WHO Model List of Essential Medicines
The WHO Model List of Essential Medicines (EML), published by the World Health Organization (WHO), contains the medications considered to be most effective and safe to meet the most important needs in a health system.[1] The list is frequently used by countries to help develop their own local lists of essential medicine.[1] As of 2016, more than 155 countries have created national lists of essential medicines based on the World Health Organization's model list.[2] This includes countries in both the developed and developing world.[1][3]
The list is divided into core items and complementary items.[4] The core items are deemed to be the most cost-effective options for key health problems and are usable with little additional health care resources.[4] The complementary items either require additional infrastructure such as specially trained health care providers or diagnostic equipment or have a lower cost–benefit ratio.[4] About 25% of items are in the complementary list.[5] Some medications are listed as both core and complementary.[6] While most medications on the list are available as generic products, being under patent does not preclude inclusion.[7]
The first list was published in 1977 and included 212 medications.[1][8] The WHO updates the list every two years.[9] The 14th list was published in 2005 and contained 306 medications.[10] In 2015, the 19th edition of the list was published and contains around 410 medications.[9] The 20th edition was published in 2017, and contains 433 medications.[11][12] The 21st list was published in 2019.[13][14] The national lists contain between 334 and 580 medications.[5]
A separate list for children up to 12 years of age, known as the WHO Model List of Essential Medicines for Children (EMLc), was created in 2007 and is in its 7th edition.[9][15] It was created to make sure that the needs of children were systematically considered such as availability of proper formulations.[16][17] Everything in the children's list is also included in the main list.[18] The list and notes are based on the 19th to 21st edition of the main list.[4][11][13] An α indicates a medicine is only on the complementary list.[4][13]
Anaesthetics
General anaesthetics and oxygen
Inhalational medicines
- Halothane
- Isoflurane
- Nitrous oxide
- Oxygen
Local anaesthetics
- Bupivacaine
- Lidocaine
- Lidocaine/epinephrine
- Ephedrineα (not a local anaesthetic, included in this list for prevention of low blood pressure associated with spinal anaesthesia during caesarean section)
Medicines for pain and palliative care
Nonopioids and nonsteroidal anti-inflammatory drugs (NSAIDs)
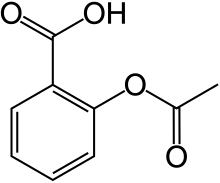
- Acetylsalicylic acid (aspirin)
- Ibuprofen
- Paracetamol[note 3] (acetaminophen)
Medicines for other common symptoms in palliative care
- Amitriptyline
- Cyclizine
- Dexamethasone
- Diazepam
- Docusate sodium
- Fluoxetine
- Haloperidol
- Hyoscine butylbromide
- Hyoscine hydrobromide
- Lactulose
- Loperamide
- Metoclopramide
- Midazolam
- Ondansetron
- Senna
Antiallergics and medicines used in anaphylaxis
- Dexamethasone
- Epinephrine (adrenaline)
- Hydrocortisone
- Loratadine[note 7]
- Prednisolone
Antidotes and other substances used in poisonings
Nonspecific
- Charcoal, activated
Specific
- Acetylcysteine
- Atropine
- Calcium gluconate
- Methylthioninium chloride (methylene blue)
- Naloxone
- Penicillamine
- Prussian blue
- Sodium nitrite
- Sodium thiosulfate
- Deferoxamineα
- Dimercaprolα
- Fomepizoleα
- Sodium calcium edetateα
- Succimerα
Anticonvulsive medication
- Carbamazepine
- Diazepam
- Lamotrigine[note 8]
- Lorazepam
- Magnesium sulfate[note 9]
- Midazolam
- Phenobarbital
- Phenytoin
- Valproic acid (sodium valproate)
- Ethosuximideα
Anti-infective medicines
Anthelminthics
Intestinal anthelminthics
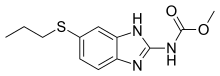
- Albendazole
- Ivermectin
- Levamisole
- Mebendazole
- Niclosamide
- Praziquantel
- Pyrantel
Antifilarials
- Albendazole
- Diethylcarbamazine
- Ivermectin
Antischistosomals and other antinematode medicines
- Praziquantel
- Triclabendazole
- Oxamniquineα[note 10]
Antibiotics
Access group
- Amikacin
- Amoxicillin
- Amoxicillin/clavulanic acid (amoxicillin + clavulanic acid)
- Ampicillin
- Benzathine benzylpenicillin
- Benzylpenicillin
- Cefalexin
- Cefazolin[note 11]
- Chloramphenicol
- Clindamycin
- Cloxacillin[note 12]
- Doxycycline
- Gentamicin
- Metronidazole
- Nitrofurantoin
- Phenoxymethylpenicillin (penicillin V)
- Procaine benzylpenicillin[note 13]
- Spectinomycin
- Sulfamethoxazole/trimethoprim[note 14]
Watch group
- Azithromycin[note 15]
- Cefixime[note 16]
- Cefotaxime[note 17]
- Ceftriaxone[note 18]
- Cefuroxime
- Ciprofloxacin
- Clarithromycin[note 19]
- Piperacillin/tazobactam
- Vancomycin
- Ceftazidimeα
- Meropenemα[note 20]
- Vancomycinα[note 21]
Reserve group
Antileprosy medicines
- Clofazimine
- Dapsone
- Rifampicin
Antituberculosis medicines

- Ethambutol
- Ethambutol/isoniazid/pyrazinamide/rifampicin (ethambutol + isoniazid + pyrazinamide + rifampicin)
- Ethambutol/isoniazid/rifampicin (ethambutol + isoniazid + rifampicin)
- Isoniazid
- Isoniazid/pyrazinamide/rifampicin (isoniazid + pyrazinamide + rifampicin)
- Isoniazid/rifampicin (isoniazid + rifampicin)
- Pyrazinamide
- Rifabutin[note 22]
- Rifampicin
- Rifapentine[note 23]
- Amikacinα
- Amoxicillin/clavulanic acidα[note 24]
- Bedaquilineα
- Clofazimineα
- Cycloserineα[note 25]
- Delamanidα
- Ethionamideα[note 26]
- Levofloxacinα[note 27]
- Linezolidα
- Meropenemα[note 28]
- Moxifloxacin
- p-aminosalicylic acidα
- Streptomycinα
Antifungal medicines
- Amphotericin B
- Clotrimazole
- Fluconazole
- Flucytosine
- Griseofulvin
- Itraconazole[note 29]
- Nystatin
- Voriconazole[note 30]
- Potassium iodideα
Antiviral medicines
Antiherpes medicines
Antiretrovirals
Nucleoside/nucleotide reverse transcriptase inhibitors
- Abacavir (ABC)
- Lamivudine (3TC)
- Tenofovir disoproxil fumarate (TDF)
- Zidovudine (ZDV or AZT)
Non-nucleoside reverse transcriptase inhibitors
- Efavirenz (EGV or EFZ)
- Nevirapine (NVP)
Protease inhibitors
200mg.jpg)
- Atazanavir
- Atazanavir/ritonavir
- Darunavir
- Lopinavir/ritonavir (LPV/r)
- Ritonavir
Integrase inhibitors
- Dolutegravir
- Raltegravir[note 31]
Fixed-dose combinations
- Abacavir/lamivudine
- Dolutegravir/lamivudine/tenofovir (dolutegravir + lamivudine + tenofovir)
- Efavirenz/emtricitabine/tenofovir[note 32]
- Efavirenz/lamivudine/tenofovir
- Emtricitabine/tenofovir[note 32][note 33]
- Lamivudine/nevirapine/zidovudine
- Lamivudine/zidovudine
Medicines for prevention of HIV-related opportunistic infections
- Isoniazid/pyridoxine/sulfamethoxazole/trimethoprim
Antihepatitis medicines
Medicines for hepatitis B
Nucleoside/Nucleotide reverse transcriptase inhibitors
- Entecavir
- Tenofovir disoproxil fumarate (TDF)
Medicines for hepatitis C
Pangenotypic direct-acting antivirals
Non-pangenotypic direct-acting antivirals
- Dasabuvir
- Ledipasvir/sofosbuvir
- Ombitasvir/paritaprevir/ritonavir
Other antivirals for hepatitis C
Antiprotozoal medicines
Antiamoebic and antigiardiasis medicines
- Diloxanide
- Metronidazole
Antileishmaniasis medicines
- Amphotericin B
- Miltefosine
- Paromomycin
- Sodium stibogluconate or meglumine antimoniate
Antimalarial medicines
For curative treatment
- Amodiaquine[note 41]
- Artemether[note 42]
- Artemether/lumefantrine[note 43]
- Artesunate[note 44]
- Artesunate/amodiaquine[note 45]
- Artesunate/mefloquine
- Artesunate/pyronaridine
- Chloroquine[note 46]
- Dihydroartemisinin/piperaquine
- Doxycycline[note 47]
- Mefloquine[note 41]
- Primaquine[note 48]
- Quinine[note 49]
- Sulfadoxine/pyrimethamine[note 50]
For prevention
- Amodiaquine + sulfadoxine/pyrimethamine
- Chloroquine[note 51]
- Doxycycline
- Mefloquine
- Proguanil[note 52]
- Sulfadoxine/pyrimethamine
Antipneumocystosis and antitoxoplasmosis medicines
- Pyrimethamine
- Sulfadiazine
- Sulfamethoxazole/trimethoprim
- Pentamidineα
Antitrypanosomal medicines
African trypanosomiasis
- Fexinidazole[note 53]
1st stage
- Pentamidine[note 54]
- Suramin sodium[note 55]
2nd stage
American trypanosomiasis
- Benznidazole
- Nifurtimox
Medicines for ectoparasitic infections
Antimigraine medicines
Acute attack
- Acetylsalicylic acid (aspirin)
- Ibuprofen
- Paracetamol (acetaminophen)
Prevention
Immunomodulators and antineoplastics
Immunomodulators for non-malignant disease
- Adalimumabα[note 58]
- Azathioprineα
- Ciclosporinα
Antineoplastics and supportive medicines
Cytotoxic medicines
- Arsenic trioxideα
- Asparaginaseα
- Bendamustineα
- Bleomycinα
- Calcium folinateα
- Capecitabineα
- Carboplatinα
- Chlorambucilα
- Cisplatinα
- Cyclophosphamideα
- Cytarabineα
- Dacarbazineα
- Dactinomycinα
- Daunorubicinα
- Docetaxelα
- Doxorubicinα
- Etoposideα
- Fludarabineα
- Fluorouracilα
- Gemcitabineα
- Hydroxycarbamideα
- Ifosfamideα
- Irinotecanα
- Melphalanα
- Mercaptopurineα
- Methotrexateα
- Oxaliplatinα
- Paclitaxelα
- Pegaspargaseα[note 59]
- Procarbazineα
- Realgar Indigo naturalis formulationα
- Tioguanineα
- Vinblastineα
- Vincristineα
- Vinorelbineα
Targeted therapies
Immunomodulators
- Filgrastimα
- Lenalidomideα
- Nivolumabα[note 61]
- Thalidomideα
Hormones and antihormones
- Abirateroneα
- Anastrozoleα
- Bicalutamideα
- Dexamethasoneα
- Hydrocortisoneα
- Leuprorelinα
- Methylprednisoloneα
- Prednisoloneα
- Tamoxifenα
Supportive medicines
- Allopurinolα
- Mesnaα
- Zoledronic acidα
Antiparkinsonism medicines
- Biperiden
- Carbidopa/levodopa (levodopa + carbidopa)
Medicines affecting the blood
Antianaemia medicines
- Ferrous salt
- Ferrous salt/folic acid
- Folic acid
- Hydroxocobalamin
- Erythropoiesis-stimulating agentsα
Medicines affecting coagulation
Blood products and plasma substitutes of human origin
Blood and blood components
- Fresh frozen plasma
- Platelet concentrates
- Packed red blood cells
- Whole blood
Plasma-derived medicines
Human immunoglobulins
- Rho(D) immune globulin (anti-D immunoglobulin)
- Anti-rabies immunoglobulin
- Anti-tetanus immunoglobulin
- Human normal immunoglobulinα
Plasma substitutes
- Dextran 70[note 65]
Cardiovascular medicines
Antianginal medicines
- Bisoprolol[note 66]
- Glyceryl trinitrate
- Isosorbide dinitrate
- Verapamil
Antiarrhythmic medicines
- Bisoprolol[note 66]
- Digoxin
- Epinephrine (adrenaline)
- Lidocaine
- Verapamil
- Amiodaroneα
Antihypertensive medicines
- Amlodipine
- Bisoprolol[note 67]
- Enalapril
- Hydralazine[note 68]
- Hydrochlorothiazide
- Lisinopril/amlodipine (lisinopril + amlodipine)
- Lisinopril/hydrochlorothiazide
- Losartan
- Methyldopa[note 69]
- Telmisartan/amlodipine (telmisartan + amlodipine)
- Telmisartan/hydrochlorothiazide
- Sodium nitroprussideα
Medicines used in heart failure
Antithrombotic medicines
Anti-platelet medicines
- Acetylsalicylic acid (aspirin)
- Clopidogrel
Lipid-lowering agents
Dermatological (topical)
Antifungal medicines
- Miconazole
- Selenium sulfide
- Sodium thiosulfate
- Terbinafine
Anti-infective medicines
- Mupirocin
- Potassium permanganate
- Silver sulfadiazine
Anti-inflammatory and antipruritic medicines
- Betamethasone
- Calamine
- Hydrocortisone
Medicines affecting skin differentiation and proliferation
- Benzoyl peroxide
- Coal tar
- Fluorouracil
- Podophyllum resin
- Salicylic acid
- Urea
Scabicides and pediculicides
- Benzyl benzoate
- Permethrin
Diagnostic agents
Ophthalmic medicines
- Fluorescein
- Tropicamide
Radiocontrast media
- Amidotrizoate
- Barium sulfate
- Iohexol
- Meglumine iotroxateα
Disinfectants and antiseptics
Antiseptics
- Chlorhexidine
- Ethanol
- Povidone iodine
Disinfectants
- Alcohol based hand rub
- Chlorine base compound
- Chloroxylenol
- Glutaral
Gastrointestinal medicines
- Pancreatic enzymesα
Antiulcer medicines
Antiemetic medicines
Anti-inflammatory medicines
- Sulfasalazine
- Hydrocortisoneα
Laxatives
- Senna
Medicines used in diarrhoea
- Co-packaged Oral rehydration salts/zinc sulfate
Oral rehydration
Medicines for diarrhea
- Zinc sulfate[note 71]
Medicines for endocrine disorders
Adrenal hormones and synthetic substitutes
- Fludrocortisone
- Hydrocortisone
Androgens
Progestogens
Medicines for diabetes
Insulins
- Insulin injection (soluble)
- Intermediate-acting insulin
Medicines for hypoglycaemia
- Glucagon
- Diazoxideα
Thyroid hormones and antithyroid medicines
- Levothyroxine
- Potassium iodide
- Methimazole[note 73]
- Propylthiouracil[note 74]
- Lugol's solutionα
Immunologicals
Diagnostic agents
- Tuberculin, purified protein derivative (PPD)
Sera and immunoglobulins
- Antivenom immunoglobulin[note 75]
- Diphtheria antitoxin
Vaccines

- BCG vaccine
- Cholera vaccine[note 76]
- Dengue vaccine[note 76]
- Diphtheria vaccine
- Haemophilus influenzae type b vaccine
- Hepatitis A vaccine[note 76]
- Hepatitis B vaccine
- HPV vaccine
- Influenza vaccine[note 77]
- Japanese encephalitis vaccine[note 78]
- Measles vaccine
- Meningococcal meningitis vaccine[note 76]
- Mumps vaccine[note 77]
- Pertussis vaccine
- Pneumococcal vaccine
- Poliomyelitis vaccine
- Rabies vaccine[note 76]
- Rotavirus vaccine
- Rubella vaccine
- Tetanus vaccine
- Tick-borne encephalitis vaccine[note 78]
- Typhoid vaccine[note 76]
- Varicella vaccine[note 77]
- Yellow fever vaccine[note 78]
Muscle relaxants (peripherally-acting) and cholinesterase inhibitors
- Atracurium
- Neostigmine
- Suxamethonium
- Vecuronium
- Pyridostigmineα
Eye preparations
Anti-infective agents
Anti-inflammatory agents
Local anesthetics
- Tetracaine
Miotics and antiglaucoma medicines
- Acetazolamide
- Latanoprost
- Pilocarpine
- Timolol
Mydriatics
- Atropine[note 80]
- Epinephrine (adrenaline)α
Anti-vascular endothelial growth factor (VEGF)
Medicines for reproductive health and perinatal care
Contraceptives
Oral hormonal contraceptives
- Ethinylestradiol/levonorgestrel
- Ethinylestradiol/norethisterone
- Levonorgestrel
- Ulipristal
Injectable hormonal contraceptives
- Estradiol cypionate/medroxyprogesterone acetate
- Medroxyprogesterone acetate
- Norethisterone enantate
Intrauterine devices
- IUD with copper
- IUD with progestogen
Barrier methods
- Condoms
- Diaphragms
Implantable contraceptives
- Etonogestrel-releasing implant
- Levonorgestrel-releasing implant
Intravaginal contraceptives
- Progesterone vaginal ring[note 81]
Uterotonics
- Carbetocin
- Ergometrine
- Mifepristone used with misoprostol[note 82]
- Misoprostol[note 83]
- Oxytocin
Antioxytocics (tocolytics)
Medicines administered to the mother
- Dexamethasone
- Tranexamic acid
Medicines administered to the neonate
- Caffeine citrate
- Chlorhexidine
- Ibuprofenα
- Prostaglandin Eα
- Prostaglandin E1
- Prostaglandin E2
- Surfactantα
Peritoneal dialysis solution
- Intraperitoneal dialysis solution (of appropriate composition)α
Medicines for mental and behavioural disorders
Medicines used in psychotic disorders
Medicines used in mood disorders
Medicines used in depressive disorders
Medicines used in bipolar disorders
- Carbamazepine
- Lithium carbonate
- Valproic acid (sodium valproate)
Medicines for anxiety disorders
Medicines used for obsessive compulsive disorders
Medicines acting on the respiratory tract
Antiasthmatics and medicines for chronic obstructive pulmonary disease
- Beclometasone
- Budesonide
- Budesonide/formoterol
- Epinephrine (adrenaline)
- Ipratropium bromide
- Salbutamol (albuterol)
- Tiotropium
Solutions correcting water, electrolyte and acid-base disturbances
Oral
- Oral rehydration salts
- Potassium chloride
Parenteral
- Glucose
- Glucose with sodium chloride
- Potassium chloride
- Sodium chloride
- Sodium hydrogen carbonate
- Sodium lactate, compound solution
Miscellaneous
- Water for injection
Vitamins and minerals
- Ascorbic acid
- Calcium
- Cholecalciferol[note 85]
- Ergocalciferol
- Iodine
- Multiple micronutrient powder
- Nicotinamide
- Pyridoxine
- Retinol
- Riboflavin
- Sodium fluoride
- Thiamine
- Calcium gluconateα
Ear, nose and throat medicines
- Acetic acid
- Budesonide
- Ciprofloxacin
- Xylometazoline
Medicines for diseases of joints
Medicines used to treat gout
Disease-modifying agents used in rheumatoid disorders
- Chloroquine
- Azathioprineα
- Hydroxychloroquineα
- Methotrexateα
- Penicillamineα
- Sulfasalazineα
Notes
An α indicates the medicine is only on the complementary list. For these items specialized diagnostic or monitoring or specialist training are needed. An item may also be listed as complementary on the basis of higher costs or a less attractive cost-benefit ratio.[4][13]
- Thiopental may be used as an alternative depending on local availability and cost.
- No more than 30% oxygen should be used to initiate resuscitation of neonates less than or equal to 32 weeks of gestation.
- Not recommended for anti‐inflammatory use due to lack of proven benefit to that effect
- For the management of cancer pain
- Alternatives limited to hydromorphone and oxycodone
- For the management of cancer pain
- There may be a role for sedating antihistamines for limited indications (EMLc).
- as adjunctive therapy for treatment-resistant partial or generalized seizures.
- For use in eclampsia and severe pre‐eclampsia and not for other convulsant disorders
- Oxamniquine is listed for use when praziquantel treatment fails.
- For surgical prophylaxis
- cloxacillin, dicloxacillin and flucloxacillin are preferred for oral administration due to better bioavailability.
- Procaine benzylpenicillin is not recommended as first-line treatment for neonatal sepsis except in settings with high neonatal mortality, when given by trained health workers in cases where hospital care is not achievable.
- single agent trimethoprim may be an alternative for lower urinary tract infection.
- Also listed for single-dose treatment of trachoma and yaws.
- Only listed for acute invasive bacterial diarrhoea (dysentery) or gonorrhoea
- Third-generation cephalosporin of choice for use in hospitalized neonates
- Do not administer with calcium and avoid in infants with hyperbilirubinemia.
- Erythromycin may be an alternative. For use in combination regimens for eradication of H. pylori in adults
- Imipenem/cilastatin is an alternative, except for acute bacterial meningitis, where meropenem is preferred
- Powder for injection:250 mg (as hydrochloride) in vial.
- For use only in patients with HIV receiving protease inhibitors
- For treatment of latent TB infection (LTBI) only
- For use only in combination with meropenem or imipenem/cilastatin
- Terizidone may be an alternative
- Prothionamide may be an alternative
- Ofloxacin and moxifloxacin may be alternatives based on availability and programme considerations.
- Imipenem/cilastatin may be an alternative
- For treatment of chronic pulmonary aspergillosis, histoplasmosis, sporotrichosis, paracoccidioidomycosis, mycoses caused by Talaromyces marneffei and chromoblastomycosis; and prophylaxis of histoplasmosis and infections caused by T. marneffei in AIDS patients
- For treatment of chronic pulmonary aspergillosis and acute invasive aspergillosis
- For use in pregnant women and in second-line regimens in accordance with WHO treatemnt guidelines.
- Emtricitabine (FTC) is an acceptable alternative to 3TC, based on knowledge of the pharmacology, the resistance patterns and clinical trials of antiretrovirals.
- Combination also indicated for pre-exposure prophylaxis
- For the treatment of viral haemorrhagic fevers
- For the treatment of cytomegalovirus retinitis (CMVr).
- For severe illness due to confirmed or suspected influenza virus infection in critically ill hospitalized patients
- When used in combination with sofosbuvir
- When used in combination with daclatasvir
- For the treatment of hepatitis C, in combination with direct acting anti-viral medicines
- To be used in combination with ribavirin
- To be used in combination with artesunate 50 mg
- For use in the management of severe malaria
- Not recommended in the first trimester of pregnancy or in children below 5 kg
- To be used in combination with either amodiaquine, mefloquine or sulfadoxine + pyrimethamine
- Other combinations that deliver the target doses required such as 153 mg or 200 mg (as hydrochloride) with 50 mg artesunate can be alternatives.
- For use only for the treatment of P. vivax infection
- For use only in combination with quinine
- Only for use to achieve radical cure of P. vivax and P. ovale infections, given for 14 days
- For use only in the management of severe malaria, and should be used in combination with doxycycline
- Only in combination with artesunate 50 mg
- For use only in Central American regions, for P. vivax infections
- For use only in combination with chloroquine
- For the treatment of 1st and 2nd stage human African trypanosomiasis due to Trypanosoma brucei gambiense infection
- To be used for the treatment of Trypanosoma brucei gambiense infection
- To be used for the treatment of the initial phase of Trypanosoma brucei rhodesiense infection
- To be used for the treatment of T. b. gambiense infection
- Only to be used in combination with eflornithine, for the treatment of T. b. gambiense infection
- Certolizumab pegol, etanercept, golimumab and infliximab are alternatives, including quality-assured biosimilars
- Including quality-assured biosimilars
- Gefitinib and afatinib are alternatives
- Pembrolizumab is an alternative
- Apixaban, edoxaban and rivaroxaban are alternatives
- Alternatives are limited to nadroparin and dalteparin
- Deferasirox oral form may be an alternative, depending on cost and availability.
- Polygeline, injectable solution, 3.5% is considered as equivalent.
- Includes metoprolol and carvedilol as alternatives
- Includes atenolol, metoprolol and carvedilol as alternatives. Atenolol should not be used as a first-line agent in uncomplicated hypertension in patients >60 years
- Hydralazine is listed for use in the acute management of severe pregnancy‐induced hypertension only. Its use in the treatment of essential hypertension is not recommended in view of the availability of more evidence of efficacy and safety of other medicines.
- Methyldopa is listed for use in the management of pregnancy‐induced hypertension only. Its use in the treatment of essential hypertension is not recommended in view of the availability of more evidence of efficacy and safety of other medicines.
- For use in high‐risk patients
- In acute diarrhoea, zinc sulfate should be used as an adjunct to oral rehydration salts
- Glibenclamide not suitable above 60 years
- Carbimazole is an alternative depending on local availability
- For use when alternative first-line treatment is not appropriate or available
- Exact type to be defined locally
- Recommended for some high-risk populations
- Recommended only for immunization programmes with certain characteristics
- Recommended for certain regions
- For infections due to Chlamydia trachomatis or Neisseria gonorrhoeae
- Or homatropine (hydrobromide) or cyclopentolate (hydrochloride)
- For use in women actively breastfeeding at least 4 times per day
- Where permitted under national law and where culturally acceptable
- For induction of labour, should only be used where appropriate facilities are available
- Buprenorphine considered to have similar clinical performance and best evidence for effectiveness and safety
- Ergocalciferol can be used as an alternative.
- For use for rheumatic fever, juvenile arthritis, Kawasaki disease
References
- "Essential medicines". World Health Organization. Retrieved 19 January 2017.
- "The WHO Essential Medicines List (EML): 30th anniversary". World Health Organization. Retrieved 26 June 2016.
- Persaud N, Jiang M, Shaikh R, Bali A, Oronsaye E, Woods H, Drozdzal G, Rajakulasingam Y, Maraj D, Wadhawan S, Umali N, Wang R, McCall M, Aronson JK, Plüddemann A, Moja L, Magrini N, Heneghan C (June 2019). "Comparison of essential medicines lists in 137 countries". Bull. World Health Organ. 97 (6): 394–404C. doi:10.2471/BLT.18.222448. hdl:10665/325509. ISSN 0042-9686. PMC 6560372. PMID 31210677.
- "19th WHO Model List of Essential Medicines" (PDF). World Health Organization. April 2015. p. Annex 1. Retrieved 17 January 2017.
- Bansal, D; Purohit, VK (January 2013). "Accessibility and use of essential medicines in health care: Current progress and challenges in India". Journal of Pharmacology & Pharmacotherapeutics. 4 (1): 13–18. doi:10.4103/0976-500X.107642. PMC 3643337. PMID 23662019.
- "The Selection and Use of Essential Medicines - WHO Technical Report Series, No. 920: 5. Reviews of sections of the Model List: 5.2 Review of core versus complementary listing of medicines". World Health Organization (WHO). 2003. Retrieved 6 March 2017.
- Beall, Reed (2016). "Patents and the WHO Model List of Essential Medicines (18th Edition): Clarifying the Debate on IP and Access" (PDF). World Intellectual Property Organization (WIPO). Retrieved 3 May 2017.
- Wirtz, VJ; Hogerzeil, HV; Gray, AL; Bigdeli, M; de Joncheere, CP; et al. (28 January 2017). "Essential medicines for universal health coverage". The Lancet. 389 (10067): 403–476. doi:10.1016/S0140-6736(16)31599-9. PMID 27832874.
- "WHO Model Lists of Essential Medicines". World Health Organization. Retrieved 17 January 2017.
- Prakash, B; Nadig, P; Nayak, A (2016). "Rational Prescription for a Dermatologist". Indian Journal of Dermatology. 61 (1): 32–38. doi:10.4103/0019-5154.174017. PMC 4763692. PMID 26955092.
- World Health Organization (2017). WHO model list of essential medicines, 20th list (March 2017, amended August 2017). Geneva. hdl:10665/273826.
- "Essential Medicines List and WHO Model Formulary". World Health Organization. Retrieved 5 May 2018.
- World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- World Health Organization (2019). Executive summary: the selection and use of essential medicines 2019: report of the 22nd WHO Expert Committee on the selection and use of essential medicines. Geneva. hdl:10665/325773. WHO/MVP/EMP/IAU/2019.05. License: CC BY-NC-SA 3.0 IGO.
- World Health Organization (2019). World Health Organization model list of essential medicines for children: 7th list 2019. Geneva. hdl:10665/325772. WHO/MVP/EMP/IAU/2019.07. License: CC BY-NC-SA 3.0 IGO.
- Rose, K; Anker, JNVd (2010). Guide to Paediatric Drug Development and Clinical Research. Karger Medical and Scientific Publishers. p. 42. ISBN 9783805593625.
- Seyberth, HW; Rane, A; Schwab, M (2011). Pediatric Clinical Pharmacology. Springer Science & Business Media. p. 358. ISBN 9783642201950.
- Kalle, H (9 February 2017). "Essential Medicines for Children". Clinical Pharmacology & Therapeutics. 101 (6): 718–720. doi:10.1002/cpt.661. PMID 28182281.
Further reading
- World Health Organization (2009). Stuart MC, Kouimtzi M, Hill SR (eds.). WHO Model Formulary 2008. hdl:10665/44053. ISBN 9789241547659.
- World Health Organization (2015). The selection and use of essential medicines. Twentieth report of the WHO Expert Committee 2015 (including 19th WHO Model List of Essential Medicines and 5th WHO Model List of Essential Medicines for Children). Geneva. hdl:10665/189763. ISBN 9789240694941. ISSN 0512-3054. WHO technical report series ; no. 994.
- World Health Organization (2017). The selection and use of essential medicines: report of the WHO Expert Committee, 2017 (including the 20th WHO Model List of Essential Medicines and the 6th Model List of Essential Medicines for Children). Geneva. hdl:10665/259481. ISBN 978-92-4-121015-7. ISSN 0512-3054. WHO technical report series ; no. 1006.
- World Health Organization (2019). The selection and use of essential medicines: report of the WHO Expert Committee on Selection and Use of Essential Medicines, 2019 (including the 21st WHO Model List of Essential Medicines and the 7th WHO Model List of Essential Medicines for Children). Geneva: World Health Organization. hdl:10665/330668. ISBN 9789241210300. ISSN 0512-3054. WHO technical report series;1021.
- World Health Organization (2019). "Additions and deletions of medicines on the WHO model lists of essential medicines: 1977-2017". hdl:10665/278038. WHO/MVP/EMP/IAU/2019.01. License: CC BY-NC-SA 3.0 IGO. Cite journal requires
|journal=(help)