Atomoxetine
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Strattera, others |
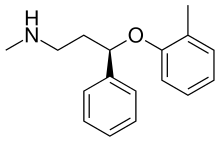
| Synonyms | (R)-N-Methyl-3-phenyl-3-(o-tolyloxy)propan-1-amine |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a603013 |
| Pregnancy category | |
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 63 to 94%[1][2][3] |
| Protein binding | 98%[1][2][3] |
| Metabolism | Hepatic, via CYP2D6[1][2][3] |
| Elimination half-life | 4.5-19 hours[1][2][3][4][5] |
| Excretion | Renal (80%) and faecal (17%)[1][2][3] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| ECHA InfoCard |
100.158.200 |
| Chemical and physical data | |
| Formula | C17H21NO |
| Molar mass |
255.36 g/mol 291.81 g/mol (hydrochloride) |
| 3D model (JSmol) | |
| |
| |
| | |
Atomoxetine, sold under the brand name Strattera among others, is a norepinephrine (noradrenaline) reuptake inhibitor which is approved for the treatment of attention deficit hyperactivity disorder (ADHD).[6] As of 2017, it is available as a generic medication in the United States.[7]
Medical uses
Attention deficit hyperactivity disorder
Atomoxetine is approved for use in children, adolescents, and adults.[6] However, its efficacy has not been studied in children under six years old.[2] Its primary advantage over the standard stimulant treatments for ADHD is that it has little known abuse potential.[2] While it has been shown to significantly reduce inattentive and hyperactive symptoms, the responses were lower than the response to stimulants. Additionally, 40% of participants who were treated with atomoxetine experienced significant residual ADHD symptoms.[8]
The initial therapeutic effects of atomoxetine usually take 2–4 weeks to become apparent.[1] A further 2–4 weeks may be required for the full therapeutic effects to be seen.[9] Its efficacy may be less than that of stimulant medications.[10]
Unlike α2 adrenoceptor agonists such as guanfacine and clonidine, atomoxetine's use can be abruptly stopped without significant discontinuation effects being seen.[2]
Contraindications
Contraindications include:[2]
- Hypersensitivity to atomoxetine or any of the excipients in the product
- Symptomatic cardiovascular disease including:
- -moderate to severe hypertension
- -atrial fibrillation
- -atrial flutter
- -ventricular tachycardia
- -ventricular fibrillation
- -ventricular flutter
- -advanced arteriosclerosis
- Severe cardiovascular disorders
- Pheochromocytoma
- Concomitant treatment with monoamine oxidase inhibitors
- Narrow angle glaucoma
- Poor metabolizers (due to the metabolism of atomoxetine by CYP2D6)
Adverse effects
Incidence of adverse effects:[2][3][11][12]
Very common (>10% incidence) adverse effects include:
- Nausea (26%)
- Xerostomia (Dry mouth) (20%)
- Appetite loss (16%)
- Insomnia (15%)
- Fatigue (10%)
- Headache
- Cough
Common (1–10% incidence) adverse effects include:
- Constipation (8%)
- Dizziness (8%)
- Erectile dysfunction (8%)
- Somnolence (sleepiness) (8%)
- Abdominal pain (7%)
- Urinary hesitation (6%)
- Tachycardia (high heart rate) (5–10%)
- Hypertension (high blood pressure) (5–10%)
- Irritability (5%)
- Abnormal dreams (4%)
- Dyspepsia (4%)
- Ejaculation disorder (4%)
- Hyperhidrosis (abnormally increased sweating) (4%)
- Vomiting (4%)
- Hot flashes (3%)
- Paraesthesia (sensation of tingling, tickling, etc.) (3%)
- Menstrual disorder (3%)
- Weight loss (2%)
- Depression
- Sinus headache
- Dermatitis
- Mood swings
Uncommon (0.1–1% incidence) adverse effects include:
- Suicide-related events
- Hostility
- Emotional lability
- Aggression
- Psychosis
- Syncope (fainting)
- Tremor
- Migraine
- Hypoaesthesia
- Seizure
- Palpitations
- Sinus tachycardia
- QT interval prolongation
- Increased blood bilirubin
- Allergic reactions
Rare (0.01–0.1% incidence) adverse effects including:
- Raynaud's phenomenon
- Abnormal/increased liver function tests
- Jaundice
- Hepatitis
- Liver injury
- Acute liver failure
- Urinary retention
- Priapism[13]
- Male genital pain
The FDA of the US has issued a black box warning for suicidal behaviour/ideation.[3] Similar warnings have been issued in Australia.[2][14] Unlike stimulant medications, atomoxetine does not have abuse liability or the potential to cause withdrawal effects on abrupt discontinuation.[2]
Overdose
Atomoxetine is relatively non-toxic in overdose. Single-drug overdoses involving over 1500 mg of atomoxetine have not resulted in death.[2] The most common symptoms of overdose include:[2]
- Gastrointestinal symptoms
- Somnolence
- Dizziness
- Tremor
- Abnormal behaviour
- Hyperactivity
- Agitation
- Dry mouth
- Tachycardia
- Hypertension
- Mydriasis
Less common symptoms:[2]
- Seizures
- QTc interval prolongation
The recommended treatment for atomoxetine overdose includes use of activated charcoal to prevent further absorption of the drug.[2]
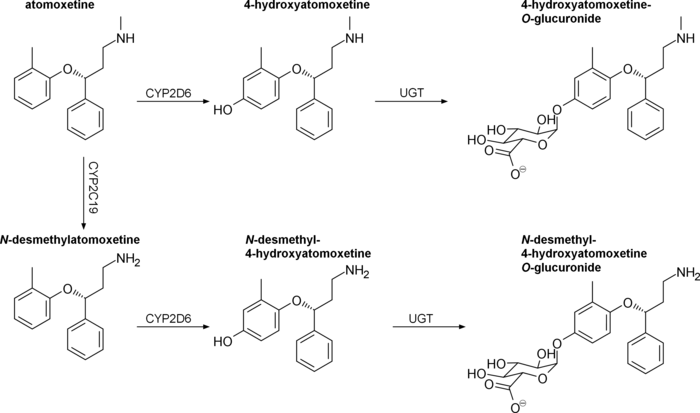
Interactions
Atomoxetine is a substrate for CYP2D6. Concurrent treatment with a CYP2D6 inhibitor such as bupropion, fluoxetine, or paroxetine has been shown to increase plasma atomoxetine by 100% or more, as well as increase N-desmethylatomoxetine levels and decrease plasma 4-hydroxyatomoxetine levels by a similar degree.[15][16][17]
Atomoxetine has been found to directly inhibit hERG potassium currents with an IC50 of 6.3 μM, which has the potential to cause arrhythmia.[16][18] QT prolongation has been reported with atomoxetine at therapeutic doses and in overdose; it is suggested that atomoxetine not be used with other medications that may prolong the QT interval, concomitantly with CYP2D6 inhibitors, and caution to be used in poor metabolizers.[16]
Other notable drug interactions include:[2]
- Antihypertensive agents, due to atomoxetine acting as an indirect sympathomimetic
- Indirect-acting sympathomimetics, such as pseudoephedrine, norepinephrine reuptake inhibitors, or MAOIs
- Direct-acting sympathomimetics, such as phenylephrine or other α1 adrenoceptor agonists, including pressors such as dobutamine or isoprenaline and β2 adrenoceptor agonists
- Highly plasma protein-bound drugs: atomoxetine has the potential to displace these drugs from plasma proteins which may potentiate their adverse or toxic effects. In vitro, atomoxetine does not affect the plasma protein binding of aspirin, desipramine, diazepam, paroxetine, phenytoin, or warfarin[4][19]
Pharmacology
Pharmacodynamics
| Site | ATX | 4-OH-ATX | N-DM-ATX | |
|---|---|---|---|---|
| SERT | 77 | 43 | ND | |
| NET | 5 | 3 | 92 | |
| DAT | 1,451 | ND | ND | |
| 5-HT1A | >1,000 | ND | ND | |
| 5-HT1B | >1,000 | ND | ND | |
| 5-HT1D | >1,000 | ND | ND | |
| 5-HT2 | 2,000 | 1,000 | 1,700 | |
| 5-HT6 | >1,000 | ND | ND | |
| 5-HT7 | >1,000 | ND | ND | |
| α1 | 11,400 | 20,000 | 19,600 | |
| α2A | 29,800 | >30,000 | >10,000 | |
| β1 | 18,000 | 56,100 | 32,100 | |
| M1 | >100,000 | >100,000 | >100,000 | |
| M2 | >100,000 | >100,000 | >100,000 | |
| D1 | >10,000 | >10,000 | >10,000 | |
| D2 | >10,000 | >10,000 | >10,000 | |
| H1 | 12,100 | >100,000 | >100,000 | |
| MOR | ND | 422 | ND | |
| DOR | ND | 300 | ND | |
| KOR | ND | 95 | ND | |
| σ1 | >1,000 | ND | ND | |
| GABAA | 200 | >30,000 | >10,000 | |
| NMDA | 3,470a | ND | ND | |
| Kir3.1/3.2 | 10,900b | ND | ND | |
| Kir3.2 | 12,400b | ND | ND | |
| Kir3.1/3.4 | 6,500b | ND | ND | |
| hERG | 6,300 | 20,000 | 5,710 | |
| Values are Ki (nM). The smaller the value, the more strongly the drug binds to the site. All values are for human receptors unless otherwise specified. arat cortex. bXenopus oocytes. Additional sources:[21][22][23][4][19] | ||||
Atomoxetine inhibits the presynaptic norepinephrine transporter (NET), preventing the reuptake of norepinephrine throughout the brain along with inhibiting the reuptake of dopamine in specific brain regions such as the prefrontal cortex, where dopamine transporter (DAT) expression is minimal.[4] In rats, atomoxetine increased prefrontal cortex catecholamine concentrations without altering dopamine levels in the striatum or nucleus accumbens; in contrast, methylphenidate, a dopamine reuptake inhibitor, was found to increase prefrontal, striatal, and accumbal dopamine levels to the same degree.[21] In mice, atomoxetine was also found to increase prefrontal catecholamine levels without affecting striatal or accumbal levels.[24]
Atomoxetine's status as a serotonin transporter (SERT) inhibitor at clinical doses in humans is uncertain. A PET imaging study on rhesus monkeys found that atomoxetine occupied >90% and >85% of neural NET and SERT, respectively.[25] However, both mouse and rat microdialysis studies have failed to find an increase in extracellular serotonin in the prefrontal cortex following acute or chronic atomoxetine treatment.[21][24] Supporting atomoxetine's selectivity, a human study found no effects on platelet serotonin uptake (a marker of SERT inhibition) and inhibition of the pressor effects of tyramine (a marker of NET inhibition).[26]
Atomoxetine has been found to act as an NMDA receptor antagonist in rat cortical neurons at therapeutic concentrations.[27][28] It causes a use-dependent open-channel block and its binding site overlaps with the Mg2+ binding site.[27][28] Atomoxetine's ability to increase prefrontal cortex firing rate in anesthetized rats could not be blocked by D1 or α2-adrenergic receptor antagonists, but could be potentiated by NMDA or an α1-adrenergic receptor antagonist, suggesting a glutaminergic mechanism.[29] In Sprague Dawley rats, atomoxetine reduces NR2B protein content without altering transcript levels.[30] Aberrant glutamate and NMDA receptor function have been implicated in the etiology of ADHD.[31][32]
Atomoxetine also reversibly inhibits GIRK currents in Xenopus oocytes in a concentration-dependent, voltage-independent, and time-independent manner.[33] Kir3.1/3.2 ion channels are opened downstream of M2, α2, D2, and A1 stimulation, as well as other Gi-coupled receptors.[33] Therapeutic concentrations of atomoxetine are within range of interacting with GIRKs, especially in CYP2D6 poor metabolizers.[33] It is not known whether this contributes to the therapeutic effects of atomoxetine in ADHD.
4-Hydroxyatomoxetine, the major active metabolite of atomoxetine in CYP2D6 extensive metabolizers, has been found to have sub-micromolar affinity for opioid receptors, acting as an antagonist at μ-opioid receptors and a partial agonist at κ-opioid receptors.[22] It is not known whether this contributes to the therapeutic effects of atomoxetine in ADHD.
Pharmacokinetics
Orally administered atomoxetine is rapidly and completely absorbed.[4] Hepatic first-pass metabolism is dependent on CYP2D6 activity, resulting in an absolute bioavailability of 63% for extensive metabolizers and 94% for poor metabolizers.[4] Maximum plasma concentration is reached in 1–2 hours.[4] If taken with food, the maximum plasma concentration decreases by 10-40% and delays the tmax by 1 hour.[4] Drugs affecting gastric pH have no effect on oral bioavailability.[34]
Atomoxetine has a volume of distribution of 0.85 L/kg, with limited partitioning into red blood cells.[4] It is highly bound to plasma proteins (98.7%), mainly albumin, along with α1-acid glycoprotein (77%) and IgG (15%).[4][19] Its metabolite N-desmethylatomoxetine is 99.1% bound to plasma proteins, while 4-hydroxyatomoxetine is only 66.6% bound.[4]
The half-life of atomoxetine varies widely between individuals, with an average range of 4.5 to 19 hours.[4][5] As atomoxetine is metabolized by CYP2D6, exposure may be increased 10-fold in CYP2D6 poor metabolizers.[5]
Atomoxetine, N-desmethylatomoxetine, and 4-hydroxyatomoxetine produce minimal to no inhbition of CYP1A2 and CYP2C9, but inhibit CYP2D6 in human liver microsomes at concentrations between 3.6-17 μmol/L.[4] Plasma concentrations of 4-hydroxyatomoxetine and N-desmethylatomoxetine at steady state are 1.0% and 5% that of atomoxetine in CYP2D6 extensive metabolizers, and are 5% and 45% that of atomoxetine in CYP2D6 poor metabolizers.[34]
Atomoxetine is excreted unchanged in urine at <3% in both extensive and poor CYP2D6 metabolizers, with >96% and 80% of a total dose being excreted in urine, respectively.[4] The fractions excreted in urine as 4-hydroxyatomoxetine and its glucuronide account for 86% of a given dose in extensive metabolizers, but only 40% in poor metabolizers.[4] CYP2D6 poor metabolizers excrete greater amounts of minor metabolites, namely N-desmethylatomoxetine and 2-hydroxymethylatomoxetine and their conjugates.[4]
Pharmacogenomics
Chinese adults homozygous for the hypoactive CYP2D6*10 allele have been found to exhibit two-fold higher AUCs and 1.5-fold higher maximum plasma concentrations compared to extensive metabolizers.[4]
Japanese men homozygous for CYP2D6*10 have similarly been found to experience two-fold higher AUCs compared to extensive metabolizers.[4]
Chemistry
Atomoxetine, or (−)-methyl[(3R)-3-(2-methylphenoxy)-3-phenylpropyl]amine, is a white, granular powder that is highly soluble in water.
 Strattera 60-mg capsule back
Strattera 60-mg capsule back Strattera 60-mg capsule front with Lilly logo
Strattera 60-mg capsule front with Lilly logo
Synthesis

Detection in biological fluids
Atomoxetine may be quantitated in plasma, serum or whole blood in order to distinguish extensive versus poor metabolizers in those receiving the drug therapeutically, to confirm the diagnosis in potential poisoning victims or to assist in the forensic investigation in a case of fatal overdosage.[37]
History
Atomoxetine is manufactured, marketed, and sold in the United States as the hydrochloride salt (atomoxetine HCl) under the brand name Strattera by Eli Lilly and Company, the original patent-filing company and current U.S. patent owner. Atomoxetine was initially intended to be developed as an antidepressant, but it was found to be insufficiently efficacious for treating depression. It was, however, found to be effective for ADHD and was approved by the FDA in 2002 for the treatment of ADHD. Its patent expired in May 2017.[38] On May 30, 2017 the FDA approved the generic production by four pharmaceutical companies.[39] On 12 August 2010, Lilly lost a lawsuit that challenged its patent on Strattera, increasing the likelihood of an earlier entry of a generic into the US market.[40] On 1 September 2010, Sun Pharmaceuticals announced it would begin manufacturing a generic in the United States.[41] In a 29 July 2011 conference call, however, Sun Pharmaceutical's Chairman stated "Lilly won that litigation on appeal so I think [generic Strattera]’s deferred."[42]
Society and culture
Brand names
In India, atomoxetine is sold under brand names including AXETRA, Axepta, Attera, Tomoxetin, and Attentin. In Australia and Romania, atomoxetine is sold under the brand name Strattera. In Iran, atomoxetine is sold under brand names including Stramox.
Research
There has been some suggestion that atomoxetine might be a helpful adjunct in people with major depression, particularly in cases with concomitant ADHD.[43][44][45]
See also
- Fluoxetine (4-trifluoromethyl instead of 2-methyl)
References
- 1 2 3 4 5 6 "atomoxetine (Rx) – Strattera". Medscape Reference. WebMD. Retrieved 10 November 2013.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 "STRATTERA® (atomoxetine hydrochloride)". TGA eBusiness Services. Eli Lilly Australia Pty. Limited. 21 August 2013. Retrieved 10 November 2013.
- 1 2 3 4 5 6 7 "ATOMOXETINE HYDROCHLORIDE capsule [Mylan Pharmaceuticals Inc.]". DailyMed. Mylan Pharmaceuticals Inc. October 2011. Retrieved 10 November 2013.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 Sauer, JM; Ring, BJ; Witcher, JW (2005). "Clinical pharmacokinetics of atomoxetine". Clinical pharmacokinetics. 44 (6): 571–90. doi:10.2165/00003088-200544060-00002. PMID 15910008.
- 1 2 3 Brown, JT; Bishop, JR (2015). "Atomoxetine pharmacogenetics: associations with pharmacokinetics, treatment response and tolerability". Pharmacogenomics. 16 (13): 1513–20. doi:10.2217/PGS.15.93. PMID 26314574.
- 1 2 "STRATTERA® (atomoxetine hydrochloride) CAPSULES for Oral Use. Full Prescribing Information" (PDF). Indianapolis, USA: Eli Lilly and Company. 20 February 2014. Retrieved 23 May 2014.
- ↑ "Press Announcements - FDA approves first generic Strattera for the treatment of ADHD". www.fda.gov. Retrieved 2 June 2017.
- ↑ Ghuman, Jaswinder K.; Hutchison, Shari L. (2014-11-01). "Atomoxetine is a second-line medication treatment option for ADHD". Evidence Based Mental Health. 17 (4): 108–108. doi:10.1136/eb-2014-101805. ISSN 1468-960X. PMID 25165169.
- ↑ Taylor, D; Paton, C; Shitij, K (2012). The Maudsley prescribing guidelines in psychiatry. West Sussex: Wiley-Blackwell. ISBN 978-0-470-97948-8.
- ↑ Kooij, JJS (2013). Adult ADHD Diagnostic Assessment and Treatment (PDF). Springer London. doi:10.1007/978-1-4471-4138-9. ISBN 978-1-4471-4137-2.
- ↑ "Strattera 10mg, 18mg, 25mg, 40mg, 60mg, 80mg or 100mg hard capsules". electronic Medicines Compendium. 28 May 2013. Retrieved 10 November 2013.
- ↑ "Strattera Product Insert". Retrieved 8 December 2013.
- ↑ "STRATTERA Medication Guide" (PDF). Eli Lilly and Company. 2003. Retrieved 17 December 2013.
- ↑ "Atomoxetine and suicidality in children and adolescents". Australian Prescriber. 36 (5). October 2013. p. 166. Archived from the original on 10 November 2013. Retrieved 10 November 2013.
- ↑ Todor, I; Popa, A; Neag, M; Muntean, D; Bocsan, C; Buzoianu, A; Vlase, L; Gheldiu, AM; Briciu, C (April–June 2016). "Evaluation of a Potential Metabolism-Mediated Drug-Drug Interaction Between Atomoxetine and Bupropion in Healthy Volunteers". Journal of pharmacy & pharmaceutical sciences : a publication of the Canadian Society for Pharmaceutical Sciences, Societe canadienne des sciences pharmaceutiques. 19 (2): 198–207. doi:10.18433/j3h03r. PMID 27518170.
- 1 2 3 Kasi, PM; Mounzer, R; Gleeson, GH (2011). "Cardiovascular side effects of atomoxetine and its interactions with inhibitors of the cytochrome p450 system". Case Reports in Medicine. 2011: 952584. doi:10.1155/2011/952584. PMC 3135225. PMID 21765848.
- ↑ Belle, DJ; Ernest, CS; Sauer, JM; Smith, BP; Thomasson, HR; Witcher, JW (November 2002). "Effect of potent CYP2D6 inhibition by paroxetine on atomoxetine pharmacokinetics". Journal of clinical pharmacology. 42 (11): 1219–27. doi:10.1177/009127002762491307. PMID 12412820.
- ↑ Scherer, D; Hassel, D; Bloehs, R; Zitron, E; von Löwenstern, K; Seyler, C; Thomas, D; Konrad, F; Bürgers, HF; Seemann, G; Rottbauer, W; Katus, HA; Karle, CA; Scholz, EP (January 2009). "Selective noradrenaline reuptake inhibitor atomoxetine directly blocks hERG currents". British Journal of Pharmacology. 156 (2): 226–36. doi:10.1111/j.1476-5381.2008.00018.x. PMC 2697834. PMID 19154426.
- 1 2 3 "21-411 Strattera Clinical Pharmacology Biopharmaceutics Review Part 2" (PDF).
- ↑ Roth, BL; Driscol, J. "PDSP Ki Database". Psychoactive Drug Screening Program (PDSP). University of North Carolina at Chapel Hill and the United States National Institute of Mental Health. Retrieved 14 August 2017.
- 1 2 3 Bymaster, FP; Katner, JS; Nelson, DL; Hemrick-Luecke, SK; Threlkeld, PG; Heiligenstein, JH; Morin, SM; Gehlert, DR; Perry, KW (November 2002). "Atomoxetine Increases Extracellular Levels of Norepinephrine and Dopamine in Prefrontal Cortex of Rat: A Potential Mechanism for Efficacy in Attention Deficit/Hyperactivity Disorder" (PDF). Neuropsychopharmacology. 27 (5): 699–711. doi:10.1016/S0893-133X(02)00346-9. PMID 12431845.
- 1 2 Creighton, CJ; Ramabadran, K; Ciccone, PE; Liu, J; Orsini, MJ; Reitz, AB (2 August 2004). "Synthesis and biological evaluation of the major metabolite of atomoxetine: elucidation of a partial kappa-opioid agonist effect". Bioorganic & Medicinal Chemistry Letters. 14 (15): 4083–5. doi:10.1016/j.bmcl.2004.05.018. PMID 15225731.
- ↑ Bymaster, FP; Katner, JS; Nelson, DL; Hemrick-Luecke, SK; Threlkeld, PG; Heiligenstein, JH; Morin, SM; Gehlert, DR; Perry, KW (November 2002). "Atomoxetine increases extracellular levels of norepinephrine and dopamine in prefrontal cortex of rat: a potential mechanism for efficacy in attention deficit/hyperactivity disorder". Neuropsychopharmacology. 27 (5): 699–711. doi:10.1016/S0893-133X(02)00346-9. PMID 12431845.
- 1 2 Koda, K; Ago, Y; Cong, Y; Kita, Y; Takuma, K; Matsuda, T (July 2010). "Effects of acute and chronic administration of atomoxetine and methylphenidate on extracellular levels of noradrenaline, dopamine and serotonin in the prefrontal cortex and striatum of mice". Journal of Neurochemistry. 114 (1): 259–70. doi:10.1111/j.1471-4159.2010.06750.x. PMID 20403082.
- ↑ Ding, Y.-S.; Naganawa, M.; Gallezot, J.-D.; Nabulsi, N.; Lin, S.-F.; Ropchan, J.; Weinzimmer, D.; McCarthy, T.J.; Carson, R.E.; Huang, Y.; Laruelle, M. (2014). "Clinical doses of atomoxetine significantly occupy both norepinephrine and serotonin transports: Implications on treatment of depression and ADHD". NeuroImage. 86: 164–171. doi:10.1016/j.neuroimage.2013.08.001. ISSN 1053-8119. PMID 23933039.
The noradrenergic action also exerts an important clinical effect in different antidepressant classes such as desipramine and nortriptyline (tricyclics, prevalent noradrenergic effect), reboxetine and atomoxetine (relatively pure noradrenergic reuptake inhibitor (NRIs)), and dual action antidepressants such as the serotonin noradrenaline reuptake inhibitors (SNRIs), the noradrenergic and dopaminergic reuptake inhibitor (NDRI) bupropion, and other compounds (e.g., mianserin, mirtazapine), which enhance the noradrenergic transmission
- ↑ Zerbe, RL; Rowe, H; Enas, GG; Wong, D; Farid, N; Lemberger, L (January 1985). "Clinical pharmacology of tomoxetine, a potential antidepressant". The Journal of Pharmacology and Experimental Therapeutics. 232 (1): 139–43. PMID 3965689.
- 1 2 Ludolph, AG; Udvardi, PT; Schaz, U; Henes, C; Adolph, O; Weigt, HU; Fegert, JM; Boeckers, TM; Föhr, KJ (May 2010). "Atomoxetine acts as an NMDA receptor blocker in clinically relevant concentrations". British Journal of Pharmacology. 160 (2): 283–291. doi:10.1111/j.1476-5381.2010.00707.x. PMC 2874851. PMID 20423340.
- 1 2 Barygin, OI; Nagaeva, EI; Tikhonov, DB; Belinskaya, DA; Vanchakova, NP; Shestakova, NN (1 April 2017). "Inhibition of the NMDA and AMPA receptor channels by antidepressants and antipsychotics". Brain Research. 1660: 58–66. doi:10.1016/j.brainres.2017.01.028. PMID 28167075.
- ↑ Di Miceli, M; Gronier, B (June 2015). "Psychostimulants and atomoxetine alter the electrophysiological activity of prefrontal cortex neurons, interaction with catecholamine and glutamate NMDA receptors". Psychopharmacology. 232 (12): 2191–205. doi:10.1007/s00213-014-3849-y. PMID 25572531.
- ↑ Udvardi, PT; Föhr, KJ; Henes, C; Liebau, S; Dreyhaupt, J; Boeckers, TM; Ludolph, AG (2013). "Atomoxetine affects transcription/translation of the NMDA receptor and the norepinephrine transporter in the rat brain--an in vivo study". Drug Design, Development and Therapy. 7: 1433–46. doi:10.2147/DDDT.S50448. PMC 3857115. PMID 24348020.
- ↑ Maltezos, S; Horder, J; Coghlan, S; Skirrow, C; O'Gorman, R; Lavender, TJ; Mendez, MA; Mehta, M; Daly, E; Xenitidis, K; Paliokosta, E; Spain, D; Pitts, M; Asherson, P; Lythgoe, DJ; Barker, GJ; Murphy, DG (18 March 2014). "Glutamate/glutamine and neuronal integrity in adults with ADHD: a proton MRS study". Translational psychiatry. 4: e373. doi:10.1038/tp.2014.11. PMC 3966039. PMID 24643164.
- ↑ Chang, JP; Lane, HY; Tsai, GE (2014). "Attention deficit hyperactivity disorder and N-methyl-D-aspartate (NMDA) dysregulation". Current Pharmaceutical Design. 20 (32): 5180–5. doi:10.2174/1381612819666140110115227. PMID 24410567.
- 1 2 3 Kobayashi, T; Washiyama, K; Ikeda, K (June 2010). "Inhibition of G-protein-activated inwardly rectifying K+ channels by the selective norepinephrine reuptake inhibitors atomoxetine and reboxetine". Neuropsychopharmacology. 35 (7): 1560–9. doi:10.1038/npp.2010.27. PMC 3055469. PMID 20393461.
- 1 2 "Strattera Package Insert" (PDF). FDA.
- ↑ A US patent 4018895 A, Bryan B. Molloy & Klaus K. Schmiegel, "Aryloxyphenylpropylamines in treating depression", published 1977-04-19, assigned to Eli Lilly And Company
- ↑ B1 US patent EP0052492 B1, Bennie Joe Foster & Edward Ralph Lavagnino, "3-aryloxy-3-phenylpropylamines", published 1984-02-29, assigned to Eli Lilly And Company
- ↑ Baselt, Randall C. (2008). Disposition of Toxic Drugs and Chemicals in Man (8th ed.). Foster City, CA: Biomedical Publications. pp. 118–20. ISBN 0-931890-08-X.
- ↑ "Patent and Exclusivity Search Results". Electronic Orange Book. US Food and Drug Administration. Retrieved 26 April 2009.
- ↑ "FDA approves first generic Strattera for the treatment of ADHD". U.S. Food and Drug Administration. May 30, 2017. Retrieved January 1, 2018.
- ↑ "Drugmaker Eli Lilly loses patent case over ADHD drug, lowers revenue outlook". Chicago Tribune.
- ↑ "Sun Pharma receives USFDA approval for generic Strattera capsules". International Business Times. Archived from the original on 7 April 2011.
- ↑ "Sun Pharma Q1 2011-12 Earnings Call Transcript 10.00 am, July 29, 2011" (PDF). Archived from the original (PDF) on 29 September 2011.
- ↑ Spencer TJ, Faraone SV, Michelson D, Adler LA, Reimherr FW, Glatt SJ & Biederman J (March 2006). "Atomoxetine and adult attention-deficit/hyperactivity disorder: the effects of comorbidity". The Journal of Clinical Psychiatry. 67 (3): 415–20. doi:10.4088/JCP.v67n0312. PMID 16649828.
- ↑ Carpenter LL, Milosavljevic N, Schecter JM, Tyrka AR, Price LH (October 2005). "Augmentation with open-label atomoxetine for partial or non-response to antidepressants". The Journal of Clinical Psychiatry. 66 (10): 1234–8. doi:10.4088/JCP.v66n1005. PMID 16259536.
- ↑ Kratochvil CJ, Newcorn JH, Arnold LE, Duesenberg D, Emslie GJ, Quintana H, Sarkis EH, Wagner KD, Gao H, Michelson D & Biederman J (September 2005). "Atomoxetine alone or combined with fluoxetine for treating ADHD with comorbid depressive or anxiety symptoms". Journal of the American Academy of Child and Adolescent Psychiatry. 44 (9): 915–24. doi:10.1097/01.chi.0000169012.81536.38. PMID 16113620.