Malakoplakia
| Malakoplakia | |
|---|---|
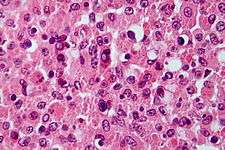 | |
| Micrograph showing the characteristic finding of malakoplakia (Michaelis–Gutmann bodies). H&E stain. |
Malakoplakia or malacoplakia (from Greek Malako "soft" + Plako "plaque") is a rare inflammatory condition which makes its presence known as a papule, plaque or ulceration that usually affects the genitourinary tract.[1]:274 However, it may also be associated with other bodily organs. It was initially described in the early 20th century as soft yellowish plaques found on the mucosa of the urinary bladder. Microscopically it is characterized by the presence of foamy histiocytes with basophilic inclusions called Michaelis–Gutmann bodies.
It usually involves gram-negative bacteria.[2]
Causes
Malakoplakia is thought to result from the insufficient killing of bacteria by macrophages. Therefore, the partially digested bacteria accumulate in macrophages and leads to a deposition of iron and calcium. The impairment of bactericidal activity manifests itself as the formation of an ulcer, plaque or papule.
Malakoplakia is associated with patients with a history of immunosuppression due to lymphoma, diabetes mellitus, renal transplantation, or because of long-term therapy with systemic corticosteroids.
Diagnosis
As malakoplakia is a condition associated with chronic cystitis, it usually presents itself as a cystitis condition. Following investigation will help in diagnosis of malakoplakia: - Urine analysis which indicates presence of bacteria and pus cells. - Urine culture - Cystoscopic evaluation confirms presence of ulcer or papule. - Biopsy to rule out other causes. - Microscopically it shows large multinucleated malakoplakia giant cells with concretions called as Michaelis Gutman bodies.
Treatment
- Catheterize the patient with full aseptic precautions. - Irrigating bladder with distilled water thrice a day with 3 way Foley's catheter. - Urinary antiseptics like pyridium which helps in relieving urinary symptoms. Should be given thrice a day for a week. - Antibiotic like Nitrofurantoin or Ciprofloxacin for prolonged time.
See also
References
- ↑ James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: clinical Dermatology. Saunders Elsevier. ISBN 0-7216-2921-0.
- ↑ Liang Cheng; David G. Bostwick (2006). Essentials of anatomic pathology. Springer. pp. 1180–. ISBN 978-1-58829-461-6. Retrieved 15 May 2010.
External links
| Classification | |
|---|---|
| External resources |