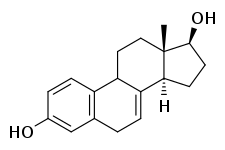
17β-Dihydroequilin
 | |
| Clinical data | |
|---|---|
| Synonyms | β-Dihydroequilin; Δ7-17β-Estradiol; 7-Dehydro-17β-estradiol; Estra-1,3,5(10),7-tetraen-3,17β-diol; NSC-12170 |
| Routes of administration | By mouth |
| Drug class | Estrogen |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| ChemSpider | |
| UNII | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C18H22O22 |
| Molar mass | 270.366 g/mol |
| 3D model (JSmol) | |
| |
| |
17β-Dihydroequilin is a naturally occurring estrogen sex hormone found in horses as well as a medication.[1][2] As the C3 sulfate ester sodium salt, it is a minor constituent (1.7%) of conjugated estrogens (CEEs; brand name Premarin).[1] However, as equilin, with equilin sulfate being a major component of CEEs, is transformed into 17β-dihydroequilin in the body, analogously to the conversion of estrone into estradiol, 17β-dihydroequilin is, along with estradiol, the most important estrogen responsible for the effects of CEEs.[1]
Pharmacology
Pharmacodynamics
17β-Dihydroequilin is an estrogen, or an agonist of the estrogen receptors (ERs), the ERα and ERβ.[1] In terms of relative binding affinity for the ERs, 17β-dihydroequilin has about 113% and 108% of that of estradiol for the ERα and ERβ, respectively.[1] 17β-Dihydroequilin has about 83% of the relative potency of CEEs in the vagina and 200% of the relative potency of CEEs in the uterus.[1] Of the equine estrogens, it shows the highest estrogenic activity and greatest estrogenic potency.[1]
Like CEEs as a whole, 17β-dihydroequilin has disproportionate effects in certain tissues such as the liver and uterus.[1] Equilin, the second major component of conjugated estrogens after estrone, is reversibly transformed into 17β-dihydroequilin analogously to the transformation of estrone into estradiol.[1] However, whereas the balance of mutual interconversion of estrone and estradiol is largely shifted in the direction of estrone, it is nearly equal in the case of equilin and 17β-dihydroequilin.[1] As such, although 17β-dihydroequilin is only a minor constituent of CEEs, it is, along with estradiol, the most important estrogen relevant to the estrogenic activity of the medication.[1]
| Estrogen | Type | HF | VE | UCa | FSH | LH | HDL-C | SHBG | CBG | AGT | Ratio |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Estradiol | Bioidentical | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Estrone | Bioidentical | ND | ND | ND | 0.3 | 0.3 | ND | ND | ND | ND | ND |
| Estriol | Bioidentical | 0.3 | 0.3 | 0.1 | 0.3 | ND | 0.2 | ND | ND | ND | 0.67 |
| Estrone sulfate | Bioidentical | ND | 0.9 | 0.9 | 0.9 | 0.9 | 0.5 | 0.9 | 0.7 | 1.5 | 0.56–1.7 |
| Conjugated estrogens | Natural | 1.2 | 1.5 | 2.0 | 1.1 | 1.0 | 1.5 | 3.0 | 1.5 | 5.0 | 1.3–4.5 |
| Equilin sulfate | Natural | ND | ND | ND | ND | ND | 6.0 | 7.5 | 6.0 | 7.5 | ND |
| Ethinylestradiol | Synthetic | 120 | 150 | 40 | 120 | 100 | 400 | 500 | 600 | 350 | 2.9–5.0 |
| Diethylstilbestrol | Synthetic | ND | ND | ND | 3.4 | ND | ND | 25.6 | 24.5 | 19.5 | 5.7–7.5 |
| Notes: Values are ratios, with estradiol as standard (i.e., 1.0). Abbreviations: HF = Clinical relief of hot flashes. VE = Increased proliferation of vaginal epithelium. UCa = Decrease in UCa. FSH = Suppression of FSH levels. LH = Suppression of LH levels. HDL-C, SHBG, CBG, and AGT = Increase in the serum levels of these hepatic proteins. Ratio = Ratio of liver protein effects to hot flashes relief and gonadotropin suppression. ND = No data. Type: Bioidentical = Identical to those found in humans. Natural = Naturally occurring but not identical to those found in humans (e.g., estrogens of other species). Synthetic = Man-made, does not naturally occur in animals or in the environment. Miscellaneous: Direct link to table. Sources: [1][3][4][5][6][7] | |||||||||||
Pharmacokinetics
17β-Dihydroequilin has about 30% of the relative binding affinity of testosterone for sex hormone-binding globulin (SHBG), relative to 50% for estradiol.[1] The metabolic clearance rate of 17β-dihydroequilin is 1,250 L/day/m2, relative to 580 L/day/m2 for estradiol.[1]
Chemistry
17β-Dihydroequilin, or simply β-dihydroequilin, also known as δ7-17β-estradiol or as 7-dehydro-17β-estradiol, as well as estra-1,3,5(10),7-tetraen-3,17β-diol, is a naturally occurring estrane steroid and an analogue of estradiol.[1] In terms of chemical structure and pharmacology, equilin (δ7-estrone) is to 17β-dihydroequilin as estrone is to estradiol.[1]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 Kuhl H (2005). "Pharmacology of estrogens and progestogens: influence of different routes of administration" (PDF). Climacteric. 8 Suppl 1: 3–63. doi:10.1080/13697130500148875. PMID 16112947.
- ↑ Marc A. Fritz; Leon Speroff (28 March 2012). Clinical Gynecologic Endocrinology and Infertility. Lippincott Williams & Wilkins. pp. 751–. ISBN 978-1-4511-4847-3.
- ↑ Alfred S. Wolf; H.P.G. Schneider (12 March 2013). Östrogene in Diagnostik und Therapie. Springer-Verlag. pp. 78–. ISBN 978-3-642-75101-1.
- ↑ Manfred Kaufmann; Serban-Dan Costa; Anton Scharl (27 November 2013). Die Gynäkologie. Springer-Verlag. pp. 105–. ISBN 978-3-662-11496-4.
- ↑ Mashchak CA, Lobo RA, Dozono-Takano R, Eggena P, Nakamura RM, Brenner PF, Mishell DR (November 1982). "Comparison of pharmacodynamic properties of various estrogen formulations". Am. J. Obstet. Gynecol. 144 (5): 511–8. doi:10.1016/0002-9378(82)90218-6. PMID 6291391.
- ↑ Helgason S (1982). "Estrogen replacement therapy after the menopause. Estrogenicity and metabolic effects". Acta Obstet Gynecol Scand Suppl. 107: 1–29. doi:10.3109/00016348209155333. PMID 6282033.
- ↑ Lobo RA, Nguyen HN, Eggena P, Brenner PF (February 1988). "Biologic effects of equilin sulfate in postmenopausal women". Fertil. Steril. 49 (2): 234–8. doi:10.1016/S0015-0282(16)59708-8. PMID 3338581.