Estradiol cypionate
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation |
/ˌɛstrəˈdaɪoʊl ES-trə-DY-ohl sip-EYE-oh-nate[1] |
| Trade names | Depo-Estradiol, Depofemin, Estradep, many others |
| Synonyms | EC; E2C; Estradiol cipionate; Estradiol 17β-cyclopentyl-propionate; Estradiol 17β-cyclopentanepropionate |
| Routes of administration | Intramuscular injection, subcutaneous injection[2] |
| Drug class | Estrogen; Estrogen ester |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | IM: High |
| Metabolism | Cleavage via esterases in the liver, blood, and tissues[3][4] |
| Metabolites | Estradiol, cypionic acid, and metabolites of estradiol[3][4] |
| Elimination half-life | IM: 8–10 days[5] |
| Duration of action | IM (1–5 mg): 11–28 days or 1.5–4 weeks[6][5][7][8] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| ECHA InfoCard |
100.005.672 |
| Chemical and physical data | |
| Formula | C26H36O3 |
| Molar mass | 396.562 g/mol |
| 3D model (JSmol) | |
| |
| |
Estradiol cypionate, sold under the brand name Depo-Estradiol among others, is an estrogen medication which is used in hormone therapy for menopausal symptoms and low estrogen levels in women, in hormone therapy for transgender women, and in hormonal birth control for women.[7][4][9][10][11][12] It is given by injection into muscle once every 1 to 4 weeks.[7][8]
Side effects of estradiol cypionate include breast tenderness, breast enlargement, nausea, headache, and fluid retention.[7][4] Estradiol cypionate is a synthetic estrogen and hence is an agonist of the estrogen receptor (ER), the biological target of estrogens like estradiol.[4][3] Estradiol cypionate is an estrogen ester and a long-lasting prodrug of estradiol in the body.[7][4][3] Because of this, it is considered to be a natural and bioidentical form of estrogen.[3][13]
Estradiol cypionate was first described as well as introduced for medical use in 1952.[14][15] Along with estradiol valerate, it is one of the most commonly used esters of estradiol.[16] Estradiol cypionate has mostly been used in the United States, but is also marketed in a few other countries.[17][18][19] It is not currently available as a generic medication in the United States.[20]
Medical uses
The medical uses of estradiol cypionate are the same as those of estradiol and other estrogens. Examples of indications for the drug include hormone therapy and hormonal contraception. In regard to the latter, estradiol cypionate has been used in combination with medroxyprogesterone acetate as a combined injectable contraceptive.[11][12][21] Along with estradiol valerate, estradiol undecylate, and estradiol benzoate, estradiol cypionate is used as a form of high-dose estrogen therapy in feminizing hormone therapy for transgender women.[22][8][23][24]
Estradiol cypionate is usually used at a dosage of 1 to 5 mg by intramuscular injection every 3 to 4 weeks in the treatment of menopausal symptoms such as hot flashes and vaginal atrophy, at a dosage of 1.5 to 2 mg by intramuscular injection once a month in the treatment of female hypoestrogenism due to hypogonadism, and at a dosage of 2 to 10 mg by intramuscular injection once every 1 or 2 weeks for hormone therapy in transgender women.[7][8][23][22]
Available forms
Estradiol cypionate is and has been available as an oil solution for intramuscular injection provided in vials and ampoules at concentrations of 1, 3, and 5 mg/mL (and containing 5, 10, 15, 25, or 50 mg estradiol cypionate total).[20][25][26] The 1 and 3 mg/mL concentrations (containing 5 and 15 mg estradiol cypionate total) have been discontinued in the United States, but the 5 mg/mL concentration (containing 25 mg estradiol cypionate total) remains available.[20][27] Aside from estradiol cypionate, the only other injectable estrogen formulations that remain available in the United States are estradiol valerate (10 mg/mL, 20 mg/mL, and 40 mg/mL in oil) and conjugated estrogens (25 mg/vial in solution).[20]
In addition to single-drug formulations, estradiol cypionate has been marketed in the past in combination with medroxyprogesterone acetate (brand name Lunelle) and in combination with testosterone cypionate (brand name Depo-Testadiol), but these formulations have both been discontinued.[20]
Side effects
The side effects of estradiol cypionate are the same as those of estradiol. Examples of such side effects include breast tenderness and enlargement, nausea, vomiting, bloating, edema, headache, migraine, and melasma.[28][29] High-dose estrogen therapy with estradiol cypionate injections may also cause an increased risk of thromboembolism, changes in blood lipid profile, increased insulin resistance, and increased levels of prolactin.[29]
Pharmacology
Pharmacodynamics
Estradiol cypionate is an estradiol ester, or a prodrug of estradiol.[4][3] As such, it is an estrogen, or an agonist of the estrogen receptors.[4][3] The affinity of estradiol valerate for the estrogen receptor has been reported to be 50 times less than that of estradiol,[30] and estradiol valerate and estradiol cypionate have been found to possess similar affinity for the estrogen receptor.[31] Both estradiol cypionate and estradiol valerate are rapidly cleaved into estradiol in the body,[4] and estradiol valerate has been found to be unable to reach target tissues in any concentration of significance.[30] As such, estradiol valerate is regarded as essentially inactive in terms of estrogenic effect itself, acting solely as a prodrug to estradiol,[30] and estradiol cypionate is described as a prodrug of estradiol similarly.[3] Estradiol cypionate is of about 46% higher molecular weight than estradiol due to the presence of its C17β cypionate ester.[32][17] Because estradiol cypionate is a prodrug of estradiol, it is considered to be a natural and bioidentical form of estrogen.[3][13]
A study compared the combination of 5 mg estradiol cypionate and 25 mg medroxyprogesterone acetate as a combined injectable contraceptive (which has been associated with peak estradiol levels of around 300 pg/mL) with an ethinylestradiol-containing combined birth control pill and found that whereas the birth control pill produced significant changes in coagulation parameters, there were no significant prothrombotic effects of the combined injectable contraceptive on levels of fibrinogen, factors VII and X, plasminogen, or the activated prothrombin time.[33] As such, it appears that similarly to depot medroxyprogesterone acetate, combined injectable contraceptives with 5 mg estradiol cypionate and 25 mg medroxyprogesterone acetate have less or no procoagulant effect relative to combined birth control pills.[33]
| Estrogen | Type | EPD (14 days) | Duration | |
|---|---|---|---|---|
| Estradiol benzoate | Bioidentical | 25–30 mg | 5 mg ≈ 5 days | |
| Estradiol dipropionate | Bioidentical | 25–30 mg | 5 mg ≈ 5–8 days | |
| Estradiol valerate | Bioidentical | 20 mg | 10 mg ≈ 14 days | |
| Estradiol cypionate | Bioidentical | 25–30 mg | 5 mg ≈ 14 days | |
| Polyestradiol phosphate | Bioidentical | 40–60 mg | 40 mg ≈ 28 days | |
| Diethylstilbestrol | Synthetic | 20 mg | 3 mg ≈ 3 days | |
| Diethylstilbestrol dipropionate | Synthetic | 15 mg | 2.5 mg ≈ 5 days | |
| Addendum: An effective ovulation-inhibiting dose of estradiol undecylate is 20–30 mg/month.[34] Notes: All of the estrogens are by intramuscular injection. Abbreviations: EPD = Endometrial proliferation dose. Miscellaneous: Direct link to table. Sources: [35][36] | ||||
Pharmacokinetics
Intramuscular injection
In contrast to oral administration, which is associated with very low bioavailability (<10%), the bioavailability of both estradiol and estradiol esters like estradiol valerate has been found to be complete (i.e., 100%) via intramuscular injection.[30] In addition, estradiol esters like estradiol cypionate and estradiol valerate, when given intramuscularly in oil, have a relatively long duration due to the formation of an intramuscular depot from which they are slowly released and absorbed.[30][38] Upon intramuscular injection of estradiol cypionate in an oil solution, the solvent (i.e., oil) is absorbed, and a primary microcrystalline depot is formed within the muscle at the site of injection.[4] In addition, a secondary depot may also be formed in adipose tissue.[4] The slow release of estradiol cypionate is caused by the increased lipophilicity of the drug, which in turn is due to its long fatty acid cypionic acid ester moiety.[30] The terminal half-life of intramuscularly administered estradiol cypionate in oil (as estradiol) has been reported to be approximately 8 days.[13][39]
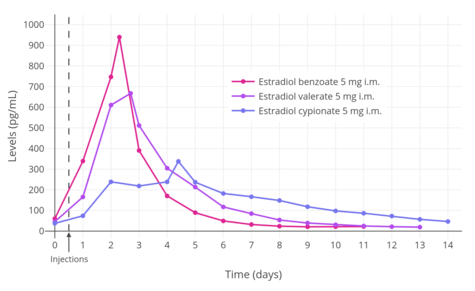
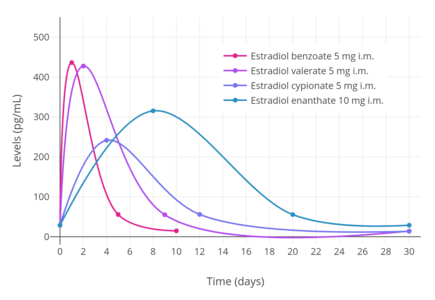
A single intramuscular injection of 5 mg estradiol cypionate has been found to result in peak circulating concentrations of 338 pg/mL estradiol and 145 pg/mL estrone, which occurred at about 4 and 5 days post-injection, respectively (see right table).[6] Compared to two other commonly used estradiol esters (which were also assessed in the study), estradiol cypionate had the longest duration, at approximately 11 days, whereas estradiol benzoate and estradiol valerate were found to last for 4 to 5 days and 7 to 8 days, respectively.[6] This is because estradiol cypionate has a more extensive fatty acid chain and in relation to this is comparatively more lipophilic.[4] For a given estradiol ester, the longer or more extensive the fatty acid chain is, the more lipophilic, longer-lasting, and more uniform/plateau-like the resultant levels of estradiol are as well as the lower the peak/maximal levels are (and hence less spike-like).[4]
Lunelle and Cyclofem are or were combined injectable contraceptives containing 5 mg estradiol cypionate and 25 mg medroxyprogesterone acetate for once-monthly intramuscular administration.[13][39] With these formulations, estradiol levels peak 2 to 3 days post-injection with average maximal circulating levels of about 250 pg/mL.[5][13][39] The terminal half-life of estradiol with these formulations is 8.4 to 10.1 days, and circulating estradiol levels return to baseline (~50 pg/mL) approximately 14 to 24 days post-injection.[5][13][39]
| Estrogen | Peak levels | Time to peak | Duration |
|---|---|---|---|
| Estradiol cypionate | E2: 338 pg/mL E1: 145 pg/mL | E2: 3.9 days E1: 5.1 days | 11 days |
| Estradiol valerate | E2: 667 pg/mL E1: 324 pg/mL | E2: 2.2 days E1: 2.7 days | 7–8 days |
| Estradiol benzoate | E2: 940 pg/mL E1: 343 pg/mL | E2: 1.8 days E1: 2.4 days | 4–5 days |
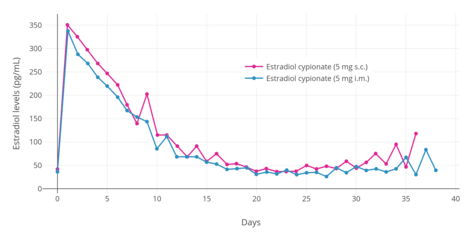
Subcutaneous injection
Estradiol cypionate in an aqueous suspension has been found to have equivalent effectiveness and virtually identical pharmacokinetics via subcutaneous and intramuscular injection.[2] However, subcutaneous injection is considered to be easier and less painful relative to intramuscular injection, and for these reasons, may result in comparatively greater satisfaction and compliance.[2]
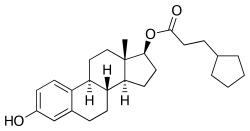
Chemistry
Estradiol cypionate is a synthetic estrane steroid and the C17β cyclopentylpropionate (or cypionate) fatty acid ester of estradiol.[32][17] It is also known as estra-1,3,5(10)-triene-3,17β-diol 17β-cyclopentylpropionate.[32][17] Other common esters of estradiol in use include estradiol valerate, estradiol enantate, and estradiol acetate, the former two of which are C17β esters of estradiol similarly to estradiol cypionate and the latter of which is the C3 acetate ester of estradiol.
History
Estradiol cypionate was patented by Upjohn in 1952, with a priority date of 1951.[25] It was first introduced for medical use by Upjohn in 1952 under the brand name Depo-Estradiol in the United States.[14][15] Subsequently, it was also marketed in other countries such as European countries and Japan.[25][15][17] Along with estradiol valerate (1954)[15][40] and estradiol benzoate (1936),[41][42] estradiol cypionate has become one of the most commonly used esters of estradiol.[16]
Society and culture
Generic names
Estradiol cypionate is the generic name of the drug and its INN and USAN.[32][17][18]
Brand names
Estradiol cypionate is or has been marketed under the brand names Depo-Estradiol, Depofemin, and Estradep, among many others.[32][17][18]
Availability
Estradiol cypionate is available both in the United States and in a few European countries such as Spain and Italy.[20][17] However, estradiol cypionate has mostly been used in the United States similarly to testosterone cypionate, with both of these medications having been developed by the American pharmaceutical company Upjohn.[17][19] Besides the United States, estradiol cypionate has been marketed in France, Germany, Italy, Spain, and Japan, among other countries.[25][15][17]
References
- ↑ https://www.drugs.com/cdi/estradiol-cypionate.html
- 1 2 3 4 Sierra-Ramírez JA, Lara-Ricalde R, Lujan M, Velázquez-Ramírez N, Godínez-Victoria M, Hernádez-Munguía IA, et al. (2011). "Comparative pharmacokinetics and pharmacodynamics after subcutaneous and intramuscular administration of medroxyprogesterone acetate (25 mg) and estradiol cypionate (5 mg)". Contraception. 84 (6): 565–70. doi:10.1016/j.contraception.2011.03.014. PMID 22078184.
- 1 2 3 4 5 6 7 8 9 Michael Oettel; Ekkehard Schillinger (6 December 2012). Estrogens and Antiestrogens II: Pharmacology and Clinical Application of Estrogens and Antiestrogen. Springer Science & Business Media. p. 261. ISBN 978-3-642-60107-1.
Natural estrogens considered here include: [...] Esters of 17β-estradiol, such as estradiol valerate, estradiol benzoate and estradiol cypionate. Esterification aims at either better absorption after oral administration or a sustained release from the depot after intramuscular administration. During absorption, the esters are cleaved by endogenous esterases and the pharmacologically active 17β-estradiol is released; therefore, the esters are considered as natural estrogens.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Kuhl H (2005). "Pharmacology of estrogens and progestogens: influence of different routes of administration" (PDF). Climacteric. 8 Suppl 1: 3–63. doi:10.1080/13697130500148875. PMID 16112947.
- 1 2 3 4 Thurman A, Kimble T, Hall P, Schwartz JL, Archer DF (2013). "Medroxyprogesterone acetate and estradiol cypionate injectable suspension (Cyclofem) monthly contraceptive injection: steady-state pharmacokinetics". Contraception. 87 (6): 738–43. doi:10.1016/j.contraception.2012.11.010. PMID 23265980.
- 1 2 3 4 5 6 Oriowo MA, Landgren BM, Stenström B, Diczfalusy E (April 1980). "A comparison of the pharmacokinetic properties of three estradiol esters". Contraception. 21 (4): 415–24. doi:10.1016/s0010-7824(80)80018-7. PMID 7389356.
- 1 2 3 4 5 6 https://www.accessdata.fda.gov/drugsatfda_docs/label/2005/085470s015lbl.pdf
- 1 2 3 4 Smith KP, Madison CM, Milne NM (December 2014). "Gonadal suppressive and cross-sex hormone therapy for gender dysphoria in adolescents and adults". Pharmacotherapy. 34 (12): 1282–97. doi:10.1002/phar.1487. PMID 25220381.
- ↑ ROBINSON WW (1953). "Estradiol cyclopentylpropionate: a new, long-acting, injectable estrogen". J. Clin. Endocrinol. Metab. 13 (10): 1279–80. doi:10.1210/jcem-13-10-1279. PMID 13096552.
- ↑ SCHWARTZ MM, SOULE SD (1955). "Estradiol 17-beta-cyclopentylpropionate, a long-acting estrogen". Am. J. Obstet. Gynecol. 70 (1): 44–50. doi:10.1016/0002-9378(55)90286-6. PMID 14388061.
- 1 2 Newton JR, D'arcangues C, Hall PE (1994). "A review of "once-a-month" combined injectable contraceptives". J Obstet Gynaecol (Lahore). 4 Suppl 1: S1–34. doi:10.3109/01443619409027641. PMID 12290848.
- 1 2 Bagade O, Pawar V, Patel R, Patel B, Awasarkar V, Diwate S (2014). "Increasing use of long-acting reversible contraception: safe, reliable, and cost-effective birth control" (PDF). World J Pharm Pharm Sci. 3 (10): 364–392. ISSN 2278-4357.
- 1 2 3 4 5 6 Nagrath Arun; Malhotra Narendra; Seth Shikha (15 December 2012). Progress in Obstetrics and Gynecology--3. Jaypee Brothers Medical Publishers Pvt. Ltd. pp. 416–419. ISBN 978-93-5090-575-3.
- 1 2 Marshall Sittig (1 January 1988). Pharmaceutical Manufacturing Encyclopedia. William Andrew. pp. 575–576. ISBN 978-0-8155-1144-1. Retrieved 20 May 2012.
- 1 2 3 4 5 William Andrew Publishing (22 October 2013). Pharmaceutical Manufacturing Encyclopedia, 3rd Edition. Elsevier. pp. 1476–1477. ISBN 978-0-8155-1856-3.
- 1 2 Samuel S. C. Yen (1991). Reproductive endocrinology: physiology, pathophysiology, and clinical management. Saunders. ISBN 978-0-7216-3206-3. Retrieved 20 May 2012.
- 1 2 3 4 5 6 7 8 9 10 Index Nominum 2000: International Drug Directory. Taylor & Francis US. 2000. p. 405. ISBN 978-3-88763-075-1. Retrieved 20 May 2012.
- 1 2 3 https://www.drugs.com/international/estradiol.html
- 1 2 William Llewellyn (2011). Anabolics. Molecular Nutrition Llc. pp. 426–. ISBN 978-0-9828280-1-4.
- 1 2 3 4 5 6 "Drugs@FDA: FDA Approved Drug Products". United States Food and Drug Administration. Retrieved 31 December 2017.
- ↑ Rowlands, S (2009). "New technologies in contraception". BJOG: An International Journal of Obstetrics & Gynaecology. 116 (2): 230–239. doi:10.1111/j.1471-0528.2008.01985.x. ISSN 1470-0328.
- 1 2 Wesp LM, Deutsch MB (March 2017). "Hormonal and Surgical Treatment Options for Transgender Women and Transfeminine Spectrum Persons". Psychiatr. Clin. North Am. 40 (1): 99–111. doi:10.1016/j.psc.2016.10.006. PMID 28159148.
- 1 2 Randi Ettner; Stan Monstrey; Eli Coleman (20 May 2016). Principles of Transgender Medicine and Surgery. Routledge. pp. 216–. ISBN 978-1-317-51460-2.
- ↑ Gianna E. Israel; Donald E. Tarver; Joy Diane Shaffer (1 March 2001). Transgender Care: Recommended Guidelines, Practical Information, and Personal Accounts. Temple University Press. pp. 64–. ISBN 978-1-56639-852-7.
- 1 2 3 4 A. Kleemann; J. Engel; B. Kutscher; D. Reichert (14 May 2014). Pharmaceutical Substances, 5th Edition, 2009: Syntheses, Patents and Applications of the most relevant APIs. Thieme. pp. 1167–1174. ISBN 978-3-13-179525-0.
- ↑ Kenneth L. Becker (2001). Principles and Practice of Endocrinology and Metabolism. Lippincott Williams & Wilkins. pp. 2153–. ISBN 978-0-7817-1750-2.
- ↑ Food and Drug Administration (2011). Approved Drug Products with Therapeutic Equivalence Evaluations - FDA Orange Book 31st Edition (2011): FDA Orange Book 31st Edition (2011). DrugPatentWatch.com. pp. 586–. ISBN 978-1-934899-81-6.
- ↑ Amit K. Ghosh (23 September 2010). Mayo Clinic Internal Medicine Board Review. OUP USA. pp. 222–. ISBN 978-0-19-975569-1.
- 1 2 Bishop BM (December 2015). "Pharmacotherapy Considerations in the Management of Transgender Patients: A Brief Review". Pharmacotherapy. 35 (12): 1130–9. doi:10.1002/phar.1668. PMID 26684553.
- 1 2 3 4 5 6 Düsterberg B, Nishino Y (December 1982). "Pharmacokinetic and pharmacological features of oestradiol valerate". Maturitas. 4 (4): 315–24. doi:10.1016/0378-5122(82)90064-0. PMID 7169965.
- ↑ Dubey RK, Jackson EK, Gillespie DG, Zacharia LC, Imthurn B, Keller PJ (2000). "Clinically used estrogens differentially inhibit human aortic smooth muscle cell growth and mitogen-activated protein kinase activity". Arterioscler. Thromb. Vasc. Biol. 20 (4): 964–72. doi:10.1161/01.atv.20.4.964. PMID 10764660.
- 1 2 3 4 5 J. Elks (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 898–. ISBN 978-1-4757-2085-3.
- 1 2 Kaunitz AM (December 2000). "Injectable contraception. New and existing options". Obstet. Gynecol. Clin. North Am. 27 (4): 741–80. doi:10.1016/S0889-8545(05)70171-6. PMID 11091987.
- ↑ Toppozada M (June 1977). "The clinical use of monthly injectable contraceptive preparations". Obstet Gynecol Surv. 32 (6): 335–47. doi:10.1097/00006254-197706000-00001. PMID 865726.
- ↑ Karl Knörr; Henriette Knörr-Gärtner; Fritz K. Beller; Christian Lauritzen (8 March 2013). Lehrbuch der Geburtshilfe und Gynäkologie: Physiologie und Pathologie der Reproduktion. Springer-Verlag. pp. 508–. ISBN 978-3-662-00526-2.
- ↑ Karl Knörr; Fritz K. Beller; Christian Lauritzen (17 April 2013). Lehrbuch der Gynäkologie. Springer-Verlag. pp. 212–213. ISBN 978-3-662-00942-0.
- 1 2 3 4 Garza-Flores J (April 1994). "Pharmacokinetics of once-a-month injectable contraceptives". Contraception. 49 (4): 347–59. doi:10.1016/0010-7824(94)90032-9. PMID 8013219.
- ↑ Sriram. Medicinal Chemistry. Pearson Education India. p. 427. ISBN 978-81-317-0031-0. Retrieved 20 May 2012.
- 1 2 3 4 Rahimy, Mohamad H; Ryan, Kristi K; Hopkins, Nancy K (1999). "Lunelle™ monthly contraceptive injection (medroxyprogesterone acetate and estradiol cypionate injectable suspension): steady-state pharmacokinetics of MPA and E2 in surgically sterile women". Contraception. 60 (4): 209–214. doi:10.1016/S0010-7824(99)00086-4. ISSN 0010-7824.
- ↑ Larry L. Duetsch (1969). Research and development, market power, and patent policy in ethical drugs. University of Wisconsin--Madison. p. 95.
- ↑ Enrique Raviña; Hugo Kubinyi (16 May 2011). The Evolution of Drug Discovery: From Traditional Medicines to Modern Drugs. John Wiley & Sons. p. 175. ISBN 978-3-527-32669-3. Retrieved 20 May 2012.
- ↑ Folley SJ (December 1936). "The effect of oestrogenic hormones on lactation and on the phosphatase of the blood and milk of the lactating cow" (PDF). The Biochemical Journal. 30 (12): 2262–72. PMC 1263335. PMID 16746289.