Health in India
The Constitution of India makes healthcare in India the responsibility of the state governments, rather than the central federal government. It makes every state responsible for "raising the level of nutrition and the standard of living of its people and the improvement of public health as among its primary duties".[1][2]
The National Health Policy was endorsed by the Parliament of India in 1983 and updated in 2002 and then in 2017. The recent four main updates in 2017 mentions the need to focus on the growing burden of the non-communicable diseases, on the emergence of the robust healthcare industry, on growing incidences of catastrophic expenditure due to health care costs and on rising economic growth enabling enhanced fiscal capacity.[1]
India's population, as per census 2011 stood at 1.21 billion (0.62 billion males and 0.588 females).[3] There are great inequalities in health between states. The infant mortality in Kerala is 6 per thousand live births,[4] but in Uttar Pradesh it is 64.[5] According to World Bank, the total expenditure on health care as a proportion of GDP in 2015 was 3.89%.[6] Out of 3.89%, the governmental health expenditure as a proportion of GDP is just 1%[7] and the out-of-pocket expenditure as a proportion of the current health expenditure was 65.06% in 2015.[8]
Major health indicators
Life expectancy at birth
The life expectancy at birth has increased from 49.7 years in 1970-1975 to 67.9 years in 2010-2014. For the same period, the life expectancy for females is 69.6 years and 66.4 years for males.[3] In 2018, the life expectancy at birth is said to be 69.1 years.[9]
Infant mortality rate (IMR)
The infant mortality rate has declined from 74 per 1,000 live births in 1994 to 37 per 1,000 live births in 2015. However, the differentials of rural (41) and urban (25) as of 2015 are still high.[3] In 2016, the infant mortality rate was estimated to be 34.6 per 1,000 live births.[9]
Under 5 mortality rate (U5MR)
The under five mortality rate for the country was 113 per 1,000 live births in 1994 whereas in 2018 it reduced to 41.1 per 1,000 live births.[9]
Maternal mortality ratio (MMR)
The maternal mortality ratio has declined from 212 per 100 000 live births in 2007-2009 to 167 per 100 000 live births in 2011-2013. However, the differentials for state Kerala (61) and Assam (300) as of 2011-2013 are still high.[3] In 2013, the maternal mortality ratio was estimated to be 190 per 100 000 live births.[9]
Total fertility rate (TFR)
The total fertility rate for the country was 2.3 in rural areas whereas it has been 1.8 in urban areas during 2015.[3]
Disability adjusted life years (DALYs)
The most common cause of disability adjusted life years lost for Indian citizens as of 2016 for all ages and sexes was ischemic heart disease (accounting for 8.66% of total DALYs ), 2nd chronic obstructive pulmonary disease (accounting for 4.81% of total DALYs), 3rd diarrhea (accounting for 4.64% of total DALYs) and 4th lower respiratory infections (accounting for 4.35% of total DALYs).[10]
As per the figures about the child mortality rate which is quite a big hurdle for the government, the 2nd most common cause of DALYs lost for children under 5 years of age was diseases like diarrhea, lower respiratory tract infections and other communicable diseases (accounting for 22,598.71 DALYs per 100 000 population) as of 2016 which can be preventable.[10]
Health issues
Malnutrition
Malnutrition refers to deficiencies, excesses or imbalances in a person’s intake of energy and/or nutrients. The term malnutrition covers 2 broad groups of conditions. One is undernutrition - which includes stunting (low height for age), wasting (low weight for height), underweight (low weight for age) and micronutrient deficiencies or insufficiencies (a lack of important vitamins and minerals). The other is overweight - overweight, obesity and diet-related noncommunicable diseases (such as heart disease, stroke, diabetes and cancer).[11]
According to a 2005 report, 60% of India’s children below the age of three were malnourished, which was greater than the statistics of sub-Saharan African of 28%.[12] World Bank data indicates that India has one of the world’s highest demographics of children suffering from malnutrition – said to be double that of sub-Saharan Africa with dire consequences. India’s Global Hunger Index India ranking of 67, the 80 nations with the worst hunger situation places it even below North Korea or Sudan. 44% of children under the age of 5 are underweight, while 72% of infants have anemia.[13] It is considered that one in every three malnourished children in the world lives in India.
States where malnutrition is prominent:[13]
- Uttar Pradesh: Most children here, in India's densest state by population, under the age of 5 are stunted due to malnutrition.
- Tamil Nadu: The state, despite high education, has a prominent child malnutrition problem. A National Family Health Survey reveals that 23% of children here are underweight, while 25% of Chennai children show moderately stunted growth.
- Madhya Pradesh: 2015 data reveals that Madhya Pradesh has India's highest number of malnourished children - 74.1% of them under 6 suffer from anemia, and 60% have to deal with malnutrition.
- Jharkhand and Bihar: At 56.5%, Jharkhand has India's second highest number of malnourished children. This is followed by Bihar, at 55.9%.
Forms of malnutrition
- Protein–energy malnutrition (PEM): also known as protein-calorie malnutrition
- Iron-deficiency: nutritional anemia which can lead to lessened productivity, sometimes becoming terminal
- Vitamin A deficiency: which can lead to blindness or a weakened immune system
- Iodine deficiency: which can lead to serious mental or physical complaints
- Vitamin B complex deficiency: can lead to insufficient birth weight or congenital anomalies such as spina bifida.[14][15]
Child malnutrition
| Condition | Prevalence % |
|---|---|
| Low birth weight | 22 |
| Kwashiorkor/Marasmus# | <1 |
| Bitot’s spots# | 0.8-1.0 |
| Iron deficiency anaemia (6–59 months) | 70.0 |
| Underweight (weight for age)* (<5 years)# | 42.6 |
| Stunting (height for age)* (<5 years)# | 48.0 |
| Wasting (weight for height)*# | 20.0 |
| Childhood overweight/obesity | 6-30 |
* : <Median -2SD of WHO Child Growth Standards
# : NNMB Rural Survey - 2005-06
A well-nourished child is one whose weight and height measurements compare very well within the standard normal distribution of heights and weights of healthy children of same age and sex.[16] A child without sufficient nutrients in its daily intake is not only exposed to physical and motor growth delays, but also to heightened risk of mortality, reduced immune defenses and decreased cognitive and learning capacities. Malnutrition limits the productivity of all those who are its victims, and thus serves to perpetuate poverty. As with serious malnutrition, growth delays also hinder a child’s intellectual development. Sick children with chronic malnutrition, especially when accompanied by anemia, often suffer from a lower learning capacity during the crucial first years of attending school.[14]
Malnutrition in adults
| Condition | Unit | Males | Females | ||||
|---|---|---|---|---|---|---|---|
| Urban | Rural# | Tribal^ | Urban | Rural# | Tribal^ | ||
| Chronic energy deficiency (BMI <18.5) | % | 33.2 | 40.0 | 36.0 | 49.0 | ||
| Anaemia in women (including pregnant women) | % | 75 | |||||
| Iodine deficiency - Goitre | millions | 54 | |||||
| Iodine deficiency - Cretinism | millions | 2.2 | |||||
| Iodine deficiency – Still births (includes neo-natal deaths) | 90,000 | ||||||
| Obesity related chronic diseases (BMI >25) | % | 36.0 | 7.8 | 2.4 | 40.0 | 10.9 | 3.2 |
| Hypertension | % | 35.0 | 25.0 | 25.0 | 35.0 | 24.0 | 23.0 |
| Diabetes mellitus (year 2006) | % | 16.0 | 5.0 | 16 | 5.0 | ||
| Coronary heart disease | % | 7–9 | 3–5 | 7–9 | 3–5 | ||
| Cancer incidence rate | per million | 113 | 123 | ||||
* : <Median -2SD of WHO Child Growth Standards
# : NNMB Rural Survey - 2005-06
^ : NNMB Tribal Survey - 2008-09
Due to their lower social status, girls are far more at risk of malnutrition than boys of their age. Partly as a result of this cultural bias, up to one third of all adult women in India are underweight. Inadequate care of these women already underdeveloped, especially during pregnancy, leads them in turn to deliver underweight babies who are vulnerable to further malnutrition and disease.[17]
Communicable diseases
Diseases such as dengue fever, hepatitis, tuberculosis, malaria and pneumonia continue to plague India due to increased resistance to drugs.[18]

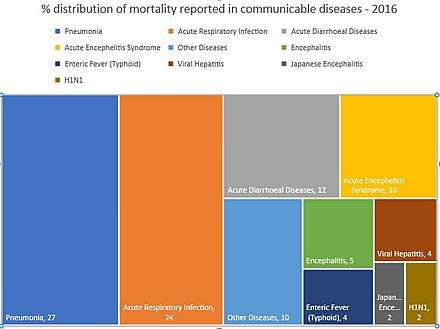
In 2011, India developed a 'totally drug-resistant' form of tuberculosis.[19] HIV/AIDS in India is ranked third highest among countries with HIV-infected patients. National AIDS Control Organisation, a government apex body is making efforts for managing the HIV/AIDS epidemic in India.[20] Diarrheal diseases are the primary causes of early childhood mortality.[21] These diseases can be attributed to poor sanitation and inadequate safe drinking water.[22] India has the world's highest incidence of rabies. Malaria has been a seasonal health problem in India from a very long time. The maximum number of malaria cases and deaths have been reported mostly form the rural parts of Orissa. The overall prevalence of the disease has diminished in 2012 and 2013 however there is a slight increase in 2014 and again started decreasing from 2015. Kala-azar is the second largest parasitic killer in the world. Most of the cases (76%) were found in Bihar in 2016. Dengue and chikungunya transmitted by Aedes mosquitoes, is another problem of concern in India. Dengue outbreaks have continued since the 1950s but severity of disease has increased in the last two decades. In 2016, India reported a total of 58,264 cases of chikungunya. Chicken pox cases were reported to be 61,118 & deaths to be 60 in 2016.[3]
In 2012, India was polio-free for the first time in its history.[23] This was achieved because of the Pulse Polio programme started in 1995–96 by the government.[24]
Non- Communicable Diseases (NCDs)
India has witnessed huge progress in the health status of its population after its independence. During this period the transition have been seen in economic development, nutritional status, fertility and mortality rates and consequently, the disease profile has changed considerably. Although great efforts have been done to control the communicable diseases, but they still contribute significantly to disease burden of the country. Decline in DALYs and deaths from communicable diseases have been accompanied by a gradual shift to, and accelerated rise in the prevalence of chronic non-communicable diseases (NCDs) such as cardiovascular disease (CVD), diabetes, chronic obstructive pulmonary disease (COPD), cancers, mental health disorders and injuries.[3]. Indians are at particularly high risk for atherosclerosis and coronary artery disease. This may be attributed to a genetic predisposition to metabolic syndrome and adverse changes in coronary artery vasodilation. NGOs such as the Indian Heart Association was created to raise awareness.[25].
Poor sanitation
As there are more than 122 million households that have no toilets, and 33% lack access to latrines, over 50% of the population (638 million) defecate in the open.(2008 estimate)[26] This is relatively higher than Bangladesh and Brazil (7%) and China (4%).[26] Although 211 million people gained access to improved sanitation from 1990–2008, only 31% use the facilities provided.[26] Only 11% of Indian rural families dispose of stools safely whereas 80% of the population leave their stools in the open or throw them in the garbage.[26] Open air defecation leads to the spread of disease and malnutrition through parasitic and bacterial infections.[27]
Safe drinking water
Several million more suffer from multiple episodes of diarrhea and still others fall ill on account of Hepatitis A, enteric fever, intestinal worms and eye and skin infections caused by poor hygiene and unsafe drinking water.[28]
Access to protected sources of drinking water has improved from 68% of the population in 1990 to 88% in 2008.[26] However, only 26% of the slum population has access to safe drinking water,[27] and 25% of the total population has drinking water on their premises.[26] This problem is exacerbated by falling levels of groundwater caused mainly by increasing extraction for irrigation.[26] Insufficient maintenance of the environment around water sources, groundwater pollution, excessive arsenic and fluoride in drinking water pose a major threat to India's health.[26]
High infant mortality rate
Despite health improvements over the last thirty years, lives continue to be lost to early childhood diseases, inadequate newborn care and childbirth-related causes. More than two million children die every year from preventable infections.[29]
Approximately 1.72 million children die each year before turning one.[30] The under five mortality and infant mortality rates have been declining, from 202 and 190 deaths per thousand live births respectively in 1970 to 64 and 50 deaths per thousand live births respectively in 2009 and to 41.1 (in 2018) and 34.6 (in 2016) deaths per thousand live births respectively.[30][31][9] However, this decline is slowing. Reduced funding for immunization leaves only 43.5% of the young fully immunized.[32] A study conducted by the Future Health Systems Consortium in Murshidabad, West Bengal indicates that barriers to immunization coverage are adverse geographic location, absent or inadequately trained health workers and low perceived need for immunization.[33] Infrastructure like hospitals, roads, water and sanitation are lacking in rural areas.[34] Shortages of healthcare providers, poor intrapartum and newborn care, diarrheal diseases and acute respiratory infections also contribute to the high infant mortality rate.[30]
Female health issues
Maternal deaths are similarly high. The reasons for this high mortality are that few women have access to skilled birth attendants and fewer still to quality emergency obstetric care. In addition, only 15 per cent of mothers receive complete antenatal care and only 58 per cent receive iron or folate tablets or syrup.[29] Women's health in India involves numerous issues. Some of them include the following:
- Malnutrition : The main cause of female malnutrition in India is the tradition requiring women to eat last, even during pregnancy and when they are lactating.[35]
- Breast Cancer : One of the most severe and increasing problems among women in India, resulting in higher mortality rates.
- Maternal Mortality : Indian maternal mortality rates in rural areas are one of the highest in the world.[35]
Rural health
Rural India contains over 68% of India's total population,[36] and half of all residents of rural areas live below the poverty line, struggling for better and easy access to health care and services.[37] Health issues confronted by rural people are many and diverse – from severe malaria to uncontrolled diabetes, from a badly infected wound to cancer.[38] Postpartum maternal illness is a serious problem in resource-poor settings and contributes to maternal mortality, particularly in rural India.[39] A study conducted in 2009 found that 43.9% of mothers reported they experienced postpartum illnesses six weeks after delivery.[40] Furthermore, because of limited government resources, much of the health care provided comes from non profits such as The MINDS Foundation.[41]
Twelfth Five Year Plan
Strategy
The Twelfth Five Year plan covering 2012-2017[42] was formulated based on the recommendation of a High Level Experts Group (HLEG) and other stakeholder consultations. The long term objective of this strategy is to establish a system of Universal Health Coverage (UHC) in the country. Key points include:
- Substantial expansion and strengthening of public sector health care system, freeing the vulnerable population from dependence on high cost and often unreachable private sector health care system.
- Health sector expenditure by central government and state government, both plan and non-plan, will have to be substantially increased by the twelfth five-year plan. It was increased from 0.94 per cent of GDP in tenth plan to 1.04 per cent in eleventh plan. The provision of clean drinking water and sanitation as one of the principal factors in control of diseases is well established from the history of industrialized countries and it should have high priority in health related resource allocation. The expenditure on health should increased to 2.5 per cent of GDP by the end of Twelfth Five Year Plan.
- Financial and managerial system will be redesigned to ensure efficient utilization of available resources and achieve better health outcome. Coordinated delivery of services within and across sectors, delegation matched with accountability, fostering a spirit of innovation are some of the measures proposed.
- Increasing the cooperation between private and public sector health care providers to achieve health goals. This will include contracting in of services for gap filling, and various forms of effectively regulated and managed Public-Private Partnership, while also ensuring that there is no compromise in terms of standards of delivery and that the incentive structure does not undermine health care objectives.
- The present Rashtriya Swasthya Bima Yojana (RSBY) which provides cash less in-patient treatment through an insurance based system should be reformed to enable access to a continuum of comprehensive primary, secondary and tertiary care. In twelfth plan period entire Below Poverty Line (BPL) population will be covered through RSBY scheme. In planning health care structure for the future, it is desirable to move from a 'fee-for-service' mechanism, to address the issue of fragmentation of services that works to the detriment of preventive and primary care and also to reduce the scope of fraud and induced demand.
- In order to increase the availability of skilled human resources, a large expansion of medical schools, nursing colleges, and so on, is therefore is necessary and public sector medical schools must play a major role in the process. Special effort will be made to expand medical education in states which are under-served. In addition, a massive effort will be made to recruit and train paramedical and community level health workers.
- The multiplicity of Central sector or Centrally Sponsored Schemes has constrained the flexibility of states to make need based plans or deploy their resources in the most efficient manner. The way forward is to focus on strengthening the pillars of the health system, so that it can prevent, detect and manage each of the unique challenges that different parts of the country face.
- A series of prescription drugs reforms, promotion of essential, generic medicine and making these universally available free of cost to all patients in public facilities as a part of the Essential Health Package will be a priority.
- Effective regulation in medical practice, public health, food and drugs is essential to safeguard people against risks and unethical practices. This is especially so given the information gaps in the health sector which make it difficult for individual to make reasoned choices.
- The health system in the Twelfth Plan will continue to have a mix of public and private service providers. The public sector health services need to be strengthened to deliver both public health related and clinical services. The public and private sectors also need to coordinate for the delivery of a continuum of care. A strong regulatory system would supervise the quality of services delivered. Standard treatment guidelines should form the basis of clinical care across public and private sectors, with the adequate monitoring by the regulatory bodies to improve the quality and control the cost of care,
Criticism

The High Level Expert Group report recommends an increase in public expenditure on health from 1.58 per cent of GDP currently to 2.1 per cent of GDP by the end of the 12th five-year plan. However, even this is far lower than the global median of 5 per cent.[43] The lack of extensive and adequately funded public health services pushes large numbers of people to incur heavy out of pocket expenditures on services purchased from the private sector. Out of pocket expenditures arise even in public sector hospitals, since lack of medicines means that patients have to buy them. This results in a very high financial burden on families in case of severe illness.[44] Though, the 12th plan document express concern over high out-of-pocket (OOP) expenditure, it does not give any target or time frame for reducing this expense . OOP can be reduced only by increasing public expenditure on health and by setting up widespread public health service providers.[45] But the planning commission is planning to do this by regulating private health care providers. It takes solace from the HLEG report which admits that, "the transformation of India’s health system to become an effective platform for UHC is an evolutionary process that will span several years".[46]
Instead of developing a better public health system with enhanced health budget, 12th five-year plan document plans to hand over health care system to private institutions. The 12th plan document causes concern over Rashtriya Swasthya Bhima Yojana being used as a medium to hand over public funds to the private sector through an insurance route. This has also incentivised unnecessary treatment which in due course will increase costs and premiums. There have been complaints about high transaction cost for this scheme due to insurance intermediaries. RSBY does not take into consideration state specific variation in disease profiles and health needs. Even though these things are acknowledged in the report, no alternative remedy is given. There is no reference to nutrition as key component of health and for universal Public Distribution System (PDS) in the plan document or HLEG recommendation. In the section of National Rural Health Mission (NRHM) in the document, the commitment to provide 30- to 50-bed Community Health Centres (CHC) per 100 000 population is missing from the main text. It was easy for the government to recruit poor women as ASHA (Accredited Social Health Activist) workers but it has failed to bring doctors, nurses and specialist in this area. The ASHA workers who are coming from a poor background are given incentive based on performance. These people lose many days job undertaking their task as ASHA worker which is not incentivised properly. Even the 12th plan doesn't give any solace.[45] To summarize, successive administrative and political reforms have conveniently bypassed training citizens and local bodies to actively participate in healthcare. In a situation where people are not enabled to identify poor quality, speak up and debate. There is dire need for the health system to fill that role on behalf of the people and can be easily done by decentralization of healthcare governance.
A recent study pointed out that access to advanced medical facilities under a single roof was the main reason for the choice of private hospitals in both rural and urban areas. The second major reason for private healthcare preference was proximity of the facility in the rural area and approachability and friendly conduct of doctors and staff in the urban centers.[47]
Initiatives[48]
Preventive and Promotive Healthcare
Programmes for Communicable Diseases
- National Viral Hepatitis Control Program (NVHCP)
- Integrated Disease Surveillance Programme(IDSP)
- Revised National Tuberculosis Control Programme(RNTCP)
- National Leprosy Eradication Programme(NLEP)
- National Vector Borne Disease Control Programme
- National AIDS Control Programme(NACP)
- Pulse Polio Programme
Programmes for Non-communicable Diseases
- National Tobacco Control Programme(NTCP)
- National Programme for Prevention and Control of Cancer, Diabetes, Cardiovascular Diseases & Stroke (NPCDCS)
- National Programme for Control Treatment of Occupational Diseases
- National Programme for Prevention and Control of Deafness (NPPCD)
- National Mental Health Programme
- National Programme for Control of Blindness
National Nutritional Programmes
- Integrated Child Development Services (ICDS)
- National Iodine Deficiency Disorders Control Programme
- Mid-Day Meal Programme
Programmes Related to System Strengthening / Welfare
- Ayushman Bharat Yojana
- National Program of Health Care for the Elderly (NPHCE)
- Reproductive, Maternal, Newborn, Child and Adolescent Health (RMNCH+A)
- National Rural Health Mission (NRHM)
- National Urban Health Mission (NUHM)
Miscellaneous
- Voluntary Blood Donation Programme
- Universal Immunization Programme (UIP)
- Pradhan Mantri Swasthya Suraksha Yojana (PMSSY)
- Janani Shishu Suraksha Yojana (JSSK)
- Rashtriya Kishor Swasthya Karyakram(RKSK)
See also
References
- 1 2 http://cdsco.nic.in/writereaddata/National-Health-Policy.pdf
- ↑ Jugal Kishore (2005). National health programs of India: national policies & legislations related to health. Century Publications. ISBN 978-81-88132-13-3. Retrieved 2 September 2012.
- 1 2 3 4 5 6 7 National Health Profile 2017. Central Bureau of Health Intelligence.
- ↑ National Family Health Survey - 4, State Fact Sheet - Kerala.
- ↑ National Family Health Survey - 4, State fact sheet - Uttar Pardesh.
- ↑ "Health expenditure, total (% of GDP)". World Bank. Retrieved 1 April 2015.
- ↑ "Domestic general government health expenditure (% of GDP)". World Bank.
- ↑ "Out-of-pocket expenditure (% of current health expenditure)". World Bank.
- 1 2 3 4 5 Rosling. "Gapminder".
- 1 2 "Global Burden of Diseases".
- ↑ "WHO - Malnutrition". WHO.
- ↑ Rieff, David (11 October 2009). "India's Malnutrition Dilemma". Source: The New York Times 2009. Retrieved 2011-09-20.
- 1 2 "Malnutrition in India Statistics State Wise". Save the Children.
- 1 2 "Child malnutrition". Archived from the original on 7 September 2014.
- 1 2 3 http://ninindia.org/DietaryGuidelinesforNINwebsite.pdf Dietary Guidelines for NIN
- ↑ "Factors affecting prevalence of malnutrition among children under three year of age in Botswana" (PDF). line feed character in
|title=at position 51 (help) - ↑ (http://www.unicef.org/india/children_4259.htm)
- ↑ "Dengue". Source: Centers for Disease Control and Prevention US. Retrieved 2011-09-20.
- ↑ Goldwert, Lindsay. "‘Totally drug-resistant’ tuberculosis reported in India; 12 patients have not responded to TB medication." New York Daily News 16 January 2012.
- ↑ "HIV/AIDS". Source: UNICEF India. Retrieved 2011-09-20.
- ↑ "Life Expectancy and Mortality in India". Source: The Prajnopaya Foundation. Retrieved 2011-09-20.
- ↑ "Health Conditions". Source: US Library of Congress. Retrieved 2011-09-20.
- ↑ "India marks one year since last polio case." Al Jazeera, 13 January 2012.
- ↑ http://india.gov.in/spotlight/spotlight_archive.php?id=90
- ↑ "Indian Heart Association".
- 1 2 3 4 5 6 7 8 "Water, Environment and Sanitation". Source: UNICEF India. Retrieved 2011-09-20.
- 1 2 "Initiatives: Hygiene and Sanitation". Source: Sangam Unity in Action. Archived from the original on 21 December 2012. Retrieved 20 September 2011.
- ↑ "What We Do – UNICEF".
- 1 2 "FAQs – UNICEF".
- 1 2 3 "Childhood Mortality and Health in India" (PDF). Source: Institute of Economic Growth University of Delhi Enclave North Campus India by Suresh Sharma. Archived from the original (PDF) on 2 April 2012. Retrieved 2011-09-20.
- ↑ "Maternal & Child Mortality and Total Fertility Rates" (PDF). Retrieved 2012-02-13.
- ↑ Robinson, Simon (1 May 2008). "India's Medical Emergency". Source: Time US. Retrieved 2011-09-20.
- ↑ Kanjilal, Barun; Debjani Barman; Swadhin Mondal; Sneha Singh; Moumita Mukherjee; Arnab Mandal; Nilanjan Bhor (September 2008). "Barriers to access immunisation services: a study in Murshidabad, West Bengal". FHS Research Brief (3).
- ↑ "Medical and Healthcare Facility Plagued". Source: Abhinandan S, Dr Ramadoss. Retrieved 2011-09-20.
- 1 2 "Chronic hunger and the status of women in India". Archived from the original on 10 September 2014.
- ↑ "RURAL URBAN DISTRIBUTION OF POPULATION" (PDF).
- ↑ Urban Rural Population of India. Indiafacts.in. Retrieved on 2012-07-17.
- ↑ JSS – The Bitter Truth About Rural Health Archived 25 April 2012 at the Wayback Machine.. Jssbilaspur.org. Retrieved on 2012-07-17.
- ↑ Sutherland, T; DM Bishai (2008). "Cost-Effectiveness Of Misoprostol And Prenatal Iron Supplementation As Maternal Mortality Interventions In Home Births In Rural India". Int J of Gynecology and Obstetrics. Retrieved 26 May 2012.
- ↑ Tuddenham, S A; et al. (February 2010). "Care seeking for postpartum morbidities in Murshidabad, rural India". Int J of Gynecology and Obstetrics. 109 (3): 245–246. doi:10.1016/j.ijgo.2010.01.016. Retrieved 26 May 2012.
- ↑ "What We Do: Our Purpose". The MINDS Foundation. Retrieved 29 July 2014.
- ↑ http://12thplan.gov.in/
- ↑ http://www.thehindu.com/business/where-the-outlook-is-healthy/article3589038.ece Retrieved from The Hindu on 27 July 2013
- ↑ "Archived copy" (PDF). Archived from the original (PDF) on 13 May 2013. Retrieved 26 July 2013. Retrieved from Planning commission site on 27 July 2013
- 1 2 T. K. Rajalakshmi. "Private leaning". Frontline.
- ↑ http://planningcommission.nic.in/reports/genrep/UHC_ExecSummary.pdf Retrieved from Planning Commission website on 27 July 2013.
- ↑ Reporter, Staff; Reporter, Staff (2017-06-07). "Friendly service, modern facilities draw people to private healthcare centres". The Hindu. ISSN 0971-751X. Retrieved 2017-10-01.
- ↑ "Ministry of Health and Family Welfare - India".

External links
- The State of the World's Midwifery – India Country Profile
- Lancet -India: Towards Universal Health Coverage
- Indian Healthcare Industry, November 2012 – Dinodia Capital Advisors