Vibrio vulnificus
| Vibrio vulnificus | |
|---|---|
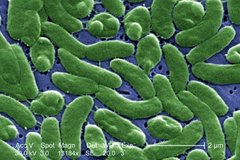 | |
| False-color SEM image of Vibrio vulnificus | |
| Scientific classification | |
| Kingdom: | Bacteria |
| Phylum: | Proteobacteria |
| Class: | Gammaproteobacteria |
| Order: | Vibrionales |
| Family: | Vibrionaceae |
| Genus: | Vibrio |
| Species: | V. vulnificus |
| Binomial name | |
| Vibrio vulnificus | |
| Synonyms | |
|
Beneckea vulnifica | |
Vibrio vulnificus is a species of Gram-negative, motile, curved rod-shaped (bacillus), pathogenic bacteria of the genus Vibrio. Present in marine environments such as estuaries, brackish ponds, or coastal areas, V. vulnificus is related to V. cholerae, the causative agent of cholera.[3][4]
Infection with V. vulnificus leads to rapidly expanding cellulitis or septicemia.[5]:279 It was first isolated as a source of disease in 1976.[6] The capsule, made of polysaccharides, is thought to protect against phagocytosis. The observed association of the infection with liver disease (associated with increased serum iron) might be due to the capability of more virulent strains to capture iron bound to transferrin.[7]
Signs and symptoms
V. vulnificus is an extremely virulent bacterium that can cause three types of infections:
- Acute gastroenteritis from eating raw or undercooked shellfish: V. vulnificus causes an infection often incurred after eating seafood, especially raw or undercooked oysters. It does not alter the appearance, taste, or odor of oysters.[8] Symptoms include vomiting, diarrhea, and abdominal pain.
- Necrotizing wound infections can occur in injured skin exposed to contaminated marine water. V. vulnificus bacteria can enter the body through open wounds when swimming or wading in infected waters,[4] or by puncture wounds from the spines of fish such as stingrays. People may develop a blistering dermatitis sometimes mistaken for pemphigus or pemphigoid.
- Invasive septicemia can occur after eating raw or undercooked shellfish, especially oysters. V. vulnificus is 80 times more likely to spread into the bloodstream in people with compromised immune systems, especially those with chronic liver disease. When this happens, severe symptoms including blistering skin lesions and septic shock can sometimes lead to death.[9][10] This severe infection may occur regardless of whether the infection began from contaminated food or an open wound.[10]
Among healthy people, ingestion of V. vulnificus can cause vomiting, diarrhea, and abdominal pain. In someone with a compromised immune system, particularly those with chronic liver disease, it can infect the bloodstream, causing a severe and life-threatening illness characterized by fever and chills, decreased blood pressure (septic shock), and blistering skin lesions.
Treatment
V. vulnificus wound infections have a mortality rate around 25%. In people in whom the infection worsens into septicemia, typically following ingestion, the mortality rate rises to 50%. The majority of these people die within the first 48 hours of infection. The optimal treatment is not known, but in one retrospective study of 93 people in Taiwan, use of a third-generation cephalosporin and a tetracycline (e.g., ceftriaxone and doxycycline, respectively) was associated with an improved outcome.[11] Prospective clinical trials are needed to confirm this finding, but in vitro data support the supposition that this combination is synergistic against V. vulnificus. Likewise, the American Medical Association and the Centers for Disease Control and Prevention (CDC) recommend treating the person with a quinolone or intravenous doxycycline with ceftazidime. The first successful documented treatment of fulminant V. vulnificus sepsis was in 1995. Treatment was Fortaz and intravenous (IV) Cipro and IV doxycycline, which proved successful. Prevention of secondary infections from respiratory failure and acute renal failure is crucial. Key to the diagnosis and treatment were the early recognition of bullae in an immunocompromised person with liver cirrhosis and oyster ingestion within the previous 48 hours, and the request by the physician for STAT Gram staining and blood cultures for V. vulnificus.[12]
V. vulnificus often causes large, disfiguring ulcers that require extensive debridement or even amputation.
Prognosis
The worst prognosis is in those people arriving at hospital in a state of shock. Total mortality in treated people (ingestion and wound) is around 33%.[11]
People especially vulnerable are those with liver disease (especially cirrhosis and hepatitis) or immunocompromised states (some kinds of cancer, bone marrow suppression, HIV, diabetes, etc.). With these cases, V. vulnificus usually enters the bloodstream, where it may cause fever and chills, septic shock (with sharply decreased blood pressure), and blistering skin lesions.[13] About half of those who contract blood infections die.
V. vulnificus infections also disproportionately affect males; 85% of those developing endotoxic shock from the bacteria are male. Females having had an oophorectomy experienced increased mortality rates, as estrogen has been shown experimentally to have a protective effect against V. vulnificus.[14]
Epidemiology
V. vulnificus is commonly found in the Gulf of Mexico, where more than a dozen people have died from the infection since 1990.[15] Most deaths at that time were occurring due to fulminant sepsis, either in the area of oyster harvest and ingestion, or in tourists returning home. Lack of disease recognition, and also of the risk factors, presentation, and cause, were and are major obstacles to good outcome and recovery.
After the successful treatment of the first person, the Florida Department of Health was able to trace the origin of the outbreak to Apalachicola Bay oysters and their harvesting in water prone to excessive growth of the organism. This contamination was due to warmth of the water and change in freshwater dilution because of a change in flow of the Chattahoochee River into the Apalachicola River, and in turn into Apalachicola Bay. A similar situation occurred after Hurricane Katrina in New Orleans.
History
The pathogen was first isolated in 1976 from a series of blood culture samples submitted to the CDC in Atlanta.[6] It was described as a "lactose-positive vibrio".[6] It was subsequently given the name Beneckea vulnifica,[1] and finally Vibrio vulnificus by Farmer in 1979.[2]
Increasing seasonal temperatures and decreasing coastal salinity levels seem to favor a greater concentration of Vibrio within filter-feeding shellfish of the US Atlantic seaboard and the Gulf of Mexico, especially oysters (Crassostrea virginica). Scientists have frequently demonstrated the presence of V. vulnificus in the gut of oysters and other shellfish and in the intestines of fish that inhabit oyster reefs. The vast majority of people who develop sepsis from V. vulnificus became ill after they ate raw oysters; most of these cases have been men.[16]
In 2005, health officials clearly identified strains of V. vulnificus infections among evacuees from New Orleans due to the flooding there caused by Hurricane Katrina.[17]
In 2015 in Florida, eight cases of V. vulnificus infection with two resulting in death were reported.[18]
Natural transformation
Natural transformation is a bacterial adaptation for DNA transfer between individual cells. V. vulnificus was found to become naturally transformable during growth on chitin in the form of crab shells.[19] The ability to now carry out transformation experiments in the laboratory should facilitate molecular genetic analysis of this opportunistic pathogen.
References
- 1 2 Reichelt JL, Baumann P, Baumann L (October 1976). "Study of genetic relationships among marine species of the genera Beneckea and Photobacterium by means of in vitro DNA/DNA hybridization". Arch. Microbiol. 110 (1): 101–20. doi:10.1007/bf00416975. PMID 1015934.
- 1 2 Farmer JJ (October 1979). "Vibrio ("Beneckea") vulnificus, the bacterium associated with sepsis, septicaemia, and the sea". Lancet. 314 (8148): 903. doi:10.1016/S0140-6736(79)92715-6. PMID 90993.
- ↑ Oliver JD, Kaper J (2001). Vibrio species. pp. 263-300 In: Food Microbiology: Fundamentals and Frontiers. (Doyle MP et al., editors) (2nd ed.). ASM Press. ISBN 1-55581-117-5.
- 1 2 Oliver JD (2005). "Wound infections caused by Vibrio vulnificus and other marine bacteria". Epidemiol Infect. 133 (3): 383–91. doi:10.1017/S0950268805003894. PMC 2870261. PMID 15962544.
- ↑ James, William D.; Berger, Timothy G. (2006). Andrews' Diseases of the Skin: Clinical Dermatology. Saunders Elsevier. ISBN 0-7216-2921-0.
- 1 2 3 Hollis DG, Weaver RE, Baker CN, Thornsberry C (April 1976). "Halophilic Vibrio species isolated from blood cultures" (PDF). J. Clin. Microbiol. 3 (4): 425–31. PMC 274318. PMID 1262454.
- ↑ Oxford handbook of Infect Dis and Microbiol, 2009
- ↑ "Vibrio Species Causing Vibriosis". Centers for Disease Control. Retrieved June 5, 2017.
- ↑ "Vibrio vulnificus". NCBI Genome Project. Retrieved 2005-09-01.
- 1 2 "Vibrio Species Causing Vibriosis - Questions and Answers". Centers for Disease Control. Retrieved June 5, 2017.
- 1 2 Liu JW, Lee IK, Tang HJ, et al. (2006). "Prognostic factors and antibiotics in Vibrio vulnificus septicemia". Archives of Internal Medicine. 166 (19): 2117&ndash, 23. doi:10.1001/archinte.166.19.2117. PMID 17060542.
- ↑ "Vibrio vulnificus fact sheet" (PDF). issc.org. Archived from the original (PDF) on 21 July 2016. Retrieved August 1, 2016.
- ↑ Oliver JD, Kaper J (2005). Vibrio vulnificus. In: Oceans and Health: Pathogens in the Marine Environment. (Belken SS, Colwell RR, editors) (2nd ed.). Springer Science. ISBN 0-387-23708-9.
- ↑ Merkel SM, Alexander S, Zufall E, Oliver JD, Huet-Hudson YM (2001). "Essential Role for Estrogen in Protection against Vibrio vulnificus-Induced Endotoxic Shock". Infection and Immunity. 69 (10): 6119–22. doi:10.1128/IAI.69.10.6119-6122.2001. PMC 98741. PMID 11553550.
- ↑ Flynn, Dan (November 22, 2011). "Still Too Many Raw Oyster Deaths in Gulf States". Food Safety News. Retrieved August 1, 2016.
- ↑ Diaz, James H. (May 2014). "Skin and Soft Tissue Infections Following Marine Injuries and Exposures in Travelers". Journal of Travel Medicine. 21 (3): 207–213. doi:10.1111/jtm.12115. ISSN 1195-1982. PMID 24628985.
- ↑ Gold, Scott (September 6, 2005). "Newest Peril from Flooding Is Disease". Los Angeles Times.
- ↑ Katy Galimberti (June 18, 2015). "Flesh-Eating Bacteria Kills Two in Florida as Water Temperatures Rise". msn.com. Retrieved August 1, 2016.
- ↑ Gulig PA, Tucker MS, Thiaville PC, Joseph JL, Brown RN (2009). "USER friendly cloning coupled with chitin-based natural transformation enables rapid mutagenesis of Vibrio vulnificus". Appl. Environ. Microbiol. 75 (15): 4936–49. doi:10.1128/AEM.02564-08. PMC 2725515. PMID 19502446.