Lymphadenopathy
| Lymphadenopathy | |
|---|---|
| Synonyms | Adenopathy |
|
| |
| Neck lymphadenopathy associated with infectious mononucleosis | |
| Classification and external resources | |
| Specialty | Infectious disease |
| ICD-10 | I88, L04, R59.1 |
| ICD-9-CM | 289.1-289.3, 683, 785.6 |
| DiseasesDB | 22225 |
| MedlinePlus | 001301 |
| eMedicine | ped/1333 |
| MeSH | D008206 |
Lymphadenopathy or adenopathy is disease of the lymph nodes, in which they are abnormal in size, number, or consistency.[1] Lymphadenopathy of an inflammatory type (the most common type) is lymphadenitis,[2] producing swollen or enlarged lymph nodes. In clinical practice, the distinction between lymphadenopathy and lymphadenitis is rarely made and the words are usually treated as synonymous. Inflammation of the lymphatic vessels is known as lymphangitis.[3] Infectious lymphadenitides affecting lymph nodes in the neck are often called scrofula.
The term comes from the word lymph and a combination of the Greek words αδένας, adenas ("gland") and παθεία, patheia ("act of suffering" or "disease").
Lymphadenopathy is a common and nonspecific sign. Common causes include infections (from minor ones such as the common cold to serious ones such as HIV/AIDS), autoimmune diseases, and cancers. Lymphadenopathy is also frequently idiopathic and self-limiting.
Classification
Lymphadenopathy may be classified by:
- Size, where lymphadenopathy in adults is often defined as a short axis of one or more lymph nodes is greater than 10mm.[4]
- By extent:
- Localized lymphadenopathy: due to localized spot of infection e.g., an infected spot on the scalp will cause lymph nodes in the neck on that same side to swell up
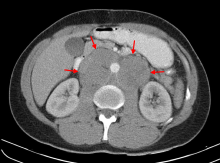
- Generalized lymphadenopathy: due to a systemic infection of the body e.g., influenza or secondary syphilis
- Persistent generalized lymphadenopathy (PGL): persisting for a long time, possibly without an apparent cause
- By localization:
- Dermatopathic lymphadenopathy: lymphadenopathy associated with skin disease.
- By malignancy: Benign lymphadenopathy is distinguished from malignant causes which mainly refer to lymphomas or lymph node metastasis
Size


- By size, where lymphadenopathy in adults is often defined as a short axis of one or more lymph nodes is greater than 10mm.[4][5] However, there is regional variation as detailed in this table:
| Generally | 10 mm[4][5] |
| Inguinal | 10[6] – 20 mm[7] |
| Pelvis | 10 mm for ovoid lymph nodes, 8 mm for rounded[6] |
| Neck | |
|---|---|
| Generally (non-retropharyngeal) | 10 mm[6][8] |
| Jugulodigastric lymph nodes | 11mm[6] or 15 mm[8] |
| Retropharyngeal | 8 mm[8]
|
| Mediastinum | |
| Mediastinum, generally | 10 mm[6] |
| Superior mediastinum and high paratracheal | 7mm[9] |
| Low paratracheal and subcarinal | 11 mm[9] |
| Upper abdominal | |
| Retrocrural space | 6 mm[10] |
| Paracardiac | 8 mm[10] |
| Gastrohepatic ligament | 8 mm[10] |
| Upper paraaortic region | 9 mm[10] |
| Portacaval space | 10 mm[10] |
| Porta hepatis | 7 mm[10] |
| Lower paraaortic region | 11 mm[10] |
Lymphadenopathy of the axillary lymph nodes can be defined as solid nodes measuring more than 15 mm without fatty hilum.[11] Axillary lymph nodes may be normal up to 30 mm if consisting largely of fat.[11]
- In children, a short axis of 8 mm can be used.[12] However, inguinal lymph nodes of up to 15 mm and cervical lymph nodes of up to 20 mm are generally normal in children up to age 8–12.[13]
Lymphadenopathy of more than 1.5 cm - 2 cm increases the risk of cancer or granulomatous disease as the cause rather than only inflammation or infection. Still, an increasing size and persistence over time are more indicative of cancer.[14]
Causes
Lymph node enlargement is recognized as a common sign of infectious, autoimmune, or malignant disease. Examples may include:
- Reactive: acute infection (e.g., bacterial, or viral), or chronic infections (tuberculous lymphadenitis,[15] cat-scratch disease[16]).
- The most distinctive sign of bubonic plague is extreme swelling of one or more lymph nodes that bulge out of the skin as "buboes." The buboes often become necrotic and may even rupture.[17]
- Infectious mononucleosis is an acute viral infection usually caused by Epstein-Barr virus and may be characterized by a marked enlargement of the cervical lymph nodes.[18]
- It is also a sign of cutaneous anthrax[19] and Human African trypanosomiasis[20]
- Toxoplasmosis, a parasitic disease, gives a generalized lymphadenopathy (Piringer-Kuchinka lymphadenopathy).[21]
- Plasma cell variant of Castleman's disease - associated with HHV-8 infection and HIV infection[22][23]
- Mesenteric lymphadenitis after viral systemic infection (particularly in the GALT in the appendix) can commonly present like appendicitis.[24][25]
Less common infectious causes of lymphadenopathy may include bacterial infections such as cat scratch disease, tularemia, brucellosis, or prevotella.
- Tumoral:
- Primary: Hodgkin lymphoma[26] and non-Hodgkin lymphoma give lymphadenopathy in all or a few lymph nodes.[21]
- Secondary: metastasis, Virchow's Node, neuroblastoma,[27] and chronic lymphocytic leukemia.[28]
- Autoimmune: systemic lupus erythematosus[29] and rheumatoid arthritis may have a generalized lymphadenopathy.[21]
- Immunocompromised: AIDS. Generalized lymphadenopathy is an early sign of infection with human immunodeficiency virus (HIV), the virus that causes acquired immunodeficiency syndrome (AIDS).[30] "Lymphadenopathy syndrome" has been used to describe the first symptomatic stage of HIV progression, preceding a diagnosis of AIDS.
- Bites from certain venomous snakes such as the pit viper[31]
- Unknown: Kikuchi disease,[32] progressive transformation of germinal centers, sarcoidosis, hyaline-vascular variant of Castleman's disease, Rosai-Dorfman disease,[33] Kawasaki disease,[34] Kimura disease[35]
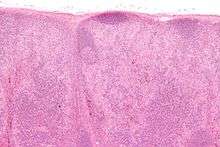
Benign (reactive) lymphadenopathy
Benign lymphadenopathy is a common biopsy finding, and may often be confused with malignant lymphoma. It may be separated into major morphologic patterns, each with its own differential diagnosis with certain types of lymphoma. Most cases of reactive follicular hyperplasia are easy to diagnose, but some cases may be confused with follicular lymphoma. There are seven distinct patterns of benign lymphadenopathy:[18]
- Follicular hyperplasia: This is the most common type of reactive lymphadenopathy.[18]
- Paracortical hyperplasia/Interfollicular hyperplasia: It is seen in viral infections, skin diseases, and nonspecific reactions.
- Sinus histiocytosis: It is seen in lymph nodes draining limbs, inflammatory lesions, and malignancies.
- Nodal extensive necrosis
- Nodal granulomatous inflammation
- Nodal extensive fibrosis (Connective tissue framework)
- Nodal deposition of interstitial substance
These morphological patterns are never pure. Thus, reactive follicular hyperplasia can have a component of paracortical hyperplasia. However, this distinction is important for the differential diagnosis of the cause.
Diagnosis
In cervical lymphadenopathy, it is routine to perform a throat examination including mirror and/or endoscopy.[36]
On ultrasound, B-mode imaging depicts lymph node morphology, whilst power Doppler can assess the vascular pattern.[37] B-mode imaging features that can distinguish metastasis and lymphoma include size, shape, calcification, loss of hilar architecture, as well as intranodal necrosis.[37] Soft tissue edema and nodal matting on B-mode imaging suggests tuberculous cervical lymphadenitis or previous radiation therapy.[37] Serial monitoring of nodal size and vascularity are useful in assessing treatment response.[37]
Fine needle aspiration cytology (FNAC) has a sensitivity and specificity percentages of 81% and 100%, respectively, in the histopathology of malignant cervical lymphadenopathy.[36] PET-CT has proven to be helpful in identifying occult primary carcinomas of the head and neck, especially when applied as a guiding tool prior to panendoscopy, and may induce treatment related clinical decisions in up to 60% of cases.[36]
See also
References
- ↑ King, D; Ramachandra, J; Yeomanson, D (2 January 2014). "Lymphadenopathy in children: refer or reassure?". Archives of Disease in Childhood: Education and Practice Edition. 99: 101–110. doi:10.1136/archdischild-2013-304443. PMID 24385291.
- ↑ "lymphadenitis" at Dorland's Medical Dictionary
- ↑ "lymphangitis" at Dorland's Medical Dictionary
- 1 2 3 Ganeshalingam, Skandadas; Koh, Dow-Mu (2009). "Nodal staging". Cancer Imaging. 9 (1). doi:10.1102/1470-7330.2009.0017. ISSN 1470-7330.
- 1 2 Schmidt Júnior, Aurelino Fernandes; Rodrigues, Olavo Ribeiro; Matheus, Roberto Storte; Kim, Jorge Du Ub; Jatene, Fábio Biscegli (2007). "Distribuição, tamanho e número dos linfonodos mediastinais: definições por meio de estudo anatômico". Jornal Brasileiro de Pneumologia. 33 (2): 134–140. doi:10.1590/S1806-37132007000200006. ISSN 1806-3713.
- 1 2 3 4 5 6 Torabi M, Aquino SL, Harisinghani MG (September 2004). "Current concepts in lymph node imaging". Journal of Nuclear Medicine. 45 (9): 1509–18. PMID 15347718.
- ↑ "Assessment of lymphadenopathy". BMJ Best Practice. Retrieved 2017-03-04. Last updated: Last updated: Feb 16, 2017
- 1 2 3 Page 432 in: Luca Saba (2016). Image Principles, Neck, and the Brain. CRC Press. ISBN 9781482216202.
- 1 2 Sharma, Amita; Fidias, Panos; Hayman, L. Anne; Loomis, Susanne L.; Taber, Katherine H.; Aquino, Suzanne L. (2004). "Patterns of Lymphadenopathy in Thoracic Malignancies". RadioGraphics. 24 (2): 419–434. doi:10.1148/rg.242035075. ISSN 0271-5333.
- 1 2 3 4 5 6 7 Dorfman, R E; Alpern, M B; Gross, B H; Sandler, M A (1991). "Upper abdominal lymph nodes: criteria for normal size determined with CT". Radiology. 180 (2): 319–322. doi:10.1148/radiology.180.2.2068292. ISSN 0033-8419.
- 1 2 Page 559 in: Wolfgang Dähnert (2011). Radiology Review Manual. Lippincott Williams & Wilkins. ISBN 9781609139438.
- ↑ Page 942 in: Richard M. Gore, Marc S. Levine (2010). High Yield Imaging Gastrointestinal HIGH YIELD in Radiology. Elsevier Health Sciences. ISBN 9781455711444.
- ↑ Laurence Knott. "Generalised Lymphadenopathy". Patient UK. Retrieved 2017-03-04. Last checked: 24 March 2014
- ↑ Bazemore AW, Smucker DR (December 2002). "Lymphadenopathy and malignancy". American Family Physician. 66 (11): 2103–10. PMID 12484692.
- ↑ Fontanilla, JM; Barnes, A; Von Reyn, CF (September 2011). "Current diagnosis and management of peripheral tuberculous lymphadenitis". Clinical Infectious Diseases. 53 (6): 555–562. doi:10.1093/cid/cir454. PMID 21865192.
- ↑ Klotz, SA; Ianas, V; Elliott, SP (2011). "Cat-scratch Disease". American Family Physician. 83 (2): 152–155. PMID 21243990.
- ↑ Butler, T (2009). "Plague into the 21st century". Clinical Infectious Diseases. 49 (5): 736–742. doi:10.1086/604718. PMID 19606935.
- 1 2 3 Weiss, LM; O'Malley, D (2013). "Benign lymphadenopathies". Modern Pathology. 26 (Supplement 1): S88–S96. doi:10.1038/modpathol.2012.176. PMID 23281438.
- ↑ Sweeney, DA; Hicks, CW; Cui, X; Li, Y; Eichacker, PQ (December 2011). "Anthrax infection". American Journal of Respiratory and Critical Care Medicine. 184 (12): 1333–1341. doi:10.1164/rccm.201102-0209CI. PMC 3361358. PMID 21852539.
- ↑ Kennedy, PG (February 2013). "Clinical features, diagnosis, and treatment of human African trypanosomiasis (sleeping sickness)". Lancet Neurology. 12 (2): 186–194. doi:10.1016/S1474-4422(12)70296-X. PMID 23260189.
- 1 2 3 Status and anamnesis, Anders Albinsson. Page 12
- ↑ Kim, TU; Kim, S; Lee, JW; Lee, NK; Jeon, UB; Ha, HG; Shin, DH (September–October 2012). "Plasma cell type of Castleman's disease involving renal parenchyma and sinus with cardiac tamponade: case report and literature review". Korean Journal of Radiology. 13 (5): 658–663. doi:10.3348/kjr.2012.13.5.658. PMC 3435867. PMID 22977337.
- ↑ Zhang, H; Wang, R; Wang, H; Xu, Y; Chen, J (June 2012). "Membranoproliferative glomerulonephritis in Castleman's disease: a systematic review of the literature and 2 case reports". Internal Medicine (Tokyo, Japan). 51 (12): 1537–1542. doi:10.2169/internalmedicine.51.6298. PMID 22728487.
- ↑ Bratucu, E; Lazar, A; Marincaş, M; Daha, C; Zurac, S (March–April 2013). "Aseptic mesenteric lymph node abscesses. In search of an answer. A new entity?" (PDF). Chirurgia (Bucarest, Romania: 1990). 108 (2): 152–160. PMID 23618562.
- ↑ Leung, A; Sigalet, DL (June 2003). "Acute Abdominal Pain in Children". American Family Physician. 67 (11): 2321–2327.
- ↑ Glass, C (September 2008). "Role of the Primary Care Physician in Hodgkin Lymphoma". American Family Physician. 78 (5): 615–622. PMID 18788239.
- ↑ Colon, NC; Chung, DH (2011). "Neuroblastoma". Advances in Pediatrics. 58 (1): 297–311. doi:10.1016/j.yapd.2011.03.011. PMC 3668791. PMID 21736987.
- ↑ Sagatys, EM; Zhang, L (January 2011). "Clinical and laboratory prognostic indicators in chronic lymphocytic leukemia". Cancer Control. 19 (1): 18–25. PMID 22143059.
- ↑ Melikoglu, MA; Melikoglu, M (October–December 2008). "The clinical importance of lymphadenopathy in systemic lupus erythematosus" (PDF). Acta Reumatologia Portuguesa. 33 (4): 402–406. PMID 19107085.
- ↑ Lederman, MM; Margolis, L (June 2008). "The lymph node in HIV pathogenesis". Seminars in Immunology. 20 (3): 187–195. doi:10.1016/j.smim.2008.06.001. PMC 2577760. PMID 18620868.
- ↑ Quan, D (October 2012). "North American poisonous bites and stings". Critical Care Clinics. 28 (4): 633–659. doi:10.1016/j.ccc.2012.07.010. PMID 22998994.
- ↑ Komagamine, T; Nagashima, T; Kojima, M; Kokubun, N; Nakamura, T; Hashimoto, K; Kimoto, K; Hirata, K (September 2012). "Recurrent aseptic meningitis in association with Kikuchi-Fujimoto disease: case report and literature review". BMC Neurology. 12: 187–195. doi:10.1186/1471-2377-12-112. PMC 3570427. PMID 23020225.
- ↑ Noguchi, S; Yatera, K; Shimajiri, S; Inoue, N; Nagata, S; Nishida, C; Kawanami, T; Ishimoto, H; Sasaguri, Y; Mukae, H (2012). "Intrathoracic Rosai-Dorfman disease with spontaneous remission: a clinical report and a review of the literature". The Tohoku Journal of Experimental Medicine. 227 (3): 231–235. doi:10.1620/tjem.227.231. PMID 22789970.
- ↑ Weiss, PF (April 2012). "Pediatric vasculitis". Pediatric Clinics of North America. 59 (2): 407–423. doi:10.1016/j.pcl.2012.03.013. PMC 3348547. PMID 22560577.
- ↑ Koh, H; Kamiishi, N; Chiyotani, A; Takahashi, H; Sudo, A; Masuda, Y; Shinden, S; Tajima, A; Kimura, Y; Kimura, T (April 2012). "Eosinophilic lung disease complicated by Kimura's disease: a case report and literature review". Internal Medicine (Tokyo, Japan). 51 (22): 3163–3167. PMID 23154725.
- 1 2 3 Balm, A. J. M.; van Velthuysen, M. L. F.; Hoebers, F. J. P.; Vogel, W. V.; van den Brekel, M. W. M. (2010). "Diagnosis and Treatment of a Neck Node Swelling Suspicious for a Malignancy: An Algorithmic Approach". International Journal of Surgical Oncology. 2010: 1–8. doi:10.1155/2010/581540. ISSN 2090-1402.
- 1 2 3 4 Ahuja, A.T. (2008). "Ultrasound of malignant cervical lymph nodes". Cancer Imaging. 8 (1): 48–56. doi:10.1102/1470-7330.2008.0006. ISSN 1470-7330.
External links
- HPC:13820 on humpath.com (Digital slides)