Esophagitis
| Esophagitis | |
|---|---|
| Classification and external resources | |
| Specialty | gastroenterology |
| ICD-10 | K20 |
| ICD-9-CM | 530.10 |
| DiseasesDB | 9182 |
| MedlinePlus | 001153 |
| MeSH | D004941 |
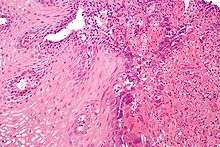
Esophagitis (or oesophagitis) is an inflammation of the esophagus. The prefix esophag/o refers to the esophagus and the suffix -itis means inflammation. The esophagus is part of the digestive system, specifically the gastrointestinal tract. It is a muscular tube where food passes through from the mouth to the stomach.[1] Esophagitis is a disease that can be painful and can make swallowing difficult. However, esophagitis can be asymptomatic.[1] Infection, irritation, and/or inflammation of the lining of the esophagus can cause esophagitis. The most common cause of esophagitis is gastroesophageal reflux disease (GERD).[2] There additionally are several types of esophagitis, some not correlated with GERD.
Mechanism
The esophagus is a muscular tube made of both voluntary and involuntary muscles. It is responsible for peristalsis of food. It is about 8 inches long and passes through the diaphragm before entering the stomach. The esophagus is made up of four different layers: serosa, muscularis externa, submucosa, and the mucosa. The mucosa, the inner most layer and lining of the esophagus, is composed of stratified squamous epithelium, lamina propria, and muscularis mucosae. At the end of the esophagus is the lower esophageal sphincter, which prevents stomach acid from moving to the esophagus. Sometimes the sphincter allows acid to backflow into the esophagus if it is not strong enough. Esophagitis occurs when either an infection or irritation to the layers of the esophagus is present. Infection can be caused by bacteria, viruses, fungi, or diseases that weaken the immune system.[3] Irritation can be caused by GERD, vomiting, surgery, medications, hernias, and radiation injury.[3] Inflammation can cause the esophagus to narrow, which makes swallowing food difficult and may result in food bolus impaction. Irritation from the backflow of acid can cause the feeling of burning in the chest and can result in the flow of acid into the throat causing acid reflux or regurgitation. If irritation, infection, and/or inflammation to the esophagus continues, it is likely that the symptoms and signs will increase.
Symptoms
The signs and symptoms for esophagitis include:[2]
- Heartburn feels like the inside of your chest is burning. It is a symptom of acid reflux or GERD.
- Nausea is the feeling of being sick, specifically with the urge to vomit.
- Swallowing is painful and difficult to pass food through your esophagus.
- Vomiting, also known as emesis, is the release of the contents of the stomach through the mouth or nose.
- Abdominal pain is when pain is felt in the abdomen.
- Food bolus impaction is an obstruction of the esophagus by swallowed food.
- Acid regurgitation is the backflow of acid from the stomach to the mouth.
- Chest pain is pain felt between the neck and upper abdomen. There are many causes and the pain can range.
- Cough is a reflex to clear the throat of irritants or mucus.
A doctor should be consulted if the signs and/or symptoms do not subside after a few days, are accompanied with flu-like symptoms, do not lessen after treating with over-the counter antacids, and/or make eating food difficult.[1]
Diagnosis
A gastroenterologist is a medical professional that can diagnose esophagitis. To diagnose esophagitis, the doctor will interview the patient regarding their signs and symptoms. If the doctor suspects esophagitis, tests can be ordered. Esophagitis can be diagnosed by an upper endoscopy, biopsy, upper GI series (or barium swallow), and laboratory tests.[3]
An upper endoscopy is a procedure to look at the esophagus by using an endoscope. While looking at the esophagus, the doctor is able to take a small biopsy. The biopsy can be used to confirm inflammation of the esophagus.
An upper GI series uses a barium contrast, fluoroscopy, and an X-ray. During a barium X-ray, a solution with barium or pill is taken before getting an X-ray. The barium makes the organs more visible and can detect if there is any narrowing, inflammation, or other abnormalities that can be causing the disease. The upper GI series can be used to find the cause of GI symptoms. An esophagram is if only the throat and esophagus are looked at.[4]
Laboratory tests can be done on biopsies removed from the esophagus and can help determine the cause of the esophagitis. Laboratory tests can help diagnose a fungal, viral, or bacterial infection. Scanning for white blood cells can help diagnose eosinophil esophagitis.
Some lifestyle indicators for this disease include: stress, unhealthy eating, smoking, drinking, family history, allergies, and an immunodeficiency. It is important for the doctor to review the patient's medical history before diagnosing with esophagitis. Specific subtypes and other causes should be taken into account when making the final diagnosis.
Subtypes of esophagitis
Reflux esophagitis
For decades it has been assumed that inflammation from acid reflux was caused by the irritation of acid itself. A recent study, however, points toward a cause and effect relationship that is less clear, and demonstrated that inflammation may not be caused by acid reflux, but that both reflux and inflammation could be caused by an underlying third factor. It is a common misconception that reflux has been proven to cause inflammation in the esophagus.[5]
Infectious esophagitis
Esophagitis that happens due to a viral, fungal, parasitic or bacterial infection. More likely to happen to people who have an immunodeficiency. Types include:
Fungal
Viral
Drug-induced esophagitis
Damage to the esophagus due to medications. If the esophagus is not coated or if the medicine is not taken with enough liquid, it can damage the tissues.
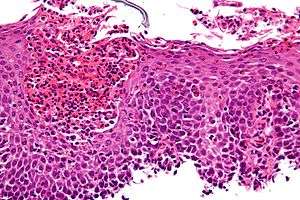
Eosinophilic esophagitis
This esophagitis is caused by a high concentration of eosinophils in the esophagus. The presence of eosinophils in the esophagus may be due to an allergen, and is often correlated with GERD. The direction of cause and effect between inflammation and acid reflux is poorly established, with recent studies (in 2016) hinting that reflux does not cause inflammation.[5] This esophagitis can be triggered by allergies to food or to inhaled allergens. This type is still poorly understood.
Lymphocytic esophagitis
Lymphocytic esophagitis is when there is an increased amount of lymphocytes in the lining of the esophagus.[1] It is a rare condition. It could be connected to eosinophilic esophagitis.
Caustic esophagitis
Caustic esophagitis is the damage of tissue via chemical origin. This occasionally occurs through occupational exposure (via breathing of fumes that mix into the saliva which is then swallowed) or through pica. It occurred in some teenagers during the fad of intentionally eating Tide pods.
Grading of severity
The severity of reflux esophagitis is commonly classified into four grades according to the Los Angeles Classification:[6][7]
| Grade A | One or more mucosal breaks < 5 mm in maximal length |
| Grade B | One or more mucosal breaks > 5mm, but without continuity across mucosal folds |
| Grade C | Mucosal breaks continuous between > 2 mucosal folds, but involving less than 75% of the esophageal circumference |
| Grade D | Mucosal breaks involving more than 75% of esophageal circumference |
Causes and prevention
Causes
Esophagitis cannot be spread. However, infections can be spread by those who have infectious esophagitis. Esophagitis can develop due to many causes. GERD is the most common cause of esophagitis because of the backflow of acid from the stomach, which can irritate the lining of the esophagus.
Other causes include:
- Medicines – Can cause esophageal damage that can lead to esophageal ulcers
- Nonsteroidal anti-inflammatory drugs (NSAIDS) – aspirin, naproxen sodium, and ibuprofen. Known to irritate the GI tract.
- Antibiotics – doxycycline and tetracycline
- Quinidine
- Bisphosphonates – used to treat osteoporosis
- Steroids
- Potassium chloride
- Chemical injury by alkaline or acid solutions
- Physical injury resulting from nasogastric tubes.
- Alcohol abuse – Can wear down the lining of the esophagus.
- Crohn's disease – a type of IBD and an autoimmune disease that can cause esophagitis if it attacks the esophagus.
- Stress – Can cause higher levels of acid reflux
- Radiation therapy-Can affect the immune system.
- Allergies (food, inhalants) – Allergies can stimulate eosinophilic esophagitis.
- Infection-People with an immunodeficiencies have a higher chance of developing esophagitis.
- Vitamins and supplements (iron, Vitamin C, and potassium) – Supplements and minerals can be hard on the GI tract.
- Vomiting – Acid can irritate esophagus.
- Hernias – A hernia can poke through the diaphragm muscle and can inhibit the stomach acid and food from draining quickly.
- Surgery
Prevention
Since there can be many causes underlying esophagitis, it is important to try to find the cause to help to prevent esophagitis. To prevent reflux esophagitis, avoid acidic foods, caffeine, eating before going to bed, alcohol, fatty meals, and smoking. To prevent drug-induced esophagitis, drink plenty of liquids when taking medicines, take an alternative drug, and do not take medicines while lying down, before sleeping, or too many at one time. Esophagitis is more prevalent in adults and does not discriminate.
Treatment and prognosis
Treatments for esophagitis include medications to block acid production, to manage pain, and to reduce inflammation. Other treatments include antibiotics and intravenous nutrition.
To treat reflux esophagitis, over the counter antacids, medications that reduce acid production (H-2 receptor blockers), and proton pump inhibitors are recommended to help block acid production and to let the esophagus heal. Some prescription medications to treat reflux esophagitis include higher dose H-2 receptor blockers, proton pump inhibitors, and prokinetics, which help with the emptying of the stomach.
To treat eosinophilic esophagitis, avoiding any allergens that may be stimulating the eosinophils is recommended. As for medications, proton pump inhibitors and steroids can be prescribed. Steroids that are used to treat asthma can be swallowed to treat eosinophil esophagitis due to nonfood allergens. The removal of food allergens from the diet is included to help treat eosinophilic esophagitis.
For infectious esophagitis, a medicine is prescribed based on what type of infection is causing the esophagitis. These medicines are prescribed to treat bacterial, fungal, viral, and/or parasitic infections.
An endoscopy can be used to remove ill fragments. Surgery can be done to remove the damaged part of the esophagus.[3] For reflux esophagitis, a fundooplication can be done to help strengthen the lower esophageal sphincter from allowing backflow of the stomach into the esophagus. As for patients that have a narrowing esophagus, a gastroenterologist can perform a procedure to dilate the esophagus.

Some home remedies and lifestyle changes to help with esophagitis include losing weight, stop smoking, lowering stress, avoid sleeping/lying down after eating, raise your head while laying down, taking medicines correctly, avoiding certain medications, and avoiding foods that cause the reflux that might be causing the esophagitis.
If the disease remains untreated, it can cause scarring and discomfort in the esophagus. If the irritation is not allowed to heal, esophagitis can result in esophageal ulcers. Esophagitis can develop into Barrett's esophagus and can increase the risk of esophageal cancer.
The prognosis for a person with esophagitis depends on the underlying causes and conditions. If a patient has a more serious underlying cause such as a digestive system or immune system issue, it may be more difficult to treat. Normally, the prognosis would be good with no serious illnesses. If there are more causes than one, the prognosis could move to fair.
Recent research
In 2015, a treatment for reflux esophagitis was introduced. It involves a small invasive surgery to place a ring of magnetic titanium beads near the lower esophageal sphincter. It is called a magnetic sphincter augmentation device or MSAD. It was made to prevent GERD by keeping the stomach acid out of the esophagus. Before the implantation of the device, the patients in this study were taking proton pump inhibitors. The pilot study for this device resulted in a treatment that "preserves gastric anatomy" and results in "less severe side effects than traditional antireflux surgery."[8] The patient's that had these devices implanted were given a questionnaire for their GERD Health Related Quality of Life (GERD-HRQL) before implantation. Their scores improved after the five years and more than 80% discontinued their proton pump inhibitors. The normalization of esophageal pH was achieved by 70% of the patients in the study.[8] At the end of the study, there were "no reports of death, device erosions, device migrations, device malfunctions, or late-occurring device complications."[8]
The study of esophagitis has focused on reflux esophagitis over the years. However, the study of different subtypes has emerged. Researchers have started to study other causes besides acid reflux. Eosinophilic esophagitis and infectious esophagitis are subtypes that target the lining of the esophagus via infection or immune-mediated inflammatory diseases. Other causes of esophagitis are being studied such as how Crohn's disease, caustic injury, chemotherapy, and radiotherapy can have an effect on the esophagus. It is important to realize that not all upper gastrointestinal tract symptoms are due to gastric reflux and to look at the patient's clinical history before diagnosing and treating the patient. It is important to note that there can be more than one underlying cause to esophagitis.[8]
References
- 1 2 3 4 "Esophagitis – Symptoms and causes – Mayo Clinic". www.mayoclinic.org. Retrieved 2017-12-13.
- 1 2 "Esophagitis-Topic Overview". WebMD. Retrieved 2017-12-13.
- 1 2 3 4 "Understanding Esophagitis". WebMD. Retrieved 2017-11-07.
- ↑ "Upper Gastrointestinal (UGI) Series". WebMD. Retrieved 2017-12-13.
- 1 2 https://www.medscape.com/viewarticle/863413
- ↑ Farivar M. "Los Angeles Classification of Esophagitis". webgerd.com. In turn citing: Lundell LR, Dent J, Bennett JR, et al. (August 1999). "Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification". Gut. 45 (2): 172–80. doi:10.1136/gut.45.2.172. PMC 1727604. PMID 10403727.
- ↑ Laparoscopic bariatric surgery, Volume 1. William B. Inabnet, Eric J. DeMaria, Sayeed Ikramuddin. ISBN 0-7817-4874-7.
- 1 2 3 4 Saino, Greta; Bonavina, Luigi; Lipham, John C.; Dunn, Daniel; Ganz, Robert A. (2015-10-01). "Magnetic Sphincter Augmentation for Gastroesophageal Reflux at 5 Years: Final Results of a Pilot Study Show Long-Term Acid Reduction and Symptom Improvement". Journal of Laparoendoscopic & Advanced Surgical Techniques. Part A. 25 (10): 787–792. doi:10.1089/lap.2015.0394. ISSN 1092-6429. PMC 4624249. PMID 26437027.