10.1097/01.ju.0000061024.75334.40. PMID 12686820.
- ↑ Leinung, MC (June 2014). "Variable Response to Oral Estradiol Therapy in Male to Female Transgender Patients". Endocrine Reviews. 35 (3). doi:10.1210/endo-meetings.2014.RE.2.OR42-1 (inactive 2018-08-19).
- ↑ Liang JJ, Jolly D, Chan KJ, Safer JD (February 2018). "Testosterone Levels Achieved by Medically Treated Transgender Women in a United States Endocrinology Clinic Cohort". Endocr Pract. 24 (2): 135–142. doi:10.4158/EP-2017-0116. PMID 29144822.
- 1 2 Wylie, Kevan Richard; Fung, Robert; Boshier, Claudia; Rotchell, Margaret (2009). "Recommendations of endocrine treatment for patients with gender dysphoria". Sexual and Relationship Therapy. 24 (2): 175–187. doi:10.1080/14681990903023306. ISSN 1468-1994.
- ↑ Carlo Trombetta; Giovanni Liguori; Michele Bertolotto (3 March 2015). Management of Gender Dysphoria: A Multidisciplinary Approach. Springer. pp. 85–. ISBN 978-88-470-5696-1.
- ↑ Rauramo L, Punnonen R, Kaihola LH, Grönroos M (January 1980). "Serum oestrone, oestradiol and oestriol concentrations in castrated women during intramuscular oestradiol valerate and oestradiolbenzoate-oestradiolphenylpropionate therapy". Maturitas. 2 (1): 53–8. doi:10.1016/0378-5122(80)90060-2. PMID 7402086.
- ↑ Garza-Flores J (April 1994). "Pharmacokinetics of once-a-month injectable contraceptives". Contraception. 49 (4): 347–59. doi:10.1016/0010-7824(94)90032-9. PMID 8013219.
- 1 2 3 4 5 6 7 8 9 Gava, Giulia; Seracchioli, Renato; Meriggiola, Maria Cristina (2017). "Therapy with Antiandrogens in Gender Dysphoric Natal Males". Endocrinology of the Testis and Male Reproduction. Endocrinology. pp. 1199–1209. doi:10.1007/978-3-319-44441-3_42. ISBN 978-3-319-44440-6. ISSN 2510-1927.
- 1 2 Lieberman R (2001). "Androgen deprivation therapy for prostate cancer chemoprevention: current status and future directions for agent development". Urology. 58 (2 Suppl 1): 83–90. doi:10.1016/s0090-4295(01)01247-x. PMID 11502457.
There are several classes of antiandrogens including (1) antigonadotropins (eg, LHRH agonists/antagonists, synthetic estrogens [diethylstilbestrol]); (2) nonsteroidal androgen-receptor antagonists (eg, flutamide, bicalutamide, nilutamide); (3) steroidal agents with mixed actions (eg, cyproterone acetate); (4) adrenal androgen inhibitors (eg, ketoconazole, hydrocortisone); (5) steroidal agents that inhibit androgen biosynthesis (eg, 5α-reductase inhibitors (type II) and dual-acting 5α-reductase inhibitors); [...]
- ↑ Brueggemeier, Robert W. (2006). "Sex Hormones (Male): Analogs and Antagonists". Encyclopedia of Molecular Cell Biology and Molecular Medicine. doi:10.1002/3527600906.mcb.200500066. ISBN 978-3527600908.
- ↑ de Lignières B, Silberstein S (April 2000). "Pharmacodynamics of oestrogens and progestogens". Cephalalgia. 20 (3): 200–7. doi:10.1046/j.1468-2982.2000.00042.x. PMID 10997774.
- ↑ Neumann F (1978). "The physiological action of progesterone and the pharmacological effects of progestogens--a short review". Postgraduate Medical Journal. 54 Suppl 2: 11–24. PMID 368741.
- 1 2 3 Singh SM, Gauthier S, Labrie F (2000). "Androgen receptor antagonists (antiandrogens): structure-activity relationships". Curr. Med. Chem. 7 (2): 211–47. doi:10.2174/0929867003375371. PMID 10637363.
- 1 2 Loren S Schechter (22 September 2016). Surgical Management of the Transgender Patient. Elsevier Health Sciences. pp. 26–. ISBN 978-0-323-48408-4.
- ↑ Lynne Carroll; Lauren Mizock (7 February 2017). Clinical Issues and Affirmative Treatment with Transgender Clients, An Issue of Psychiatric Clinics of North America, E-Book. Elsevier Health Sciences. pp. 107–. ISBN 978-0-323-51004-2.
- ↑ Laura Erickson-Schroth (12 May 2014). Trans Bodies, Trans Selves: A Resource for the Transgender Community. Oxford University Press. pp. 258–. ISBN 978-0-19-932536-8.
- 1 2 3 4 J. Larry Jameson; Leslie J. De Groot (18 May 2010). Endocrinology - E-Book: Adult and Pediatric. Elsevier Health Sciences. pp. 2282–. ISBN 978-1-4557-1126-0.
- 1 2 3 4 5 6 Randi Ettner; Stan Monstrey; Eli Coleman (20 May 2016). Principles of Transgender Medicine and Surgery. Routledge. pp. 169–170, 216. ISBN 978-1-317-51460-2.
- 1 2 Kolkhof P, Bärfacker L (July 2017). "30 YEARS OF THE MINERALOCORTICOID RECEPTOR: Mineralocorticoid receptor antagonists: 60 years of research and development". J. Endocrinol. 234 (1): T125–T140. doi:10.1530/JOE-16-0600. PMC 5488394. PMID 28634268.
- 1 2 3 4 McMullen GR, Van Herle AJ (December 1993). "Hirsutism and the effectiveness of spironolactone in its management". J. Endocrinol. Invest. 16 (11): 925–32. doi:10.1007/BF03348960. PMID 8144871.
- 1 2 3 Loriaux, D. Lynn (November 1976). "Spironolactone and endocrine dysfunction". Annals of Internal Medicine. 85 (5): 630–6. doi:10.7326/0003-4819-85-5-630. PMID 984618.
- 1 2 3 Thompson DF, Carter JR (1993). "Drug-induced gynecomastia". Pharmacotherapy. 13 (1): 37–45. doi:10.1002/j.1875-9114.1993.tb02688.x (inactive 2018-08-19). PMID 8094898.
- 1 2 3 Shaw JC (February 1991). "Spironolactone in dermatologic therapy". J. Am. Acad. Dermatol. 24 (2 Pt 1): 236–43. doi:10.1016/0190-9622(91)70034-Y. PMID 1826112.
- 1 2 3 4 5 Layton AM, Eady EA, Whitehouse H, Del Rosso JQ, Fedorowicz Z, van Zuuren EJ (2017). "Oral Spironolactone for Acne Vulgaris in Adult Females: A Hybrid Systematic Review". Am J Clin Dermatol. 18 (2): 169–191. doi:10.1007/s40257-016-0245-x. PMC 5360829. PMID 28155090.
- ↑ Doggrell SA, Brown L (May 2001). "The spironolactone renaissance". Expert Opin Investig Drugs. 10 (5): 943–54. doi:10.1517/13543784.10.5.943. PMID 11322868.
- ↑ Jashin J. Wu (18 October 2012). Comprehensive Dermatologic Drug Therapy E-Book. Elsevier Health Sciences. pp. 364–. ISBN 978-1-4557-3801-4.
Spironolactone is an aldosterone antagonist and a relatively weak antiandrogen that blocks the AR and inhibits androgen biosynthesis.
- ↑ H.J.T. Coelingh Benni; H.M. Vemer (15 December 1990). Chronic Hyperandrogenic Anovulation. CRC Press. pp. 152–. ISBN 978-1-85070-322-8.
- 1 2 Pavone-Macaluso M, de Voogt HJ, Viggiano G, Barasolo E, Lardennois B, de Pauw M, Sylvester R (September 1986). "Comparison of diethylstilbestrol, cyproterone acetate and medroxyprogesterone acetate in the treatment of advanced prostatic cancer: final analysis of a randomized phase III trial of the European Organization for Research on Treatment of Cancer Urological Group". J. Urol. 136 (3): 624–31. doi:10.1016/S0022-5347(17)44996-2. PMID 2942707.
- 1 2 Jeffrey K. Aronson (2 March 2009). Meyler's Side Effects of Cardiovascular Drugs. Elsevier. pp. 253–258. ISBN 978-0-08-093289-7.
- 1 2 Lainscak M, Pelliccia F, Rosano G, Vitale C, Schiariti M, Greco C, Speziale G, Gaudio C (2015). "Safety profile of mineralocorticoid receptor antagonists: Spironolactone and eplerenone". Int. J. Cardiol. 200: 25–9. doi:10.1016/j.ijcard.2015.05.127. PMID 26404748.
- ↑ Juurlink DN, Mamdani MM, Lee DS, Kopp A, Austin PC, Laupacis A, Redelmeier DA (2004). "Rates of hyperkalemia after publication of the Randomized Aldactone Evaluation Study". N. Engl. J. Med. 351 (6): 543–51. doi:10.1056/NEJMoa040135. PMID 15295047.
- 1 2 Zaenglein AL, Pathy AL, Schlosser BJ, Alikhan A, Baldwin HE, Berson DS, Bowe WP, Graber EM, Harper JC, Kang S, Keri JE, Leyden JJ, Reynolds RV, Silverberg NB, Stein Gold LF, Tollefson MM, Weiss JS, Dolan NC, Sagan AA, Stern M, Boyer KM, Bhushan R (2016). "Guidelines of care for the management of acne vulgaris". J. Am. Acad. Dermatol. 74 (5): 945–73.e33. doi:10.1016/j.jaad.2015.12.037. PMID 26897386.
- 1 2 Plovanich M, Weng QY, Mostaghimi A (2015). "Low Usefulness of Potassium Monitoring Among Healthy Young Women Taking Spironolactone for Acne". JAMA Dermatol. 151 (9): 941–4. doi:10.1001/jamadermatol.2015.34. PMID 25796182.
- ↑ Fourcade, R.-O.; McLeod, D. (2015). "Tolerability of Antiandrogens in the Treatment of Prostate Cancer". UroOncology. 4 (1): 5–13. doi:10.1080/1561095042000191655. ISSN 1561-0950.
- 1 2 3 Jacobi GH, Altwein JE, Kurth KH, Basting R, Hohenfellner R (1980). "Treatment of advanced prostatic cancer with parenteral cyproterone acetate: a phase III randomised trial". Br J Urol. 52 (3): 208–15. doi:10.1111/j.1464-410x.1980.tb02961.x. PMID 7000222.
- 1 2 3 Neumann F (1994). "The antiandrogen cyproterone acetate: discovery, chemistry, basic pharmacology, clinical use and tool in basic research". Exp. Clin. Endocrinol. 102 (1): 1–32. doi:10.1055/s-0029-1211261. PMID 8005205.
- ↑ Raudrant D, Rabe T (2003). "Progestogens with antiandrogenic properties". Drugs. 63 (5): 463–92. doi:10.2165/00003495-200363050-00003. PMID 12600226.
- ↑ Koch UJ, Lorenz F, Danehl K, Ericsson R, Hasan SH, Keyserlingk DV, Lübke K, Mehring M, Römmler A, Schwartz U, Hammerstein J (1976). "Continuous oral low-dosage cyproterone acetate for fertility regulation in the male? A trend analysis in 15 volunteers". Contraception. 14 (2): 117–35. doi:10.1016/0010-7824(76)90081-0. PMID 949890.
- ↑ Moltz, L.; Römmler, A.; Schwartz, U.; Hammerstein, J. (1978). "Effects of Cyproterone Acetate (CPA) on Pituitary Gonadotrophin Release and on Androgen Secretion Before and After LH-RH Double Stimulation Tests in Men". International Journal of Andrology. 1 (s2b): 713–719. doi:10.1111/j.1365-2605.1978.tb00518.x. ISSN 0105-6263.
- ↑ Wang C, Yeung KK (1980). "Use of low-dosage oral cyproterone acetate as a male contraceptive". Contraception. 21 (3): 245–72. doi:10.1016/0010-7824(80)90005-0. PMID 6771091.
- ↑ Moltz L, Römmler A, Post K, Schwartz U, Hammerstein J (April 1980). "Medium dose cyproterone acetate (CPA): effects on hormone secretion and on spermatogenesis in men". Contraception. 21 (4): 393–413. doi:10.1016/s0010-7824(80)80017-5. PMID 6771095.
- ↑ Knuth UA, Hano R, Nieschlag E (1984). "Effect of flutamide or cyproterone acetate on pituitary and testicular hormones in normal men". J. Clin. Endocrinol. Metab. 59 (5): 963–9. doi:10.1210/jcem-59-5-963. PMID 6237116.
- ↑ Fung, Raymond; Hellstern-Layefsky, Miriam; Lega, Iliana (2017). "Is a lower dose of cyproterone acetate as effective at testosterone suppression in transgender women as higher doses?". International Journal of Transgenderism. 18 (2): 123–128. doi:10.1080/15532739.2017.1290566. ISSN 1553-2739.
- ↑ Pucci E, Petraglia F (December 1997). "Treatment of androgen excess in females: yesterday, today and tomorrow". Gynecol. Endocrinol. 11 (6): 411–33. doi:10.3109/09513599709152569. PMID 9476091.
- ↑ Pharmacology of the Skin II: Methods, Absorption, Metabolism and Toxicity, Drugs and Diseases. Springer Science & Business Media. 6 December 2012. pp. 474, 489. ISBN 978-3-642-74054-1.
- ↑ Thole Z, Manso G, Salgueiro E, Revuelta P, Hidalgo A (2004). "Hepatotoxicity induced by antiandrogens: a review of the literature". Urol. Int. 73 (4): 289–95. doi:10.1159/000081585. PMID 15604569.
- ↑ Migliari R, Muscas G, Murru M, Verdacchi T, De Benedetto G, De Angelis M (1999). "Antiandrogens: a summary review of pharmacodynamic properties and tolerability in prostate cancer therapy". Archivio Italiano di Urologia e Andrologia. 71 (5): 293–302. PMID 10673793.
The only advantage of cyproterone acetate on pure antiandrogens seems to be the low incidence of hot flushes; [...] However, hepatotoxicity associated with long term daily doses of 300 mg daily and the unacceptably high incidence of cardiovascular side effects (10%) should restrict its use to patients who are intolerant of pure antiandrogen compound. In contrast to steroidal compound nonsteroidal compounds let sexual potency to be retained, [...]
- ↑ Lothstein, Leslie M. (1996). "Antiandrogen treatment for sexual disorders: Guidelines for establishing a standard of care". Sexual Addiction & Compulsivity. 3 (4): 313–331. doi:10.1080/10720169608400122. ISSN 1072-0162.
- ↑ Dangerous Sex Offenders: A Task Force Report of the American Psychiatric Association. American Psychiatric Pub. 1999. pp. 112–144. ISBN 978-0-89042-280-9.
- ↑ Kravitz HM, Haywood TW, Kelly J, Liles S, Cavanaugh JL (1996). "Medroxyprogesterone and paraphiles: do testosterone levels matter?". Bull Am Acad Psychiatry Law. 24 (1): 73–83. PMID 8891323.
- ↑ Novak E, Hendrix JW, Chen TT, Seckman CE, Royer GL, Pochi PE (October 1980). "Sebum production and plasma testosterone levels in man after high-dose medroxyprogesterone acetate treatment and androgen administration". Acta Endocrinol. 95 (2): 265–70. doi:10.1530/acta.0.0950265. PMID 6449127.
- ↑ Kirschner MA, Schneider G (February 1972). "Suppression of the pituitary-Leydig cell axis and sebum production in normal men by medroxyprogesterone acetate (provera)". Acta Endocrinol. 69 (2): 385–93. doi:10.1530/acta.0.0690385. PMID 5066846.
- 1 2 Kemppainen JA, Langley E, Wong CI, Bobseine K, Kelce WR, Wilson EM (March 1999). "Distinguishing androgen receptor agonists and antagonists: distinct mechanisms of activation by medroxyprogesterone acetate and dihydrotestosterone". Mol. Endocrinol. 13 (3): 440–54. doi:10.1210/mend.13.3.0255. PMID 10077001.
- ↑ Worly BL, Gur TL, Schaffir J (February 2018). "The relationship between progestin hormonal contraception and depression: a systematic review". Contraception. 97 (6): 478–489. doi:10.1016/j.contraception.2018.01.010. PMID 29496297.
- ↑ Westhoff C (August 2003). "Depot-medroxyprogesterone acetate injection (Depo-Provera): a highly effective contraceptive option with proven long-term safety". Contraception. 68 (2): 75–87. doi:10.1016/S0010-7824(03)00136-7. PMID 12954518.
- ↑ Nieschlag E (November 2010). "Clinical trials in male hormonal contraception". Contraception. 82 (5): 457–70. doi:10.1016/j.contraception.2010.03.020. PMID 20933120.
- ↑ Nieschlag E, Zitzmann M, Kamischke A (November 2003). "Use of progestins in male contraception". Steroids. 68 (10–13): 965–72. doi:10.1016/S0039-128X(03)00135-1. PMID 14667989.
- ↑ Wu FC, Balasubramanian R, Mulders TM, Coelingh-Bennink HJ (January 1999). "Oral progestogen combined with testosterone as a potential male contraceptive: additive effects between desogestrel and testosterone enanthate in suppression of spermatogenesis, pituitary-testicular axis, and lipid metabolism". J. Clin. Endocrinol. Metab. 84 (1): 112–22. doi:10.1210/jcem.84.1.5412. PMID 9920070.
- ↑ Kumamoto Y, Yamaguchi Y, Sato Y, Suzuki R, Tanda H, Kato S, Mori K, Matsumoto H, Maki A, Kadono M (February 1990). "[Effects of anti-androgens on sexual function. Double-blind comparative studies on allylestrenol and chlormadinone acetate Part I: Nocturnal penile tumescence monitoring]". Hinyokika Kiyo (in Japanese). 36 (2): 213–26. PMID 1693037.
- ↑ Geller J, Albert J, Geller S (1982). "Acute therapy with megestrol acetate decreases nuclear and cytosol androgen receptors in human BPH tissue". The Prostate. 3 (1): 11–5. doi:10.1002/pros.2990030103. PMID 6176985.
- ↑ Sander S, Nissen-Meyer R, Aakvaag A (1978). "On gestagen treatment of advanced prostatic carcinoma". Scand. J. Urol. Nephrol. 12 (2): 119–21. doi:10.3109/00365597809179977. PMID 694436.
- ↑ Hinman, Frank, Jr. (1983). Benign Prostatic Hypertrophy. Springer Science & Business Media. pp. 259, 266, 272. ISBN 978-1-4612-5476-8.
- ↑ Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA (25 August 2011). Campbell-Walsh Urology: Expert Consult Premium Edition: Enhanced Online Features and Print, 4-Volume Set. Elsevier Health Sciences. pp. 2938–. ISBN 978-1-4160-6911-9.
- ↑ A. Hughes; S. H. Hasan; G. W. Oertel; H. E. Voss, F. Bahner, F. Neumann, H. Steinbeck, K.-J. Gräf, J. Brotherton, H. J. Horn, R. K. Wagner (27 November 2013). Androgens II and Antiandrogens / Androgene II und Antiandrogene. Springer Science & Business Media. pp. 490–491. ISBN 978-3-642-80859-3.
- ↑ Wenderoth, U. K.; Jacobi, G. H. (1983). "Gonadotropin-releasing hormone analogues for palliation of carcinoma of the prostate". World Journal of Urology. 1 (1): 40–48. doi:10.1007/BF00326861. ISSN 0724-4983.
- 1 2 3 4 5 Thomas L. Lemke; David A. Williams (2008). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. pp. 1288–. ISBN 978-0-7817-6879-5.
- 1 2 3 Giorgetti R, di Muzio M, Giorgetti A, Girolami D, Borgia L, Tagliabracci A (March 2017). "Flutamide-induced hepatotoxicity: ethical and scientific issues" (PDF). Eur Rev Med Pharmacol Sci. 21 (1 Suppl): 69–77. PMID 28379593.
- 1 2 Erem C (2013). "Update on idiopathic hirsutism: diagnosis and treatment". Acta Clin Belg. 68 (4): 268–74. doi:10.2143/ACB.3267. PMID 24455796.
- 1 2 Moretti C, Guccione L, Di Giacinto P, Simonelli I, Exacoustos C, Toscano V, Motta C, De Leo V, Petraglia F, Lenzi A (March 2018). "Combined Oral Contraception and Bicalutamide in Polycystic Ovary Syndrome and Severe Hirsutism: A Double-Blind Randomized Controlled Trial". J. Clin. Endocrinol. Metab. 103 (3): 824–838. doi:10.1210/jc.2017-01186. PMID 29211888.
- 1 2 3 William D. Figg; Cindy H. Chau; Eric J. Small (14 September 2010). Drug Management of Prostate Cancer. Springer Science & Business Media. pp. 71–72. ISBN 978-1-60327-829-4.
- ↑ Caubet JF, Tosteson TD, Dong EW, Naylon EM, Whiting GW, Ernstoff MS, Ross SD (January 1997). "Maximum androgen blockade in advanced prostate cancer: a meta-analysis of published randomized controlled trials using nonsteroidal antiandrogens". Urology. 49 (1): 71–8. doi:10.1016/S0090-4295(96)00325-1. PMID 9000189.
- ↑ Bruce A. Chabner; Dan L. Longo (8 November 2010). Cancer Chemotherapy and Biotherapy: Principles and Practice. Lippincott Williams & Wilkins. pp. 680–. ISBN 978-1-60547-431-1.
- ↑ Neyman, A; Fuqua, JS; Eugster, EA (December 2017). "Bicalutamide as an Androgen Blocker with Secondary Effect of Promoting Feminization in Male to Female (MTF) Transgender Adolescents". Hormone Research in Paediatrics. 88: 1–628. doi:10.1159/000481424. PMID 28968603.
- ↑ Crawford ED, Schellhammer PF, McLeod DG, Moul JW, Higano CS, Shore N, Denis L, Iversen P, Eisenberger MA, Labrie F (May 2018). "Androgen Receptor-Targeted Treatments for Prostate Cancer: 35 Years' Progress with Antiandrogens". J. Urol. doi:10.1016/j.juro.2018.04.083. PMID 29730201.
- ↑ Ito Y, Sadar MD (2018). "Enzalutamide and blocking androgen receptor in advanced prostate cancer: lessons learnt from the history of drug development of antiandrogens". Res Rep Urol. 10: 23–32. doi:10.2147/RRU.S157116. PMC 5818862. PMID 29497605.
- 1 2 Ricci F, Buzzatti G, Rubagotti A, Boccardo F (November 2014). "Safety of antiandrogen therapy for treating prostate cancer". Expert Opin Drug Saf. 13 (11): 1483–99. doi:10.1517/14740338.2014.966686. PMID 25270521.
- ↑ Lutz Moser (1 January 2008). Controversies in the Treatment of Prostate Cancer. Karger Medical and Scientific Publishers. pp. 41–. ISBN 978-3-8055-8524-8.
- ↑ Prostate Cancer. Demos Medical Publishing. 20 December 2011. pp. 504–. ISBN 978-1-935281-91-7.
- ↑ Chang S (10 March 2010), Bicalutamide BPCA Drug Use Review in the Pediatric Population (PDF), U.S. Department of Health and Human Service, archived (PDF) from the original on 24 October 2016, retrieved 20 July 2016
- ↑ Kolvenbag GJ, Blackledge GR (January 1996). "Worldwide activity and safety of bicalutamide: a summary review". Urology. 47 (1A Suppl): 70–9, discussion 80–4. doi:10.1016/S0090-4295(96)80012-4. PMID 8560681.
- ↑ Vogelzang NJ (September 2012). "Enzalutamide--a major advance in the treatment of metastatic prostate cancer". N. Engl. J. Med. 367 (13): 1256–7. doi:10.1056/NEJMe1209041. PMID 23013078.
- ↑ J. Ramon; L.J. Denis (5 June 2007). Prostate Cancer. Springer Science & Business Media. pp. 256–. ISBN 978-3-540-40901-4.
- ↑ Hussain S, Haidar A, Bloom RE, Zayouna N, Piper MH, Jafri SM (2014). "Bicalutamide-induced hepatotoxicity: A rare adverse effect". Am J Case Rep. 15: 266–70. doi:10.12659/AJCR.890679. PMC 4068966. PMID 24967002.
- ↑ Gao Y, Maurer T, Mirmirani P (January 2018). "Understanding and Addressing Hair Disorders in Transgender Individuals". Am J Clin Dermatol. 19 (4): 517–527. doi:10.1007/s40257-018-0343-z. PMID 29352423.
Non-steroidal antiandrogens include flutamide, nilutamide, and bicalutamide, which do not lower androgen levels and may be favorable for individuals who want to preserve sex drive and fertility [9].
- ↑ Iversen P, Melezinek I, Schmidt A (Jan 2001). "Nonsteroidal antiandrogens: a therapeutic option for patients with advanced prostate cancer who wish to retain sexual interest and function". BJU International. 87 (1): 47–56. doi:10.1046/j.1464-410x.2001.00988.x. PMID 11121992.
- ↑ Morgante, E; Gradini, R; Realacci, M; Sale, P; D'eramo, G; Perrone, G A; Cardillo, M R; Petrangeli, E; Russo, Ma; Di Silverio, F (2001). "Effects of long-term treatment with the anti-androgen bicalutamide on human testis: an ultrastructural and morphometric study". Histopathology. 38 (3): 195–201. doi:10.1046/j.1365-2559.2001.01077.x. ISSN 0309-0167. PMID 11260298.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Engel JB, Schally AV (February 2007). "Drug Insight: clinical use of agonists and antagonists of luteinizing-hormone-releasing hormone". Nat Clin Pract Endocrinol Metab. 3 (2): 157–67. doi:10.1038/ncpendmet0399. PMID 17237842.
- 1 2 3 Shlomo Melmed (1 January 2016). Williams Textbook of Endocrinology. Elsevier Health Sciences. pp. 154–. ISBN 978-0-323-29738-7.
- ↑ Timothy L. Ratliff; William J. Catalona (6 December 2012). Genitourinary Cancer: Basic and Clinical Aspects. Springer Science & Business Media. pp. 158–. ISBN 978-1-4613-2033-3.
- ↑ Ezzati M, Carr BR (January 2015). "Elagolix, a novel, orally bioavailable GnRH antagonist under investigation for the treatment of endometriosis-related pain". Womens Health (Lond). 11 (1): 19–28. doi:10.2217/whe.14.68. PMID 25581052.
- 1 2 AbbVie (24 July 2018). "AbbVie Receives U.S. FDA Approval of ORILISSA™ (elagolix) for the Management of Moderate to Severe Pain Associated with Endometriosis". PR Newswire. Retrieved 31 July 2018.
- ↑ Conn PM, Crowley WF (January 1991). "Gonadotropin-releasing hormone and its analogues". N. Engl. J. Med. 324 (2): 93–103. doi:10.1056/NEJM199101103240205. PMID 1984190.
- ↑ Jerome F. Strauss; Jerome F. Strauss, III; Robert L. Barbieri (13 September 2013). Yen and Jaffe's Reproductive Endocrinology. Elsevier Health Sciences. pp. 272–. ISBN 978-1-4557-2758-2.
- 1 2 3 Krakowsky Y, Morgentaler A (July 2017). "Risk of Testosterone Flare in the Era of the Saturation Model: One More Historical Myth". Eur Urol Focus. doi:10.1016/j.euf.2017.06.008. PMID 28753828.
- ↑ Thompson IM (2001). "Flare Associated with LHRH-Agonist Therapy". Rev Urol. 3 Suppl 3: S10–4. PMC 1476081. PMID 16986003.
- 1 2 3 4 J. Larry Jameson; Leslie J. De Groot (25 February 2015). Endocrinology: Adult and Pediatric E-Book. Elsevier Health Sciences. pp. 2009, 2207, 2479. ISBN 978-0-323-32195-2.
- ↑ Louis J Denis; Keith Griffiths; Amir V Kaisary; Gerald P Murphy (1 March 1999). Textbook of Prostate Cancer: Pathology, Diagnosis and Treatment: Pathology, Diagnosis and Treatment. CRC Press. pp. 308–. ISBN 978-1-85317-422-3.
- ↑ Reilly DR, Delva NJ, Hudson RW (August 2000). "Protocols for the use of cyproterone, medroxyprogesterone, and leuprolide in the treatment of paraphilia". Can J Psychiatry. 45 (6): 559–63. doi:10.1177/070674370004500608. PMID 10986575.
[...] estrogen or antiandrogen treatment prior to the first leuprolide injection may reduce [the risk of symptoms caused by the testosterone "flare" at the initiation of treatment] (16).
- 1 2 3 Dittrich R, Binder H, Cupisti S, Hoffmann I, Beckmann MW, Mueller A (December 2005). "Endocrine treatment of male-to-female transsexuals using gonadotropin-releasing hormone agonist". Exp. Clin. Endocrinol. Diabetes. 113 (10): 586–92. doi:10.1055/s-2005-865900. PMID 16320157.
- 1 2 3 Loren S Schechter; Bauback Safa (23 June 2018). Gender Confirmation Surgery, An Issue of Clinics in Plastic Surgery, E-Book. Elsevier Health Sciences. pp. 314–. ISBN 978-0-323-61075-9.
- ↑ Everett E. Vokes; Harvey M. Golomb (28 June 2011). Oncologic Therapies. Springer Science & Business Media. pp. 493–. ISBN 978-3-642-55780-4.
- ↑ Cone, Allen (25 July 2018). "FDA approves drug to control endometriosis pain". UPI. Retrieved 31 July 2018.
- ↑ Bartsch G, Rittmaster RS, Klocker H (April 2000). "Dihydrotestosterone and the concept of 5alpha-reductase inhibition in human benign prostatic hyperplasia". Eur. Urol. 37 (4): 367–80. doi:10.1159/000020181. PMID 10765065.
- ↑ Yamana K, Labrie F, Luu-The V (August 2010). "Human type 3 5α-reductase is expressed in peripheral tissues at higher levels than types 1 and 2 and its activity is potently inhibited by finasteride and dutasteride". Horm Mol Biol Clin Investig. 2 (3): 293–9. doi:10.1515/HMBCI.2010.035. PMID 25961201.
- ↑ Jerry Shapiro; Nina Otberg (17 April 2015). Hair Loss and Restoration, Second Edition. CRC Press. pp. 39–40. ISBN 978-1-4822-3199-1.
- ↑ Ralph M. Trüeb; Won-Soo Lee (13 February 2014). Male Alopecia: Guide to Successful Management. Springer Science & Business Media. pp. 91–. ISBN 978-3-319-03233-7.
- ↑ Thomas L. Lemke; David A. Williams (24 January 2012). Foye's Principles of Medicinal Chemistry. Lippincott Williams & Wilkins. pp. 1397–1399. ISBN 978-1-60913-345-0.
- 1 2 3 4 5 6 7 Macias, Hector; Hinck, Lindsay (2012). "Mammary gland development". Wiley Interdisciplinary Reviews: Developmental Biology. 1 (4): 533–557. doi:10.1002/wdev.35. ISSN 1759-7684. PMC 3404495. PMID 22844349.
- 1 2 3 4 5 6 Sun, Susie X.; Bostanci, Zeynep; Kass, Rena B.; Mancino, Anne T.; Rosenbloom, Arlan L.; Klimberg, V. Suzanne; Bland, Kirby I. (2018). "Breast Physiology": 37–56.e6. doi:10.1016/B978-0-323-35955-9.00003-9.
- 1 2 3 4 5 6 7 8 Wierckx K, Gooren L, T'Sjoen G (2014). "Clinical review: Breast development in trans women receiving cross-sex hormones". J Sex Med. 11 (5): 1240–7. doi:10.1111/jsm.12487. PMID 24618412.
- ↑ Cox DB, Kent JC, Casey TM, Owens RA, Hartmann PE (March 1999). "Breast growth and the urinary excretion of lactose during human pregnancy and early lactation: endocrine relationships". Exp. Physiol. 84 (2): 421–34. doi:10.1017/S0958067099018072. PMID 10226182.
- 1 2 3 Wiegratz I, Kuhl H (August 2004). "Progestogen therapies: differences in clinical effects?". Trends Endocrinol. Metab. 15 (6): 277–85. doi:10.1016/j.tem.2004.06.006. PMID 15358281.
- ↑ Mary C. Brucker; Tekoa L. King (8 September 2015). Pharmacology for Women’s Health. Jones & Bartlett Publishers. pp. 368–. ISBN 978-1-284-05748-5.
- 1 2 Ilan H. Meyer; Mary E. Northridge (12 March 2007). The Health of Sexual Minorities: Public Health Perspectives on Lesbian, Gay, Bisexual and Transgender Populations. Springer. pp. 476–. ISBN 978-0-387-31334-4.
- ↑ Gianna E. Israel; Donald E. Tarver; Joy Diane Shaffer (1 March 2001). Transgender Care: Recommended Guidelines, Practical Information, and Personal Accounts. Temple University Press. pp. 58–. ISBN 978-1-56639-852-7.
- ↑ Richard Ekins; Dave King (23 October 2006). The Transgender Phenomenon. SAGE Publications. pp. 48–. ISBN 978-1-84787-726-0.
- 1 2 Kronawitter D, Gooren LJ, Zollver H, Oppelt PG, Beckmann MW, Dittrich R, Mueller A (August 2009). "Effects of transdermal testosterone or oral dydrogesterone on hypoactive sexual desire disorder in transsexual women: results of a pilot study". Eur. J. Endocrinol. 161 (2): 363–8. doi:10.1530/EJE-09-0265. PMID 19497984.
- ↑ Meyer WJ, Webb A, Stuart CA, Finkelstein JW, Lawrence B, Walker PA (April 1986). "Physical and hormonal evaluation of transsexual patients: a longitudinal study". Archives of Sexual Behavior. 15 (2): 121–38. doi:10.1007/bf01542220. PMID 3013122.
- ↑ Daniel R. Mishell; Val Davajan (1979). Reproductive endocrinology, infertility, and contraception. F. A. Davis Co. p. 224. ISBN 978-0-8036-6235-3.
It has been suggested that progestins be added during the last week of each cycle of estrogen therapy in order to develop more rounded breasts rather than the conical breasts many of these patients develop, but we have been unable to detect any difference in breast contour with or without progestins.
- ↑ Jerome F. Strauss; Robert L. Barbieri; Antonio R. Gargiulo (23 December 2017). Yen & Jaffe's Reproductive Endocrinology E-Book: Physiology, Pathophysiology, and Clinical Management. Elsevier Health Sciences. pp. 250–. ISBN 978-0-323-58232-2.
- ↑ Morris JM (June 1953). "The syndrome of testicular feminization in male pseudohermaphrodites". Am. J. Obstet. Gynecol. 65 (6): 1192–1211. doi:10.1016/0002-9378(53)90359-7. PMID 13057950.
- ↑ Lorincz AM, Sukumar S (2006). "Molecular links between obesity and breast cancer". Endocrine-related Cancer. 13 (2): 279–92. doi:10.1677/erc.1.00729. PMID 16728564.
Adipocytes make up the bulk of the human breast, with epithelial cells accounting for only approximately 10% of human breast volume.
- ↑ Howard BA, Gusterson BA (2000). "Human breast development". Journal of Mammary Gland Biology and Neoplasia. 5 (2): 119–37. PMID 11149569.
In the stroma, there is an increase in the amount of fibrous and fatty tissue, with the adult nonlactating breast consisting of 80% or more of stroma.
- ↑ Sperling MA (10 April 2014). Pediatric Endocrinology. Elsevier Health Sciences. pp. 598–. ISBN 978-1-4557-5973-6.
Estrogen stimulates the nipples to grow, mammary terminal duct branching to progress to the stage at which ductules are formed, and fatty stromal growth to increase until it constitutes about 85% of the mass of the breast. [...] Lobulation appears around menarche, when multiple blind saccular buds form by branching of the terminal ducts. These effects are due to the presence of progesterone. [...] Full alveolar development normally only occurs during pregnancy under the influence of additional progesterone and prolactin.
- ↑ Hagisawa S, Shimura N, Arisaka O (2012). "Effect of excess estrogen on breast and external genitalia development in growth hormone deficiency". Journal of Pediatric and Adolescent Gynecology. 25 (3): e61–3. doi:10.1016/j.jpag.2011.11.005. PMID 22206682.
Estrogen stimulates growth of the nipples, progression of mammary duct branching to the stage at which ductiles are formed, and fatty stromal growth until it constitutes about 85% of the mass of the breast.
- ↑ Gompel A (April 2012). "Micronized progesterone and its impact on the endometrium and breast vs. progestogens". Climacteric. 15 Suppl 1: 18–25. doi:10.3109/13697137.2012.669584. PMID 22432812.
- ↑ Cline JM, Wood CE (December 2008). "The Mammary Glands of Macaques". Toxicol Pathol. 36 (7): 134s–141s. doi:10.1177/0192623308327411. PMC 3070964. PMID 21475638.
- ↑ Pasqualini JR (2007). "Progestins and breast cancer". Gynecol. Endocrinol. 23 Suppl 1: 32–41. doi:10.1080/09513590701585003. PMID 17943537.
- ↑ Pasqualini JR (2009). "Breast cancer and steroid metabolizing enzymes: the role of progestogens". Maturitas. 65 Suppl 1: S17–21. doi:10.1016/j.maturitas.2009.11.006. PMID 19962254.
- ↑ Schindler AE (February 2011). "Dydrogesterone and other progestins in benign breast disease: an overview". Arch. Gynecol. Obstet. 283 (2): 369–71. doi:10.1007/s00404-010-1456-7. PMID 20383772.
- ↑ Winkler UH, Schindler AE, Brinkmann US, Ebert C, Oberhoff C (December 2001). "Cyclic progestin therapy for the management of mastopathy and mastodynia". Gynecol. Endocrinol. 15 Suppl 6: 37–43. PMID 12227885.
- 1 2 3 4 Ruan X, Mueck AO (November 2014). "Systemic progesterone therapy--oral, vaginal, injections and even transdermal?". Maturitas. 79 (3): 248–55. doi:10.1016/j.maturitas.2014.07.009. PMID 25113944.
- ↑ Bińkowska, Małgorzata; Woroń, Jarosław (2015). "Progestogens in menopausal hormone therapy". Menopausal Review. 2: 134–143. doi:10.5114/pm.2015.52154. ISSN 1643-8876.
- ↑ Kenneth L. Becker (2001). Principles and Practice of Endocrinology and Metabolism. Lippincott Williams & Wilkins. pp. 889–. ISBN 978-0-7817-1750-2.
- ↑ Sanjay Rajagopalan; Debabrata Mukherjee; Emile R. Mohler (2005). Manual of Vascular Diseases. Lippincott Williams & Wilkins. pp. 1–. ISBN 978-0-7817-4499-7.
- 1 2 Lee-Ellen C. Copstead-Kirkhorn; Jacquelyn L. Banasik (25 June 2014). Pathophysiology - E-Book. Elsevier Health Sciences. pp. 660–. ISBN 978-0-323-29317-4.
Throughout the reproductive years, some women note swelling of the breast around the latter part of each menstrual cycle before the onset of menstruation. The water retention and subsequent swelling of breast tissue during this phase of the menstrual cycle are thought to be due to high levels of circulating progesterone stimulating the secretory cells of the breast.12
- 1 2 Farage MA, Neill S, MacLean AB (2009). "Physiological changes associated with the menstrual cycle: a review". Obstet Gynecol Surv. 64 (1): 58–72. doi:10.1097/OGX.0b013e3181932a37. PMID 19099613.
- ↑ Worsley R, Santoro N, Miller KK, Parish SJ, Davis SR (March 2016). "Hormones and Female Sexual Dysfunction: Beyond Estrogens and Androgens--Findings from the Fourth International Consultation on Sexual Medicine". J Sex Med. 13 (3): 283–90. doi:10.1016/j.jsxm.2015.12.014. PMID 26944460.
- ↑ Reisman T, Goldstein Z (2018). "Case Report: Induced Lactation in a Transgender Woman". Transgend Health. 3 (1): 24–26. doi:10.1089/trgh.2017.0044. PMC 5779241. PMID 29372185.
- ↑ Kanhai RC, Hage JJ, van Diest PJ, Bloemena E, Mulder JW (January 2000). "Short-term and long-term histologic effects of castration and estrogen treatment on breast tissue of 14 male-to-female transsexuals in comparison with two chemically castrated men". The American Journal of Surgical Pathology. 24 (1): 74–80. doi:10.1097/00000478-200001000-00009. PMID 10632490.
- ↑ Lawrence, Anne A. (2007). "Transgender Health Concerns". The Health of Sexual Minorities: 473–505. doi:10.1007/978-0-387-31334-4_19.
- ↑ Paul Peter Rosen (2009). Rosen's Breast Pathology. Lippincott Williams & Wilkins. pp. 31–. ISBN 978-0-7817-7137-5.
- ↑ Apgar BS, Greenberg G (October 2000). "Using progestins in clinical practice". Am Fam Physician. 62 (8): 1839–46, 1849–50. PMID 11057840.
- 1 2 Goletiani NV, Keith DR, Gorsky SJ (2007). "Progesterone: review of safety for clinical studies" (PDF). Exp Clin Psychopharmacol. 15 (5): 427–44. doi:10.1037/1064-1297.15.5.427. PMID 17924777.
- ↑ Bäckström T, Bixo M, Johansson M, Nyberg S, Ossewaarde L, Ragagnin G, Savic I, Strömberg J, Timby E, van Broekhoven F, van Wingen G (2014). "Allopregnanolone and mood disorders". Prog. Neurobiol. 113: 88–94. doi:10.1016/j.pneurobio.2013.07.005. PMID 23978486.
- 1 2 3 Davey DA (March 2018). "Menopausal hormone therapy: a better and safer future". Climacteric: 1–8. doi:10.1080/13697137.2018.1439915. PMID 29526116.
- ↑ Raj R, Korja M, Koroknay-Pál P, Niemelä M (2018). "Multiple meningiomas in two male-to-female transsexual patients with hormone replacement therapy: A report of two cases and a brief literature review". Surg Neurol Int. 9: 109. doi:10.4103/sni.sni_22_18. PMC 5991277. PMID 29930875.
- ↑ Nota NM, Wiepjes CM, de Blok CJ, Gooren LJ, Peerdeman SM, Kreukels BP, den Heijer M (July 2018). "The occurrence of benign brain tumours in transgender individuals during cross-sex hormone treatment". Brain. 141 (7): 2047–2054. doi:10.1093/brain/awy108. PMID 29688280.
- ↑ Kuhl H (2011). "Pharmacology of Progestogens" (PDF). Journal für Reproduktionsmedizin und Endokrinologie-Journal of Reproductive Medicine and Endocrinology. 8 (1): 157–177.
- ↑ Kuhl H, Schneider HP (August 2013). "Progesterone--promoter or inhibitor of breast cancer". Climacteric. 16 Suppl 1: 54–68. doi:10.3109/13697137.2013.768806. PMID 23336704.
- 1 2 de Ziegler D, Fanchin R (2000). "Progesterone and progestins: applications in gynecology". Steroids. 65 (10–11): 671–9. doi:10.1016/S0039-128X(00)00123-9. PMID 11108875.
- 1 2 Hermann AC, Nafziger AN, Victory J, Kulawy R, Rocci ML, Bertino JS (2005). "Over-the-counter progesterone cream produces significant drug exposure compared to a food and drug administration-approved oral progesterone product". J Clin Pharmacol. 45 (6): 614–9. doi:10.1177/0091270005276621. PMID 15901742.
- ↑ Tollan A, Oian P, Kjeldsen SE, Eide I, Maltau JM (1993). "Progesterone reduces sympathetic tone without changing blood pressure or fluid balance in men". Gynecol. Obstet. Invest. 36 (4): 234–8. doi:10.1159/000292636. PMID 8300009.
- ↑ Unfer, Vittorio; di Renzo, Gian; Gerli, Sandro; Casini, Maria (2006). "The Use of Progesterone in Clinical Practice: Evaluation of its Efficacy in Diverse Indications Using Different Routes of Administration". Current Drug Therapy. 1 (2): 211–219. doi:10.2174/157488506776930923. ISSN 1574-8855.
- ↑ Brady BM, Anderson RA, Kinniburgh D, Baird DT (2003). "Demonstration of progesterone receptor-mediated gonadotrophin suppression in the human male". Clin. Endocrinol. (Oxf). 58 (4): 506–12. PMID 12641635.
- ↑ A. Wayne Meikle (1 June 1999). Hormone Replacement Therapy. Springer Science & Business Media. pp. 383, 389. ISBN 978-1-59259-700-0.
- ↑ Elliott S, Latini DM, Walker LM, Wassersug R, Robinson JW (September 2010). "Androgen deprivation therapy for prostate cancer: recommendations to improve patient and partner quality of life". J Sex Med. 7 (9): 2996–3010. doi:10.1111/j.1743-6109.2010.01902.x. PMID 20626600.
- ↑ Higano CS (February 2003). "Side effects of androgen deprivation therapy: monitoring and minimizing toxicity". Urology. 61 (2 Suppl 1): 32–8. doi:10.1016/S0090-4295(02)02397-X. PMID 12667885.
- ↑ Higano CS (October 2012). "Sexuality and intimacy after definitive treatment and subsequent androgen deprivation therapy for prostate cancer". J. Clin. Oncol. 30 (30): 3720–5. doi:10.1200/JCO.2012.41.8509. PMID 23008326.
- ↑ Eberhard Nieschlag; Hermann Behre (29 June 2013). Andrology: Male Reproductive Health and Dysfunction. Springer Science & Business Media. pp. 54–. ISBN 978-3-662-04491-9.
- ↑ Fisher, Alessandra Daphne; Maggi, Mario (2015). "Endocrine Treatment of Transsexual Male-to-Female Persons": 83–91. doi:10.1007/978-88-470-5696-1_10.
- ↑ Radix, Asa E. (2016). "Medical Transition for Transgender Individuals": 351–361. doi:10.1007/978-3-319-19752-4_19.
- ↑ de, Blok Christel; Klaver, Maartje; Nota, Nienke; Dekker, Marieke; den, Heijer Martin (2016). "Breast development in male-to-female transgender patients after one year cross-sex hormonal treatment". Endocrine Abstracts. doi:10.1530/endoabs.41.GP146. ISSN 1479-6848.
- ↑ de Blok CJ, Klaver M, Wiepjes CM, Nota NM, Heijboer AC, Fisher AD, Schreiner T, T'Sjoen G, den Heijer M (February 2018). "Breast Development in Transwomen After 1 Year of Cross-Sex Hormone Therapy: Results of a Prospective Multicenter Study". J. Clin. Endocrinol. Metab. 103 (2): 532–538. doi:10.1210/jc.2017-01927. PMID 29165635.
- ↑ Michael S. Baggish; Mickey M. Karram (18 August 2011). Atlas of Pelvic Anatomy and Gynecologic Surgery. Elsevier Health Sciences. pp. 1200–. ISBN 978-1-4557-1068-3.
- 1 2 3 4 5 6 Asscheman H, Gooren LJ (1992). "Hormone Treatment in Transsexuals". Archived from the original on 3 June 2012. Retrieved 13 June 2008.
- ↑ Meikle, James. "Breast regrowth procedure trialled for mastectomy patients". Retrieved 17 January 2015.
- ↑ Kirk, MD, Sheila (1999). Feminizing Hormonal Therapy For The Transgendered (1999 Edition). Pittsburgh, PA: Together Lifeworks. p. 38.
- 1 2 3 Giltay EJ, Gooren LJ (August 2000). "Effects of sex steroid deprivation/administration on hair growth and skin sebum production in transsexual males and females". Journal of Clinical Endocrinology and Metabolism. 85 (8): 2913–21. doi:10.1210/jc.85.8.2913. PMID 10946903.
- ↑ Randall, V. A.; Hibberts, N. A.; Thornton, M. J.; Hamada, K.; Merrick, A. E.; Kato, S.; Jenner, T. J.; De Oliveira, I.; Messenger, A. G. (2000-01-01). "The hair follicle: a paradoxical androgen target organ". Hormone Research. 54 (5–6): 243–250. doi:10.1159/000053266. ISSN 0301-0163. PMID 11595812.
- ↑ Leach NE, Wallis NE, Lothringer LL, Olson JA (May 1971). "Corneal hydration changes during the normal menstrual cycle--a preliminary study". The Journal of Reproductive Medicine. 6 (5): 201–4. PMID 5094729.
- ↑ Kiely PM, Carney LG, Smith G (October 1983). "Menstrual cycle variations of corneal topography and thickness". American Journal of Optometry and Physiological Optics. 60 (10): 822–9. doi:10.1097/00006324-198310000-00003. PMID 6650653.
- ↑ Gurwood AS, Gurwood I, Gubman DT, Brzezicki LJ (January 1995). "Idiosyncratic ocular symptoms associated with the estradiol transdermal estrogen replacement patch system". Optometry and Vision Science. 72 (1): 29–33. doi:10.1097/00006324-199501000-00006. PMID 7731653.
- ↑ Kirk, MD, Sheila (1999). Feminizing Hormonal Therapy For The Transgendered (1999 Edition). Pittsburgh, PA: Together Lifeworks. p. 56.
- ↑ Krenzer KL, Dana MR, Ullman MD, et al. (December 2000). "Effect of androgen deficiency on the human meibomian gland and ocular surface". The Journal of Clinical Endocrinology and Metabolism. 85 (12): 4874–82. doi:10.1210/jcem.85.12.7072. PMID 11134156.
- ↑ Sullivan DA, Sullivan BD, Evans JE, et al. (June 2002). "Androgen deficiency, Meibomian gland dysfunction, and evaporative dry eye". Annals of the New York Academy of Sciences. 966 (1): 211–22. Bibcode:2002NYASA.966..211S. doi:10.1111/j.1749-6632.2002.tb04217.x. PMID 12114274.
- ↑ Sullivan BD, Evans JE (December 2002). "Complete androgen insensitivity syndrome: effect on human meibomian gland secretions". Archives of Ophthalmology. 120 (12): 1689–1699. doi:10.1001/archopht.120.12.1689. PMID 12470144.
- ↑ Cermak JM, Krenzer KL, Sullivan RM, Dana MR, Sullivan DA (August 2003). "Is complete androgen insensitivity syndrome associated with alterations in the meibomian gland and ocular surface?". Cornea. 22 (6): 516–21. doi:10.1097/00003226-200308000-00006. PMID 12883343.
- ↑ Oprea L, Tiberghien A, Creuzot-Garcher C, Baudouin C (October 2004). "Influence des hormones sur le film lacrymal" [Hormonal regulatory influence in tear film]. Journal Français d'Ophtalmologie (in French). 27 (8): 933–41. doi:10.1016/S0181-5512(04)96241-9. PMID 15547478.
- ↑ Peterson's Principles of Oral and Maxillofacial Surgery. PMPH-USA. 2012. pp. 1209–. ISBN 978-1-60795-111-7.
- 1 2 3 4 Klein C., Gorzalka B.B. (2009). "Sexual functioning in transsexuals following hormone therapy and genital surgery: A review". Journal of Sexual Medicine. 6 (11): 2922–2939. doi:10.1111/j.1743-6109.2009.01370.x. PMID 20092545.
- ↑ Hulshoff, Cohen-Kettenis; et al. (July 2006). "Changing your sex changes your brain: influences of testosterone and estrogen on adult human brain structure". European Journal of Endocrinology. 155 (Suppl 1): 107–114. doi:10.1530/eje.1.02248. ISSN 0804-4643.
- ↑ Henriksson P, Eriksson A, Stege R, et al. (1988). "Cardiovascular follow-up of patients with prostatic cancer treated with single-drug polyestradiol phosphate". The Prostate. 13 (3): 257–61. doi:10.1002/pros.2990130308. PMID 3211807.
- von Schoultz B, Carlström K, Collste L, et al. (1989). "Estrogen therapy and liver function--metabolic effects of oral and parenteral administration". The Prostate. 14 (4): 389–95. doi:10.1002/pros.2990140410. PMID 2664738.
- Asscheman H, Gooren LJ, Eklund PL (September 1989). "Mortality and morbidity in transsexual patients with cross-gender hormone treatment". Metabolism: Clinical and Experimental. 38 (9): 869–873. doi:10.1016/0026-0495(89)90233-3. PMID 2528051.
- Aro J, Haapiainen R, Rasi V, Rannikko S, Alfthan O (1990). "The effect of parenteral estrogen versus orchiectomy on blood coagulation and fibrinolysis in prostatic cancer patients". European Urology. 17 (2): 161–5. PMID 2178941.
- Henriksson P, Blombäck M, Eriksson A, Stege R, Carlström K (March 1990). "Effect of parenteral oestrogen on the coagulation system in patients with prostatic carcinoma". British Journal of Urology. 65 (3): 282–5. doi:10.1111/j.1464-410X.1990.tb14728.x. PMID 2110842.
- Aro J (1991). "Cardiovascular and all-cause mortality in prostatic cancer patients treated with estrogens or orchiectomy as compared to the standard population". The Prostate. 18 (2): 131–7. doi:10.1002/pros.2990180205. PMID 2006119.
- Henriksson P, Stege R (1991). "Cost comparison of parenteral estrogen and conventional hormonal treatment in patients with prostatic cancer". International Journal of Technology Assessment in Health Care. 7 (2): 220–5. doi:10.1017/S0266462300005110. PMID 1907600.
- Henriksson P (Jan–Feb 1991). "Estrogen in patients with prostatic cancer. An assessment of the risks and benefits". Drug Safety. 6 (1): 47–53. doi:10.2165/00002018-199106010-00005. PMID 2029353.
- Caine YG, Bauer KA, Barzegar S, et al. (October 1992). "Coagulation activation following estrogen administration to postmenopausal women". Thrombosis and Haemostasis. 68 (4): 392–5. PMID 1333098.
- Stege R, Sander S (March 1993). "[Endocrine treatment of prostatic cancer. A renaissance for parenteral estrogen]". Tidsskrift for den Norske Lægeforening (in Norwegian). 113 (7): 833–5. PMID 8480286.
- Stege R, Carlström K, Hedlund PO, Pousette A, von Schoultz B, Henriksson P (September 1995). "[Intramuscular depot estrogens (Estradurin) in treatment of patients with prostate carcinoma. Historical aspects, mechanism of action, results and current clinical status]". Der Urologe. Ausg. A (in German). 34 (5): 398–403. PMID 7483157.
- Cox RL, Crawford ED (December 1995). "Estrogens in the treatment of prostate cancer". Journal of Urology. 154 (6): 1991–8. doi:10.1016/S0022-5347(01)66670-9. PMID 7500443.
- Henriksson P, Carlström K, Pousette A, et al. (July 1999). "Time for revival of estrogens in the treatment of advanced prostatic carcinoma? Pharmacokinetics, and endocrine and clinical effects, of a parenteral estrogen regimen". The Prostate. 40 (2): 76–82. doi:10.1002/(SICI)1097-0045(19990701)40:2<76::AID-PROS2>3.0.CO;2-Q. PMID 10386467.
- Hedlund PO, Henriksson P (March 2000). "Parenteral estrogen versus total androgen ablation in the treatment of advanced prostate carcinoma: effects on overall survival and cardiovascular mortality. The Scandinavian Prostatic Cancer Group (SPCG)-5 Trial Study". Urology. 55 (3): 328–33. doi:10.1016/S0090-4295(99)00580-4. PMID 10699602.
- Hedlund PO, Ala-Opas M, Brekkan E, et al. (2002). "Parenteral estrogen versus combined androgen deprivation in the treatment of metastatic prostatic cancer -- Scandinavian Prostatic Cancer Group (SPCG) Study No. 5". Scandinavian Journal of Urology and Nephrology. 36 (6): 405–13. doi:10.1080/003655902762467549. PMID 12623503.
- Scarabin PY, Oger E, Plu-Bureau G (August 2003). "Differential association of oral and transdermal oestrogen-replacement therapy with venous thromboembolism risk". Lancet. 362 (9382): 428–32. doi:10.1016/S0140-6736(03)14066-4. PMID 12927428.
- Straczek C, Oger E, Yon de Jonage-Canonico MB, et al. (November 2005). "Prothrombotic mutations, hormone therapy, and venous thromboembolism among postmenopausal women: impact of the route of estrogen administration". Circulation. 112 (22): 3495–500. doi:10.1161/CIRCULATIONAHA.105.565556. PMID 16301339.
- Ockrim J; Lalani el-N; Abel P (October 2006). "Therapy Insight: parenteral estrogen treatment for prostate cancer--a new dawn for an old therapy". Nature Clinical Practice Oncology. 3 (10): 552–63. doi:10.1038/ncponc0602. PMID 17019433.
- Basurto L, Saucedo R, Zárate A, et al. (2006). "Effect of pulsed estrogen therapy on hemostatic markers in comparison with oral estrogen regimen in postmenopausal women". Gynecologic and Obstetric Investigation. 61 (2): 61–4. doi:10.1159/000088603. PMID 16192735.
- Hemelaar M, Rosing J, Kenemans P, Thomassen MC, Braat DD, van der Mooren MJ (July 2006). "Less effect of intranasal than oral hormone therapy on factors associated with venous thrombosis risk in healthy postmenopausal women". Arteriosclerosis, Thrombosis, and Vascular Biology. 26 (7): 1660–6. doi:10.1161/01.ATV.0000224325.96659.53. PMID 16645152.
- Hedlund PO, Damber JE, Hagerman I, et al. (2008). "Parenteral estrogen versus combined androgen deprivation in the treatment of metastatic prostatic cancer: part 2. Final evaluation of the Scandinavian Prostatic Cancer Group (SPCG) Study No. 5". Scandinavian Journal of Urology and Nephrology. 42 (3): 220–9. doi:10.1080/00365590801943274. PMID 18432528.
- Canonico M, Plu-Bureau G, Lowe GD, Scarabin PY (May 2008). "Hormone replacement therapy and risk of venous thromboembolism in postmenopausal women: systematic review and meta-analysis". BMJ. 336 (7655): 1227–31. doi:10.1136/bmj.39555.441944.BE. PMC 2405857. PMID 18495631.
- ↑ Levy, Andy; Crown, Anna; Reid, Russell (2003-11-01). "Endocrine intervention for transsexuals". Clinical Endocrinology. 59 (4): 409–418. doi:10.1046/j.1365-2265.2003.01821.x. ISSN 0300-0664.
- ↑ Kirk, MD, Sheila (1999). Feminizing Hormonal Therapy For The Transgendered (1999 Edition). Pittsburgh, PA: Together Lifeworks. p. 52.
- 1 2 Gooren LJ, van Trotsenburg MA, Giltay EJ, van Diest PJ (2013). "Breast cancer development in transsexual subjects receiving cross-sex hormone treatment". J Sex Med. 10 (12): 3129–34. doi:10.1111/jsm.12319. PMID 24010586.
- 1 2 Brown GR, Jones KT (2015). "Incidence of breast cancer in a cohort of 5,135 transgender veterans" (PDF). Breast Cancer Res. Treat. 149 (1): 191–8. doi:10.1007/s10549-014-3213-2. PMID 25428790.
- 1 2 Cuhaci N, Polat SB, Evranos B, Ersoy R, Cakir B (2014). "Gynecomastia: Clinical evaluation and management". Indian J Endocrinol Metab. 18 (2): 150–8. doi:10.4103/2230-8210.129104. PMC 3987263. PMID 24741509.
- 1 2 Niewoehner CB, Schorer AE (2008). "Gynaecomastia and breast cancer in men". BMJ. 336 (7646): 709–13. doi:10.1136/bmj.39511.493391.BE. PMC 2276281. PMID 18369226.
- ↑ Christopher Li (11 November 2009). Breast Cancer Epidemiology. Springer Science & Business Media. pp. 266–. ISBN 978-1-4419-0685-4.
- ↑ Stella Pelengaris; Michael Khan (13 March 2013). The Molecular Biology of Cancer: A Bridge from Bench to Bedside. John Wiley & Sons. pp. 586–. ISBN 978-1-118-43085-9.
- ↑ Gilda Cardenosa (2004). Breast Imaging. Lippincott Williams & Wilkins. pp. 1–. ISBN 978-0-7817-4685-4.
- ↑ Gao YR, Walters KA, Desai R, Zhou H, Handelsman DJ, Simanainen U (2014). "Androgen receptor inactivation resulted in acceleration in pubertal mammary gland growth, upregulation of ERα expression, and Wnt/β-catenin signaling in female mice". Endocrinology. 155 (12): 4951–63. doi:10.1210/en.2014-1226. PMID 25076121.
- ↑ Jerome F. Strauss, III; Robert L. Barbieri (13 September 2013). Yen and Jaffe's Reproductive Endocrinology. Elsevier Health Sciences. pp. 236–. ISBN 978-1-4557-2758-2.
- ↑ Shlomo Melmed; Kenneth S. Polonsky; P. Reed Larsen; Henry M. Kronenberg (30 November 2015). Williams Textbook of Endocrinology. Elsevier Health Sciences. pp. 934–. ISBN 978-0-323-29738-7.
- ↑ Hughes IA, Werner R, Bunch T, Hiort O (2012). "Androgen insensitivity syndrome". Semin. Reprod. Med. 30 (5): 432–42. doi:10.1055/s-0032-1324728. PMID 23044881.
- ↑ Schoemaker MJ, Swerdlow AJ, Higgins CD, Wright AF, Jacobs PA (2008). "Cancer incidence in women with Turner syndrome in Great Britain: a national cohort study". Lancet Oncol. 9 (3): 239–46. doi:10.1016/S1470-2045(08)70033-0. PMID 18282803.
- 1 2 3 Gooren L, Morgentaler A (2014). "Prostate cancer incidence in orchidectomised male-to-female transsexual persons treated with oestrogens". Andrologia. 46 (10): 1156–60. doi:10.1111/and.12208. PMID 24329588.
- 1 2 3 Turo R, Jallad S, Prescott S, Cross WR (2013). "Metastatic prostate cancer in transsexual diagnosed after three decades of estrogen therapy". Can Urol Assoc J. 7 (7–8): E544–6. doi:10.5489/cuaj.175. PMC 3758950. PMID 24032068.
- ↑ Prostate Cancer. Demos Medical Publishing. 20 December 2011. pp. 460–. ISBN 978-1-935281-91-7.
Further reading
- Gooren LJ, Giltay EJ, Bunck MC (January 2008). "Long-term treatment of transsexuals with cross-sex hormones: extensive personal experience". J. Clin. Endocrinol. Metab. 93 (1): 19–25. doi:10.1210/jc.2007-1809. PMID 17986639.
- Gooren LJ (March 2011). "Clinical practice. Care of transsexual persons". N. Engl. J. Med. 364 (13): 1251–7. doi:10.1056/NEJMcp1008161. PMID 21449788.
- Wierckx K, Gooren L, T'Sjoen G (2014). "Clinical review: Breast development in trans women receiving cross-sex hormones". J Sex Med. 11 (5): 1240–7. doi:10.1111/jsm.12487. PMID 24618412.
- Fabris B, Bernardi S, Trombetta C (March 2015). "Cross-sex hormone therapy for gender dysphoria". J. Endocrinol. Invest. 38 (3): 269–82. doi:10.1007/s40618-014-0186-2. PMID 25403429.
- Tangpricha V, den Heijer M (April 2017). "Oestrogen and anti-androgen therapy for transgender women". Lancet Diabetes Endocrinol. 5 (4): 291–300. doi:10.1016/S2213-8587(16)30319-9. PMC 5366074. PMID 27916515.
- Unger CA (December 2016). "Hormone therapy for transgender patients". Transl Androl Urol. 5 (6): 877–884. doi:10.21037/tau.2016.09.04. PMC 5182227. PMID 28078219.
- Wesp LM, Deutsch MB (March 2017). "Hormonal and Surgical Treatment Options for Transgender Women and Transfeminine Spectrum Persons". Psychiatr. Clin. North Am. 40 (1): 99–111. doi:10.1016/j.psc.2016.10.006. PMID 28159148.
External links
- Hembree WC, Cohen-Kettenis PT, Gooren L, Hannema SE, Meyer WJ, Murad MH, Rosenthal SM, Safer JD, Tangpricha V, T'Sjoen GG (November 2017). "Endocrine Treatment of Gender-Dysphoric/Gender-Incongruent Persons: An Endocrine Society Clinical Practice Guideline" (PDF). J. Clin. Endocrinol. Metab. 102 (11): 3869–3903. doi:10.1210/jc.2017-01658. PMID 28945902.
- Coleman, E.; Bockting, W.; Botzer, M.; Cohen-Kettenis, P.; DeCuypere, G.; Feldman, J.; Fraser, L.; Green, J.; Knudson, G.; Meyer, W. J.; Monstrey, S.; Adler, R. K.; Brown, G. R.; Devor, A. H.; Ehrbar, R.; Ettner, R.; Eyler, E.; Garofalo, R.; Karasic, D. H.; Lev, A. I.; Mayer, G.; Meyer-Bahlburg, H.; Hall, B. P.; Pfaefflin, F.; Rachlin, K.; Robinson, B.; Schechter, L. S.; Tangpricha, V.; van Trotsenburg, M.; Vitale, A.; Winter, S.; Whittle, S.; Wylie, K. R.; Zucker, K. (2012). "Standards of Care for the Health of Transsexual, Transgender, and Gender-Nonconforming People, Version 7" (PDF). International Journal of Transgenderism. 13 (4): 165–232. doi:10.1080/15532739.2011.700873. ISSN 1553-2739.
- Deutsch M (17 June 2016). "Guidelines for the Primary and Gender-Affirming Care of Transgender and Gender Nonbinary People" (pdf) (2nd ed.). University of California, San Francisco: Center of Excellence for Transgender Health. p. 28.
- Dahl, M; Feldman, JL; Goldberg, J; Jaberi, A (2015). "Endocrine Therapy for Transgender Adults in British Columbia: Suggested Guidelines" (PDF). Vancouver Coastal Health. Retrieved 15 August 2018.
- Bourns, Amy (2015). "Guidelines and Protocols for Comprehensive Primary Care for Trans Clients" (PDF). Sherbourne Health Centre. Retrieved 15 August 2018.

