Naltrexone
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | ReVia, Vivitrol, others |
| Synonyms | EN-1639A; UM-792; N-Cyclopropyl-methylnoroxymorphone; N-Cyclopropylmethyl-14-hydroxydihydro-morphinone; 17-(Cyclopropylmethyl)-4,5α-epoxy-3,14-dihydroxymorphinan-6-one |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a685041 |
| Pregnancy category | |
| Routes of administration | By mouth, intramuscular injection, subcutaneous implant |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 5–40% |
| Protein binding | 21% |
| Metabolism | Liver |
| Elimination half-life |
Naltrexone: 4 hours 6β-Naltrexol: 13 hours |
| Excretion | Urine |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| ECHA InfoCard |
100.036.939 |
| Chemical and physical data | |
| Formula | C20H23NO4 |
| Molar mass | 341.401 g/mol |
| 3D model (JSmol) | |
| Melting point | 169 °C (336 °F) |
| |
| |
| | |
Naltrexone, sold under the brand names ReVia and Vivitrol among others, is a medication primarily used to manage alcohol or opioid dependence.[1] An opioid-dependent person should not receive naltrexone before detoxification.[1] It is taken by mouth or by injection into a muscle.[1] Effects begin within 30 minutes.[1] A decreased desire for opioids, though, may take a few weeks.[1]
Side effects may include trouble sleeping, anxiety, nausea, and headaches.[1] In those still on opioids, opioid withdrawal may occur.[1] Use is not recommended in people with liver failure.[1] It is unclear if use is safe during pregnancy.[1][2] Naltrexone is an opioid antagonist and works by blocking the effects of opioids, both those from inside and outside the body.[1]
Naltrexone was first made in 1965 and was approved for medical use in the United States in 1984.[1][3] As of 2017, the wholesale cost of tablets is about US$0.74 per day in the US.[4][5] The extended-release injections cost about $1,267 per month ($41.20 per day).[5] Naltrexone, as bupropion/naltrexone, is also used to treat obesity.[6]
Medical uses
Alcoholism
Naltrexone has been best studied as a treatment for alcoholism.[7] Naltrexone has been shown to decrease the amount and frequency of drinking.[8] It does not appear to change the percentage of people drinking.[9] Its overall benefit has been described as "modest".[10]
Acamprosate may work better than naltrexone for eliminating drinking, while naltrexone may decrease the desire for alcohol to a greater extent.[11]
The Sinclair method is a method of using opiate antagonists such as naltrexone to treat alcoholism. The person takes the medication about an hour (and only then) before drinking to avoid side effects that arise from chronic use.[12][13] The opioid antagonist blocks the positive-reinforcement effects of alcohol and allows the person to stop or reduce drinking.[13]
Opioid use
Long-acting injectable naltrexone decreases heroin use more than placebo.[14] It has benefits over methadone and buprenorphine in that it is not a restricted medication.[14] It may decrease cravings for opioids after a number of weeks, and decreases the risk of overdose.[1][15] It is given once per month and has better compliance than the oral formulation.[16]
A 2011 review found insufficient evidence to determine the effect of naltrexone taken by mouth in opioid dependence.[17] While some do well with this formulation, it must be taken daily, and a person whose cravings become overwhelming can obtain opioid intoxication simply by skipping a dose. Due to this issue, the usefulness of oral naltrexone in opioid use disorders is limited by the low retention in treatment. Naltrexone by mouth remains an ideal treatment for a small number of people with opioid use, usually those with a stable social situation and motivation. With additional contingency management support, naltrexone may be effective in a broader population.[18]
Others
Naltrexone is not useful for quitting smoking.[19]
Available forms
Naltrexone is available and most commonly used in the form of an oral tablet (50 mg).[20] Vivitrol, a naltrexone formulation for depot injection containing 380 mg of the medication per vial, is also available.[20][21] Additionally, naltrexone subcutaneous implants that are surgically implanted are available.[22] While these are manufactured in Australia, they are not authorized for use within Australia, but only for export.[23] By 2009, naltrexone implants showed encouraging results.[24]
Contraindications
Naltrexone should not be used by persons with acute hepatitis or liver failure, or those with recent opioid use (typically 7–10 days).
Side effects
The most common side effects reported with naltrexone are gastrointestinal complaints such as diarrhea and abdominal cramping. These adverse effects are analogous to the symptoms of opioid withdrawal, as the mu receptor blockade will increase GI motility.
Naltrexone has been reported to cause liver damage (when given at doses higher than recommended). It carries an FDA boxed warning for this rare side effect. Due to these reports, some physicians may check liver function tests prior to starting naltrexone, and periodically thereafter. Concerns for liver toxicity initially arose from a study of nonaddicted obese patients receiving 300 mg of naltrexone.[25] Subsequent studies have suggested limited toxicity in other patient populations.
Naltrexone should not be started until several (typically 7-10) days of abstinence from opioids have been achieved. This is due to the risk of acute opioid withdrawal if naltrexone is taken, as naltrexone will displace most opioids from their receptors. The time of abstinence may be shorter than 7 days, depending on the half-life of the specific opioid taken. Some physicians use a naloxone challenge to determine whether an individual has any opioids remaining. The challenge involves giving a test dose of naloxone and monitoring for opioid withdrawal. If withdrawal occurs, naltrexone should not be started.[26]
Pharmacology
Pharmacodynamics
| Affinities (Ki) | Ratio | Ref | ||
|---|---|---|---|---|
| MOR | DOR | KOR | MOR:DOR:KOR | |
| 1.0 nM 0.0825 nM | 149 nM 8.02 nM | 3.9 nM 0.509 nM | 1:149:4 1:97:6 | [27] [28] |
Naltrexone and its active metabolite 6β-naltrexol are competitive antagonists at the μ-opioid receptor (MOR), the κ-opioid receptor (KOR) to a lesser extent, and, to a far lesser extent, at the δ-opioid receptor (DOR).[29]
Mechanism of action
The blockade of opioid receptors is the basis behind naltrexone's action in the management of opioid dependence—it reversibly blocks or attenuates the effects of opioids. Its mechanism of action in alcohol dependence is not fully understood, but as an opioid receptor antagonist is likely to be due to the modulation of the dopaminergic mesolimbic pathway (one of the primary centers for risk-reward analysis in the brain, and a tertiary "pleasure center") which is hypothesized to be a major center of the reward associated with addiction that all major drugs of abuse are believed to activate. Mechanism of action may be antagonism to endogenous opioids such as tetrahydropapaveroline, whose production is augmented in the presence of alcohol.[30]
Pharmacokinetics
Naltrexone is metabolized in the liver mainly to 6β-naltrexol by the enzyme dihydrodiol dehydrogenase. Other metabolites include 2-hydroxy-3-methoxy-6β-naltrexol and 2-hydroxy-3-methoxy-naltrexone. These are then further metabolized by conjugation with glucuronide. The plasma half-life of naltrexone and its metabolite 6β-naltrexol are about 4 hours and 13 hours, respectively.
Pharmacogenetics
A naltrexone treatment study by Anton et al., released by the National Institutes of Health in February 2008 and published in the Archives of General Psychiatry, has shown that alcoholics having a certain variant of the opioid receptor gene (G polymorphism of SNP Rs1799971 in the gene OPRM1), known as Asp40, demonstrated strong response to naltrexone and were far more likely to experience success at cutting back or discontinuing their alcohol intake altogether, while for those lacking the gene variant, naltrexone appeared to be no different from placebo.[31] The G allele of OPRM1 is most common in individuals of Asian descent, with 60% to 70% of people of Chinese, Japanese, and Indian ancestry having at least one copy, as opposed to 30% of Europeans and few Africans.[32]
Because of the characteristics of the patient group in the US, the first study was done on white patients, and the next was without regard for ethnicity. Anton et al. found that patients of African descent did not have much success with naltrexone in treatment for alcohol dependence because of lacking the relevant gene.[31]
As white patients with the gene had a five times greater rate of success in reducing drinking when given naltrexone than did patients without the gene, when used in a protocol of medical management (MM), Anton et al. concluded,
"Because almost 25% of the treatment-seeking population carries the Asp40 allele, genetic testing of individuals before naltrexone treatment might be worth the cost and effort, especially if structured behavioral treatment were not being considered."[31] This would enable treatment to be targeted by genetics to patients for whom it would be most effective. They noted, "Naltrexone is relatively easy to administer and free of serious adverse effects, and as we observed in the Asp40 carriers we studied, it appears to be highly effective."[31]
Studies have found naltrexone to be more efficacious among certain white subjects, because of the genetic basis, than among black subjects, who generally do not carry the relevant gene variant.[33] A 2009 study of naltrexone as an alcohol-dependence treatment among African Americans failed to find any statistically significant differences between naltrexone and a placebo.[34] Studies have suggested that carriers of the G allele may experience higher levels of craving and stronger "high" upon alcohol consumption, compared to carriers of the dominant allele, and naltrexone somewhat blunts these responses, leading to a reduction in alcohol use in some studies.[35]
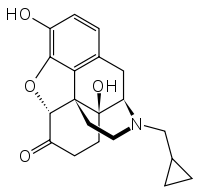
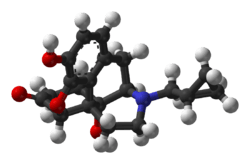
Chemistry
Naltrexone can be described as a substituted oxymorphone – here the tertiary amine methyl-substituent is replaced with methylcyclopropane. Naltrexone is the N-cyclopropylmethyl derivative of oxymorphone.
Analogues
The closely related medication, methylnaltrexone, is used to treat opioid-induced constipation, but does not treat addiction as it does not cross the blood–brain barrier. Nalmefene is similar to naltrexone and is used for the same purposes as naltrexone. Naltrexone should not be confused with naloxone, which is used in emergency cases of opioid overdose. Other related opioid antagonists include nalodeine and samidorphan.
History
Naltrexone was first synthesized in 1963 by Metossian at Endo Laboratories, a small pharmaceutical company in New York City.[36] It was characterized by Blumberg, Dayton, and Wolf in 1965 and was found to be an orally active, long-acting, and very potent opioid antagonist.[36][37][38][3] The drug showed advantages over earlier opioid antagonists such as cyclazocine, nalorphine, and naloxone, including its oral activity, a long duration of action allowing for once-daily administration, and a lack of dysphoria, and was selected for further development.[3] It was patented by Endo Laboratories in 1967 under the developmental code name EN-1639A and Endo Laboratories was acquired by DuPont in 1969.[39] Clinical trials for opioid dependence began in 1973, and a developmental collaboration of DuPont with the National Institute on Drug Abuse for this indication started the next year in 1974.[39] The drug was approved by the FDA for the oral treatment of opioid dependence in 1984, with the brand name Trexan, and for the oral treatment of alcohol dependence in 1995, when the brand name was changed by DuPont to ReVia.[39][20] A depot formulation for intramuscular injection was approved by the FDA under the brand name Vivitrol for alcohol dependence in 2006 and opioid dependence in 2010.[21][20]
Society and culture
Generic names
Naltrexone is the generic name of the drug and its INN, USAN, BAN, DCF, and DCIT, while naltrexone hydrochloride is its USP and BANM.[40][41][42][43]
Brand names
Naltrexone is or has been marketed under a variety of brand names, including Adepend, Antaxone, Celupan, Depade, Nalorex, Narcoral, Nemexin, Revia/ReVia, Trexan, and Vivitrol.[40][41][42][43] It is also marketed in combination with bupropion (bupropion/naltrexone) as Contrave and was marketed with morphine (morphine/naltrexone) as Embeda.[43] A combination of naltrexone with buprenorphine (buprenorphine/naltrexone) has been developed, but has not been marketed.[44]
Controversies
The FDA authorized use of injectable naltrexone for opioid addiction using a single study[45] that was led by Evgeny Krupitsky at Bekhterev Research Psychoneurological Institute, St Petersburg State Pavlov Medical University, St Petersburg, Russia,[46] a country where opioid agonists such as methadone and buprenorphine are not available. The study was a "double-blind, placebo-controlled, randomized", 24-week trial running "from July 3, 2008, through October 5, 2009" with "250 patients with opioid dependence disorder" at "13 clinical sites in Russia" on the use of injectable naltrexone (XR-NTX) for opioid dependence. The study was funded by the Boston-based biotech Alkermes firm which produces and markets naltrexone in the United States. A 2011 article reported that this single trial of naltrexone was performed not by comparing it to the best available, evidence-based treatment (methadone or buprenorphine), but by comparing it with a placebo.[47] A subsequent RCT in Norway did compare injectable naltrexone to buprenorphine and found them to be similar in outcomes.[48]
In May 2017, United States Secretary of Health and Human Services Tom Price, praised [Vivitrol] as the future of opioid addiction treatment after visiting the company’s plant in Ohio.[49] His remarks set off sharp criticism with almost 700 experts in the field of substance abuse submitting a letter to Price cautioning him about Vivitrol's "marketing tactics" and warning him that his comment "ignore widely accepted science".[50] The experts pointed out that Vivitrol's competitors, buprenorphine and methadone, are "less expensive", "more widely used", and have been "rigorously studied".
Price had claimed that buprenorphine and methadone were "simply substitute[s]" for "illicit drugs"[49] whereas according to the letter, "the substantial body of research evidence supporting these treatments is summarized in guidance from within your own agency, including the Substance Abuse and Mental Health Services Administration, the US Surgeon General, the National Institute on Drug Abuse, and the Centers for Disease Control and Prevention. To briefly summarize, buprenorphine and methadone have been demonstrated to be highly effective in managing the core symptoms of opioid use disorder, reducing the risk of relapse and fatal overdose, and encouraging long-term recovery."[50]
According to a June 11, 2017, The New York Times article, Alkermes "has spent years coaxing, with a deft lobbying strategy that has targeted lawmakers and law enforcement officials. The company has spent millions of dollars on contributions to officials struggling to stem the epidemic of opioid abuse. It has also provided thousands of free doses to encourage the use of Vivitrol in jails and prisons, which have by default become major detox centers".[49]
Research
Depersonalization
Naltrexone is sometimes used in the treatment of dissociative symptoms such as depersonalization and derealization.[51][52] Some studies suggest it might help.[53] Other small, preliminary studies have also shown benefit.[51][52] Blockade of the KOR by naltrexone and naloxone is thought to be responsible for their effectiveness in ameliorating depersonalization and derealization.[51][52] Since these drugs are less efficacious in blocking the KOR relative to the MOR, higher doses than typically used seem to be necessary.[51][52]
Low-dose
"Low-dose naltrexone" (LDN) describes the "off-label" use of naltrexone at low doses for diseases not related to chemical dependency or intoxication, such as multiple sclerosis.[54] More research needs to be done before it can be recommended for clinical use.
Although some scientific studies show its efficacy in some conditions such as fibromyalgia,[55] other, more dramatic claims for its use in conditions such as cancer and HIV have less scientific support.[54] This treatment has received significant attention on the Internet, especially through websites run by organizations promoting its use.[56]
Self-injury
Some studies suggest that self-injurious behaviors present in persons with developmental disabilities (including autism) can sometimes be remedied with naltrexone.[57] In these cases, the self-injury is believed to be done to release beta-endorphin, which binds to the same receptors as heroin and morphine.[58] If the "rush" generated by self-injury is removed, the behavior may stop.
Behavioral disorders
Some indications exist that naltrexone might be beneficial in the treatment of impulse-control disorders such as kleptomania, compulsive gambling, or trichotillomania (compulsive hair pulling), but evidence of its effectiveness for gambling is conflicting.[59][60][61] A 2008 case study reported successful use of naltrexone in suppressing and treating an internet pornography addiction.[62]
Interferon alpha
Naltrexone is effective in suppressing the cytokine-mediated adverse neuropsychiatric effects of interferon alpha therapy.[63][64]
See also
- Opioid antagonist § List of opioid antagonists
- One Little Pill (2014 film) - documentary about using naltrexone to treat alcohol use disorder
References
- 1 2 3 4 5 6 7 8 9 10 11 12 "Naltrexone Monograph for Professionals - Drugs.com". Drugs.com. American Society of Health-System Pharmacists. Archived from the original on 9 November 2017. Retrieved 9 November 2017.
- ↑ Tran, TH; Griffin, BL; Stone, RH; Vest, KM; Todd, TJ (July 2017). "Methadone, Buprenorphine, and Naltrexone for the Treatment of Opioid Use Disorder in Pregnant Women". Pharmacotherapy. 37 (7): 824–839. doi:10.1002/phar.1958. PMID 28543191.
- 1 2 3 Sadock, Benjamin J.; Sadock, Virginia A.; Sussman, Norman (2012). Kaplan & Sadock's Pocket Handbook of Psychiatric Drug Treatment. Lippincott Williams & Wilkins. p. 265. ISBN 9781451154467. Archived from the original on 2017-12-05.
- ↑ "Naltrexone". ATC/DDD Index. WHO Collaborating Centre for Drug Statistics Methodology. Archived from the original on 3 March 2016. Retrieved 11 July 2016.
DDD ... 50 mg
- 1 2 "NADAC as of 2017-11-29". Centers for Medicare and Medicaid Services. Archived from the original on 3 December 2017. Retrieved 3 December 2017.
- ↑ "Naltrexone/bupropion for obesity". Drug and therapeutics bulletin. 55 (11): 126–129. November 2017. doi:10.1136/dtb.2017.11.0550. PMID 29117992.
- ↑ Aboujaoude, E; Salame, WO (August 2016). "Naltrexone: A Pan-Addiction Treatment?". CNS Drugs. 30 (8): 719–33. doi:10.1007/s40263-016-0373-0. PMID 27401883.
- ↑ Rösner, S; Hackl-Herrwerth, A; Leucht, S; Vecchi, S; Srisurapanont, M; Soyka, M (8 December 2010). "Opioid antagonists for alcohol dependence". The Cochrane Database of Systematic Reviews (12): CD001867. doi:10.1002/14651858.CD001867.pub2. PMID 21154349.
- ↑ Donoghue, Kim; Elzerbi, Catherine; Saunders, Rob; Whittington, Craig; Pilling, Stephen; Drummond, Colin (2015). "The efficacy of acamprosate and naltrexone in the treatment of alcohol dependence, Europe versus the rest of the world: A meta-analysis". Addiction. 110 (6): 920–30. doi:10.1111/add.12875. PMID 25664494.
- ↑ c. Garbutt, James (2010). "Efficacy and Tolerability of Naltrexone in the Management of Alcohol Dependence". Current Pharmaceutical Design. 16 (19): 2091–7. doi:10.2174/138161210791516459. PMID 20482515.
- ↑ Maisel, Natalya C.; Blodgett, Janet C.; Wilbourne, Paula L.; Humphreys, Keith; Finney, John W. (October 17, 2012). "Meta-analysis of naltrexone and acamprosate for treating alcohol use disorders: When are these medications most helpful?". Addiction. 108 (2): 275–93. doi:10.1111/j.1360-0443.2012.04054.x. PMC 3970823. PMID 23075288.
- ↑ Anderson, Kenneth (Jul 28, 2013). "Drink Your Way Sober with Naltrexone". Psychology Today. Archived from the original on 17 September 2016. Retrieved 18 July 2016.
- 1 2 Sinclair, J. D. (2001). "Evidence about the use of naltrexone and for different ways of using it in the treatment of alcoholism". Alcohol and Alcoholism. 36 (1): 2–10. doi:10.1093/alcalc/36.1.2. PMID 11139409.
- 1 2 Sharma, A; Kelly, SM; Mitchell, SG; Gryczynski, J; O'Grady, KE; Schwartz, RP (June 2017). "Update on Barriers to Pharmacotherapy for Opioid Use Disorders". Current psychiatry reports. 19 (6): 35. doi:10.1007/s11920-017-0783-9. PMID 28526967.
- ↑ Sharma, B; Bruner, A; Barnett, G; Fishman, M (July 2016). "Opioid Use Disorders". Child and adolescent psychiatric clinics of North America. 25 (3): 473–87. doi:10.1016/j.chc.2016.03.002. PMC 4920977. PMID 27338968.
- ↑ Comer, Sandra D.; Sullivan, Maria A.; Yu, Elmer; Rothenberg, Jami L.; Kleber, Herbert D.; Kampman, Kyle; Dackis, Charles; o'Brien, Charles P. (2006). "Injectable, Sustained-Release Naltrexone for the Treatment of Opioid Dependence". Archives of General Psychiatry. 63 (2): 210–8. doi:10.1001/archpsyc.63.2.210. PMC 4200530. PMID 16461865.
- ↑ Minozzi, S; Amato, L; Vecchi, S; Davoli, M; Kirchmayer, U; Verster, A (13 April 2011). "Oral naltrexone maintenance treatment for opioid dependence". The Cochrane Database of Systematic Reviews (4): CD001333. doi:10.1002/14651858.CD001333.pub4. PMID 21491383.
- ↑ Johansson, Björn Axel; Berglund, Mats; Lindgren, Anna (2006). "Efficacy of maintenance treatment with naltrexone for opioid dependence: A meta-analytical review". Addiction. 101 (4): 491–503. doi:10.1111/j.1360-0443.2006.01369.x. PMID 16548929.
- ↑ David, Sean P.; Lancaster, Tim; Stead, Lindsay F.; Evins, A. Eden; Prochaska, Judith J. (6 June 2013). "Opioid antagonists for smoking cessation". The Cochrane Database of Systematic Reviews (6): CD003086. doi:10.1002/14651858.CD003086.pub3. ISSN 1469-493X. PMC 4038652. PMID 23744347.
- 1 2 3 4 H. Thomas Milhorn (17 October 2017). Substance Use Disorders: A Guide for the Primary Care Provider. Springer International Publishing. pp. 88–. ISBN 978-3-319-63040-3.
- 1 2 "Alcoholism Once A Month Injectable Drug, Vivitrol, Approved By FDA Archived 2009-01-05 at the Wayback Machine.," Medical News Today, April 16, 2006.
- ↑ Therapeutic Goods Administration. "Australian Register of Therapeutic Goods Medicines" (Online database of approved medicines). Archived from the original on 2009-05-14. Retrieved 2009-03-22.
- ↑ Therapeutic Goods Administration. "Australian Register of Therapeutic Goods Medicines" (Online database of approved medicines, specific entry for "O'Neil Long Acting Naltrexone Implant"). Retrieved 2017-04-27.
- ↑ Hulse, Gary K.; Morris, Noella; Arnold-Reed, Diane; Tait, Robert J. (2009). "Improving Clinical Outcomes in Treating Heroin Dependence". Archives of General Psychiatry. 66 (10): 1108–15. doi:10.1001/archgenpsychiatry.2009.130. PMID 19805701.
- ↑ Pfohl, David N.; Allen, John I.; Atkinson, Richard L.; Knopman, David S.; Malcolm, Robert J.; Mitchell, James E.; Morley, John E. (1986). "Naltrexone hydrochloride (Trexan): A review of serum transaminase elevations at high dosage". NIDA research monograph. 67: 66–72. PMID 3092099. Archived from the original on 2017-01-21.
- ↑ Galanter, Marc; Kleber, Herbert. The American Psychiatric Publishing Textbook of Substance Abuse Treatment, 4th Edition. ISBN 1585622761
- ↑ Raynor K, Kong H, Chen Y, Yasuda K, Yu L, Bell GI, Reisine T (1994). "Pharmacological characterization of the cloned kappa-, delta-, and mu-opioid receptors". Mol. Pharmacol. 45 (2): 330–4. PMID 8114680.
- ↑ Codd, E. E.; Shank, R. P.; Schupsky, J. J.; Raffa, R. B. (1995). "Serotonin and norepinephrine uptake inhibiting activity of centrally acting analgesics: Structural determinants and role in antinociception". The Journal of Pharmacology and Experimental Therapeutics. 274 (3): 1263–70. PMID 7562497. Archived from the original on 2017-02-02.
- ↑ Niciu, Mark J.; Arias, Albert J. (2013). "Targeted Opioid Receptor Antagonists in the Treatment of Alcohol Use Disorders". CNS Drugs. 27 (10): 777–87. doi:10.1007/s40263-013-0096-4. PMC 4600601. PMID 23881605.
- ↑ Haber, Hanka; Roske, Irmgard; Rottmann, Matthias; Georgi, Monika; Melzig, Matthias F. (1996). "Alcohol induces formation of morphine precursors in the striatum of rats". Life Sciences. 60 (2): 79–89. doi:10.1016/S0024-3205(96)00597-8. PMID 9000113.
- 1 2 3 4 Anton, Raymond F.; Oroszi, Gabor; o'Malley, Stephanie; Couper, David; Swift, Robert; Pettinati, Helen; Goldman, David (2008). "An Evaluation of μ-Opioid Receptor (OPRM1) as a Predictor of Naltrexone Response in the Treatment of Alcohol Dependence". Archives of General Psychiatry. 65 (2): 135–44. doi:10.1001/archpsyc.65.2.135. PMC 2666924. PMID 18250251.
- ↑ "Rs1799971 (SNPedia)". Archived from the original on 2011-11-27.
- ↑ Kranzler, Henry R.; Kirk, Jeffrey (2001). "Efficacy of Naltrexone and Acamprosate for Alcoholism Treatment: A Meta-Analysis". Alcoholism: Clinical and Experimental Research. 25 (9): 1335–41. doi:10.1111/j.1530-0277.2001.tb02356.x. PMID 11584154.
- ↑ Ray, Lara A.; Oslin, David W. (2009). "Naltrexone for the treatment of alcohol dependence among African Americans: Results from the COMBINE Study". Drug and Alcohol Dependence. 105 (3): 256–8. doi:10.1016/j.drugalcdep.2009.07.006. PMC 3409877. PMID 19717248.
- ↑ Ray, Lara A.; Barr, Christina S.; Blendy, Julie A.; Oslin, David; Goldman, David; Anton, Raymond F. (2012). "The Role of the Asn40Asp Polymorphism of the Mu Opioid Receptor Gene (OPRM1) on Alcoholism Etiology and Treatment: A Critical Review". Alcoholism: Clinical and Experimental Research. 36 (3): 385–94. doi:10.1111/j.1530-0277.2011.01633.x. PMC 3249007. PMID 21895723.
- 1 2 National Research Council (U.S.). Committee on Problems of Drug Dependence (1974). Report of the Thirty-sixth Annual Scientific Meeting: Committee on Problems of Drug Dependence, Mexico City, March 10-14, 1974. National Academies. pp. 265–. NAP:13963.
- ↑ Howard Padwa; Jacob Cunningham (2010). Addiction: A Reference Encyclopedia. ABC-CLIO. pp. 207–. ISBN 978-1-59884-229-6.
- ↑ G Bennett (14 January 2004). Treating Drug Abusers. Routledge. pp. 112–. ISBN 978-1-134-93173-6.
- 1 2 3 Joseph Wouk (1 March 2009). Google Ldn !. Lulu.com. pp. 78–88. ISBN 978-0-578-00439-6.
- 1 2 J. Elks (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 851–. ISBN 978-1-4757-2085-3.
- 1 2 Index Nominum 2000: International Drug Directory. Taylor & Francis. 2000. pp. 715–. ISBN 978-3-88763-075-1.
- 1 2 I.K. Morton; Judith M. Hall (6 December 2012). Concise Dictionary of Pharmacological Agents: Properties and Synonyms. Springer Science & Business Media. pp. 189–. ISBN 978-94-011-4439-1.
- 1 2 3 "Archived copy". Archived from the original on 2017-12-04. Retrieved 2017-12-04.
- ↑ McCann DJ (2008). "Potential of buprenorphine/naltrexone in treating polydrug addiction and co-occurring psychiatric disorders". Clin. Pharmacol. Ther. 83 (4): 627–30. doi:10.1038/sj.clpt.6100503. PMID 18212797.
- ↑ Armstrong, Walter (7 May 2013). "A Shot in the Dark: Can Vivitrol Help Us Control Our Addictions?". Pacific Standard. Archived from the original on 13 September 2017.
- ↑ Krupitsky, Evgeny; Nunes, Edward V.; Ling, Walter; Illeperuma, Ari; Gastfriend, David R.; Silverman, Bernard L. (April 28, 2011). "Injectable extended-release naltrexone for opioid dependence: a double-blind, placebo-controlled, multicentre randomised trial" (PDF). The Lancet. 377 (9776): 1506–13. doi:10.1016/s0140-6736(11)60358-9. Archived (PDF) from the original on September 12, 2017. Retrieved June 11, 2017.
- ↑ Wolfe, Daniel; Carrieri, MP; Dasgupta, Nabarun; Bruce, Douglas; Wodak, Alex (2011). "Injectable extended-release naltrexone for opioid dependence – Authors' reply". The Lancet. 378 (9792): 666. doi:10.1016/S0140-6736(11)61333-0.
- ↑ Tanum, L; Solli, KK; Latif, ZE; Benth, JŠ; Opheim, A; Sharma-Haase, K; Krajci, P; Kunøe, N (18 October 2017). "The Effectiveness of Injectable Extended-Release Naltrexone vs Daily Buprenorphine-Naloxone for Opioid Dependence: A Randomized Clinical Noninferiority Trial". JAMA Psychiatry. 74 (12): 1197–1205. doi:10.1001/jamapsychiatry.2017.3206. PMID 29049469.
- 1 2 3 Goodnough, Abby; Zernike, Kate (June 11, 2017). "Seizing on Opioid Crisis, a Drug Maker Lobbies Hard for Its Product". The New York Times. Archived from the original on June 11, 2017. Retrieved June 11, 2017.
Advertising for Vivitrol on a subway car in Brooklyn last month. Marketing for the drug has shifted into high gear.
- 1 2 "Letter to Tom Price". May 2017. Archived from the original on June 25, 2017. Retrieved June 11, 2017.
- 1 2 3 4 Daphne Simeon; Jeffrey Abugel (10 October 2008). Feeling Unreal: Depersonalization Disorder and the Loss of the Self. Oxford University Press. pp. 166–. ISBN 978-0-19-976635-2.
- 1 2 3 4 Ulrich F. Lanius, PhD; Sandra L. Paulsen, PhD; Frank M. Corrigan, MD (13 May 2014). Neurobiology and Treatment of Traumatic Dissociation: Towards an Embodied Self. Springer Publishing Company. pp. 489–. ISBN 978-0-8261-0632-2.
- ↑ Sierra, Mauricio (2014). "Depersonalization disorder: Pharmacological approaches". Expert Review of Neurotherapeutics. 8 (1): 19–26. doi:10.1586/14737175.8.1.19. PMID 18088198.
- 1 2 Novella, Steven (5 May 2010). "Low Dose Naltrexone – Bogus or Cutting Edge Science?". Science-Based Medicine. Archived from the original on 8 July 2011. Retrieved 5 July 2011.
- ↑ Younger, Jarred; MacKey, Sean (2009). "Fibromyalgia Symptoms Are Reduced by Low-Dose Naltrexone: A Pilot Study". Pain Medicine. 10 (4): 663–72. doi:10.1111/j.1526-4637.2009.00613.x. PMC 2891387. PMID 19453963.
- ↑ Bowling, Allen C. "Low-dose naltrexone (LDN) The "411" on LDN". National Multiple Sclerosis Society. Archived from the original on 22 December 2011. Retrieved 6 July 2011.
- ↑ Smith, Stanley G.; Gupta, Krishan K.; Smith, Sylvia H. (1995). "Effects of naltrexone on self-injury, stereotypy, and social behavior of adults with developmental disabilities". Journal of Developmental and Physical Disabilities. 7 (2): 137–46. doi:10.1007/BF02684958.
- ↑ Manley, Cynthia (1998-03-20). "Self-injuries may have biochemical base: study". The Reporter. Archived from the original on 2009-01-05.
- ↑ Grant, Jon E.; Kim, Suck Won; Odlaug, Brian L. (2009). "A Double-Blind, Placebo-Controlled Study of the Opiate Antagonist, Naltrexone, in the Treatment of Kleptomania". Biological Psychiatry. 65 (7): 600–6. doi:10.1016/j.biopsych.2008.11.022. PMID 19217077. Lay summary – Science Daily (April 3, 2009).
- ↑ "A Randomized, Double-Blind, Placebo-Controlled Trial of Naltrexone in the Treatment of Concurrent Alcohol Dependence and Pathological Gambling - ICH GCP - Clinical Trials Registry". Archived from the original on 2015-06-26.
- ↑ Kim, Suck Won; Grant, Jon E; Adson, David E; Shin, Young Chul (2001). "Double-blind naltrexone and placebo comparison study in the treatment of pathological gambling". Biological Psychiatry. 49 (11): 914–21. doi:10.1016/S0006-3223(01)01079-4. PMID 11377409.
- ↑ Bostwick, J. Michael; Bucci, Jeffrey A. (2008). "Internet Sex Addiction Treated with Naltrexone". Mayo Clinic Proceedings. 83 (2): 226–30. doi:10.4065/83.2.226. PMID 18241634.
- ↑ Vignau, J.; Karila, L.; Costisella, O.; Canva, V. (2005). "Hépatite C, Interféron α et dépression : Principales hypothèses physiopathologiques" [Hepatitis C, interferon a and depression: main physiopathologic hypothesis]. L'Encéphale (in French). 31 (3): 349–57. doi:10.1016/s0013-7006(05)82400-5. PMID 16142050. INIST:16920336.
- ↑ Małyszczak, Krzysztof; Inglot, Małgorzata; Pawłowski, Tomasz; Czarnecki, Marcin; Rymer, Weronika; Kiejna, Andrzej (2006). "Objawy neuropsychiatryczne w trakcie leczenia interferonem alfa" [Neuropsychiatric symptoms related to interferon alpha]. Psychiatria polska (in Polish). 40 (4): 787–97. PMID 17068950. Archived from the original on 2017-02-02.