Klebsiella pneumonia
| Klebsiella pneumonia | |
|---|---|
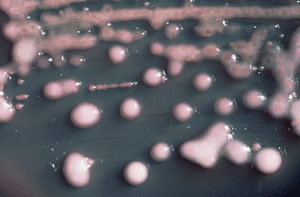 | |
| K. pneumoniae on a MacConkey agar plate. | |
| Specialty |
Pulmonology |
| Causes | Klebsiella pneumonia(bacteria)[1] |
| Diagnostic method | CBC, Sputum(culture][1][2] |
| Treatment | Antibiotics[3][4] |
Klebsiella pneumonia (KP) is a form of bacterial pneumonia associated with Klebsiella pneumoniae.[5][1] It is typically due to aspiration and alcoholism may be a risk factor, though it is also commonly implicated in hospital-acquired urinary tract infections, and COPD (chronic obstructive pulmonary disease) individuals[2][3]
Signs and symptoms
Individuals with Klebsiella pneumonia tend to cough up a characteristic sputum, as well as having fever, nausea, tachycardia and vomiting. Klebsiella pneumonia tends to affect people with underlying conditions, such as alcoholism.[2]
Cause
The cause of the condition Klebsiella pneumonia is Klebsiella pneumoniae which is gram-negative, as well as rod-shaped, glucose-fermenting, facultative anaerobic bacterium.[6][7][8]
Pathophysiology
In terms of the pathophysiology of Klebsiella pneumonia we see neutrophil myeloperoxidase defense against K P.Oxidative inactivation of elastase is involved, while LBP helps transfer bacteria cell wall elements to the cells.[1][9]
Resistant strains

Klebsiella resistant strains have been recorded in USA with a roughly threefold increase in Chicago cases,[10] quarantined individuals in Israel,[11] United Kingdom and parts of Europe, possible ground zero, or location of emergence, is the India-Pakistan border.[12]
A strain known as Carbapenem-Resistant Klebsiella pneumonia (CRKP)[13] was estimated to be involved in 350 cases in Los Angeles county between June and December 2010.[14]
Diagnosis
In terms of the diagnosis of Klebsiella pneumonia the following can be done to determine if the individual has this infection, including susceptibility testing for (ESBL) Extended Spectrum β-Lactamase, as well as:[1][2]
- CBC
- Sputum(culture]
- Radiography(chest)
- CT scan
Treatment
Treatment for Klebsiella pneumonia is by antibiotics such as aminoglycosides and cephalosporins, the choice depending upon the person’s health condition, medical history and severity of the disease.[3][4]


Klebsiella possesses beta-lactamase giving it resistance to ampicillin, many strains have acquired an extended-spectrum beta-lactamase with additional resistance to carbenicillin, amoxicillin, and ceftazidime. The bacteria remain susceptible to aminoglycosides and cephalosporins, varying degrees of inhibition of the beta-lactamase with clavulanic acid have been reported. Infections due to multidrug-resistant gram-negative pathogens in the ICU have invoked the re-emergence of colistin. However, colistin-resistant strains of K. pneumoniae have been reported in ICUs.[1][15][16][17] In 2009, strains of K. pneumoniae with gene called New Delhi metallo-beta-lactamase ( NDM-1) that even gives resistance against intravenous antibiotic carbapenem, were discovered in India and Pakistan.Klebsiella cases in Taiwan have shown abnormal toxicity, causing liver abscesses in people with diabetes mellitus (DM), treatment consists of third generation cephalosporins.
History
Community-acquired pneumonia caused by Klebsiella pneumoniae may be called Friedländer's bacillus, after Carl Friedländer, a German pathologist and microbiologist [18]
See also
References
- 1 2 3 4 5 6 Klebsiella Infections at eMedicine
- 1 2 3 4 "Aspiration Pneumonia Symptoms. Treatment and Information | Patient". Patient. Retrieved 13 January 2017.
- 1 2 3 "Klebsiella species – GOV.UK". www.gov.uk. Retrieved 13 January 2017.
- 1 2 Wilson WC, Grande CM, Hoyt DB (2007). Trauma critical care. New York: Informa Healthcare. p. 444. ISBN 978-1-4200-1684-0. Retrieved 13 January 2017.
- ↑ Dorland's Dictionary of Medical Acronyms and Abbreviations (7th ed.). Elsevier Health Sciences. 2016. p. 233. ISBN 978-0-323-44254-1. Retrieved 14 January 2017.
- ↑ Williamson MA, Snyder LM (2014). Wallach's Interpretation of Diagnostic Tests: Pathways to Arriving at a Clinical Diagnosis. Lippincott Williams & Wilkins. ISBN 978-1-4698-8741-8. Retrieved 14 January 2017. Google books page number not offered
- ↑ Procop GW, Pritt B (2014). Pathology of Infectious Diseases: A Volume in the Series: Foundations in Diagnostic Pathology. Elsevier Health Sciences. p. 257. ISBN 978-1-4557-5384-0.
- ↑ "Klebsiella". MeSH. NCBI. Retrieved 14 January 2017.
- ↑ Li B, Zhao Y, Liu C, Chen Z, Zhou D (2014). "Molecular pathogenesis of Klebsiella pneumoniae". Future Microbiology. 9 (9): 1071–81. doi:10.2217/fmb.14.48. PMID 25340836.
- ↑ Bigongiari J (October 26, 2010). "Chicago sees drug-resistant bacteria spreading". VaccineNewsDaily.com.
- ↑ Siegel-Itzcovich J (26 October 2010). "Israelis hospitalized in India to be checked for 'bugs'". The Jerusalem Post.
- ↑ Ogundipe S (October 25, 2010). "New 'superbug' scare emerges from India, Pakistan". Vanguard.
- ↑ Petrosillo N, Giannella M, Lewis R, Viale P (2013). "Treatment of carbapenem-resistant Klebsiella pneumoniae: the state of the art". Expert Review of Anti-infective Therapy. 11 (2): 159–77. doi:10.1586/eri.12.162. PMID 23409822.
- ↑ Moisse K (March 25, 2011). "Deadly Antibiotic-Resistant Superbug Spreads in Southern California". ABC News.
- ↑ Sanchez GV, Master RN, Clark RB, Fyyaz M, Duvvuri P, Ekta G, Bordon J (January 2013). "Klebsiella pneumoniae antimicrobial drug resistance, United States, 1998–2010". Emerging Infectious Diseases. 19 (1): 133–6. doi:10.3201/eid1901.120310. PMC 3557979. PMID 23260464.
- ↑ Antoniadou A, Kontopidou F, Poulakou G, Koratzanis E, Galani I, Papadomichelakis E, Kopterides P, Souli M, Armaganidis A, Giamarellou H (April 2007). "Colistin-resistant isolates of Klebsiella pneumoniae emerging in intensive care unit patients: first report of a multiclonal cluster". The Journal of Antimicrobial Chemotherapy. 59 (4): 786–90. doi:10.1093/jac/dkl562. PMID 17307769.
- ↑ "Klebsiella pneumoniae in Healthcare Settings". Centers for Disease Control and Prevention. Retrieved 13 January 2017.
- ↑ Zander DS, Farver CF (2016). Pulmonary Pathology: A Volume in Foundations in Diagnostic Pathology Series. Elsevier Health Sciences. p. 169. ISBN 978-0-323-46119-1. Retrieved 14 January 2017.
Further reading
- Hirsch EB, Tam VH (June 2010). "Detection and treatment options for Klebsiella pneumoniae carbapenemases (KPCs): an emerging cause of multidrug-resistant infection". The Journal of Antimicrobial Chemotherapy. 65 (6): 1119–25. doi:10.1093/jac/dkq108. PMID 20378670.
External links
| Classification | |
|---|---|
| External resources |