Prednisolone
Prednisolone is a steroid medication used to treat certain types of allergies, inflammatory conditions, autoimmune disorders, and cancers.[2][3] Some of these conditions include adrenocortical insufficiency, high blood calcium, rheumatoid arthritis, dermatitis, eye inflammation, asthma, and multiple sclerosis.[3] It is used by mouth, injection into a vein, as a skin cream, and as eye drops.[4][5][3]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Orapred, PediaPred, Millipred, others |
| Other names | 11,17-Dihydroxy-17-(2-hydroxyacetyl)-10,13-dimethyl-6,7,8,9,10,11,12,13,14,15,16,17-dodecahydrocyclopenta[a] phenanthren-3-one |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a615042 |
| License data |
|
| Pregnancy category | |
| Routes of administration | By mouth, intravenous, topical, eye drop |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Elimination half-life | 2–3 hours |
| Excretion | urine |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.020 |
| Chemical and physical data | |
| Formula | C21H28O5 |
| Molar mass | 360.444 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
InChI
| |
| (verify) | |
Side effects with short-term use include nausea and feeling tired.[2] More severe side effects include psychiatric problems, which may occur in about 5% of people.[6] Common side effects with long term use include bone loss, weakness, yeast infections, and easy bruising.[3] While short-term use in the later part of pregnancy is safe, long-term use or use in early pregnancy is occasionally associated with harm to the baby.[1] It is a glucocorticoid made from hydrocortisone (cortisol).[7]
Prednisolone was discovered and approved for medical use in 1955.[7] It is on the World Health Organization's List of Essential Medicines, the safest and most effective medicines needed in a health system.[8] It is available as a generic medication.[3] The wholesale cost in the developing world is about US$0.01 per 5 mg tablet.[9] In 2017, it was the 129th most commonly prescribed medication in the United States, with more than five million prescriptions.[10][11]
Medical uses
Prednisolone is a corticosteroid drug with predominant glucocorticoid and low mineralocorticoid activity, making it useful for the treatment of a wide range of inflammatory and autoimmune conditions[12] such as asthma,[13] uveitis, pyoderma gangrenosum, rheumatoid arthritis, urticaria,[14] angioedema,[14] ulcerative colitis, pericarditis, temporal arteritis and Crohn's disease, Bell's palsy, multiple sclerosis,[15] cluster headaches, vasculitis, acute lymphoblastic leukemia and autoimmune hepatitis,[16] systemic lupus erythematosus, Kawasaki disease,[17] dermatomyositis,[4] and sarcoidosis.[18]
Prednisolone acetate ophthalmic suspension (eye drops) is an adrenocortical steroid product, prepared as a sterile ophthalmic suspension and used to reduce swelling, redness, itching, and allergic reactions affecting the eye.[19][5][20] It has been explored as a treatment option for bacterial keratitis.[21]
Prednisolone can also be used for allergic reactions ranging from seasonal allergies to drug allergic reactions.[22]
Prednisolone can also be used as an immunosuppressive drug for organ transplants.[4][23]
Prednisolone in lower doses can be used in cases of primary adrenal insufficiency (Addison's disease).[24][25]
Corticosteroids inhibit the inflammatory response to a variety of inciting agents and, it is presumed, delay or slow healing.[26] They inhibit the edema, fibrin deposition, capillary dilation, leukocyte migration, capillary proliferation, fibroblast proliferation, deposition of collagen, and scar formation with inflammation.[27]
Adverse effects
Adverse reactions from the use of prednisolone include:[28][4]
- Increased appetite, weight gain, nausea, and malaise
- Increased risk of infection
- Cardiovascular events
- Dermatological effects including reddening of face, bruising/skin discoloration, impaired wound healing, thinning of skin, skin rash, fluid build up and abnormal hair growth
- Hyperglycemia; patients with diabetes may need increased insulin or diabetic therapies
- Menstrual abnormalities
- Less response to hormones, especially during stressful instances such as surgery or illness
- Change in electrolytes: rise in blood pressure, increased sodium and low potassium, leading to alkalosis
- GI system effects: swelling of stomach lining, reversible increase in liver enzymes, and risk of stomach ulcers
- Muscular and skeletal abnormalities, such as muscle weakness/muscle loss, osteoporosis (see steroid-induced osteoporosis), long bone fractures, tendon rupture, and back fractures
- Neurological effects, including involuntary movements (convulsions), headaches, and vertigo
- Behavioral disturbances [29]
- Nasal septum perforation and bowel perforation (in some pathologic conditions).[30][31]
Withdrawal from prednisolone after long-term or high-dose use can lead to adrenal insufficiency.[29]
Pregnancy and breastfeeding
Although there are no major human studies of prednisolone use in pregnant women, studies in several animals show that it may cause birth defects including increase cleft palate. Prednisolone should be used in pregnant women when benefits outweigh the risks and children born from mothers using prednisolone during pregnancy should be monitored for impaired adrenal function.
Prednisolone is found in breast milk of mothers taking prednisolone.[29]
Pharmacology
As a glucocorticoid, the lipophilic structure of prednisolone allows for easy passage through the cell membrane where it then binds to its respective glucocorticoid receptor (GCR) located in the cytoplasm. Upon binding, formation of the GC/GCR complex causes dissociation of chaperone proteins from the glucocorticoid receptor enabling the GC/GCR complex to translocate inside the nucleus. This process occurs within 20 minutes of binding. Once inside the nucleus, the homodimer GC/GCR complex binds to specific DNA binding-sites known as glucocorticoid response elements (GREs) resulting in gene expression or inhibition. Complex binding to positive GREs leads to synthesis of anti-inflammatory proteins while binding to negative GREs blocks the transcription of inflammatory genes.[32]
Chemistry
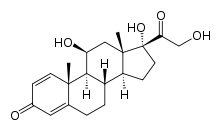
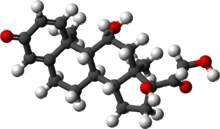
Prednisolone is a synthetic pregnane corticosteroid closely related to its cognate prednisone, having identical structure save for two fewer hydrogens near C11. It is also known as δ1-cortisol, δ1-hydrocortisone, 1,2-dehydrocortisol, or 1,2-dehydrohydrocortisone, as well as 11β,17α,21-trihydroxypregna-1,4-diene-3,20-dione.[33][34]
Society and culture
Dosage forms
In the United States:
- Prednisolone sodium phosphate oral solution (Pediapred)[29]
- Prednisolone acetate oral suspension (Flo-Pred)[28]
- Prednisolone oral tablets (Millipred)[22]
- Prednisolone sodium phosphate oral dissolving tablets (Orapred ODT)[4]
- Prednisolone acetate ophthalmic suspension (Omnipred, Pred Forte)[5][19][20]
Athletics
As a glucocorticosteroid, unauthorized or ad-hoc use of prednisolone during competition via oral, intravenous, intramuscular or rectal routes is banned under World Anti-Doping Agency (WADA) anti-doping rules.[35]
Veterinary uses
Prednisolone is used in the treatment of inflammatory and allergic conditions in cats, dogs, and ferrets.
See also
- Methylprednisolone
- Loteprednol
References
- "Prednisolone Use During Pregnancy". Drugs.com. 16 January 2000. Retrieved 9 March 2020.
- World Health Organization (2009). Stuart MC, Kouimtzi M, Hill SR (eds.). WHO Model Formulary 2008. World Health Organization. pp. 53–54. hdl:10665/44053. ISBN 9789241547659.
- "Prednisolone". The American Society of Health-System Pharmacists. Archived from the original on 23 December 2016. Retrieved 8 December 2016.
- "Orapred ODT- prednisolone sodium phosphate tablet, orally disintegrating". DailyMed. 11 September 2019. Retrieved 9 March 2020.
- "Omnipred- prednisolone acetate suspension". DailyMed. 9 September 2019. Retrieved 9 March 2020.
- "Pevanti 10mg Tablets – Summary of Product Characteristics (SPC) – (eMC)". www.medicines.org.uk. 1 December 2014. Archived from the original on 20 December 2016. Retrieved 13 December 2016.
- Kim K, Roh JK, Wee H, Kim C (2016). Cancer Drug Discovery: Science and History. Springer. p. 169. ISBN 9789402408447. Archived from the original on 10 September 2017.
- World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- "Prednisolone" (PDF). WHO International Drug Price Indicator Guide, 2014.
- "The Top 300 of 2020". ClinCalc. Retrieved 11 April 2020.
- "Prednisolone - Drug Usage Statistics". ClinCalc. Retrieved 11 April 2020.
- Czock D, Keller F, Rasche FM, Häussler U (2005). "Pharmacokinetics and pharmacodynamics of systemically administered glucocorticoids". Clinical Pharmacokinetics. 44 (1): 61–98. doi:10.2165/00003088-200544010-00003. PMID 15634032.
- Fiel SB, Vincken W (June 2006). "Systemic corticosteroid therapy for acute asthma exacerbations". The Journal of Asthma. 43 (5): 321–31. doi:10.1080/02770900600567163. PMID 16801135.
- Spickett G (2014). "Urticaria and angioedema". J R Coll Physicians Edinb. 44 (1): 50–4. doi:10.4997/JRCPE.2014.112. PMID 24995449.
- Thrower BW (January 2009). "Relapse management in multiple sclerosis". The Neurologist. 15 (1): 1–5. doi:10.1097/NRL.0b013e31817acf1a. PMID 19131851.
- Lambrou GI, Vlahopoulos S, Papathanasiou C, Papanikolaou M, Karpusas M, Zoumakis E, Tzortzatou-Stathopoulou F (December 2009). "Prednisolone exerts late mitogenic and biphasic effects on resistant acute lymphoblastic leukemia cells: Relation to early gene expression". Leukemia Research. 33 (12): 1684–95. doi:10.1016/j.leukres.2009.04.018. PMID 19450877.
- Miura M, Tamame T, Naganuma T, Chinen S, Matsuoka M, Ohki H (October 2011). "Steroid pulse therapy for Kawasaki disease unresponsive to additional immunoglobulin therapy". Paediatrics & Child Health. 16 (8): 479–84. doi:10.1093/pch/16.8.479. PMC 3202387. PMID 23024586.
- Gera K, Gupta N, Ahuja A, Shah A (April 2014). "Acute alveolar sarcoidosis presenting with hypoxaemic respiratory failure". BMJ Case Reports. 2014: bcr2013202247. doi:10.1136/bcr-2013-202247. PMC 4024548. PMID 24789154.
- "Pred Forte- prednisolone acetate suspension/ drops". DailyMed. 19 July 2019. Retrieved 9 March 2020.
- "Pred Mild- prednisolone acetate suspension/ drops". DailyMed. 19 July 2019. Retrieved 9 March 2020.
- Herretes S, Wang X, Reyes JM (October 2014). "Topical corticosteroids as adjunctive therapy for bacterial keratitis". The Cochrane Database of Systematic Reviews (10): CD005430. doi:10.1002/14651858.CD005430.pub3. PMC 4269217. PMID 25321340.
- "Millipred- prednisolone tablet". DailyMed. 8 April 2019. Retrieved 9 March 2020.
- Vethe NT, Midtvedt K, Asberg A, Amundsen R, Bergan S (October 2011). "[Drug interactions and immunosuppression in organ transplant recipients]". Tidsskrift for den Norske Laegeforening. 131 (20): 2000–3. doi:10.4045/tidsskr.11.0138. PMID 22016125.
- Husebye ES, Allolio B, Arlt W, Badenhoop K, Bensing S, Betterle C, Falorni A, Gan EH, Hulting AL, Kasperlik-Zaluska A, Kämpe O, Løvås K, Meyer G, Pearce SH (February 2014). "Consensus statement on the diagnosis, treatment and follow-up of patients with primary adrenal insufficiency". Journal of Internal Medicine. 275 (2): 104–15. doi:10.1111/joim.12162. PMID 24330030.
- AMA Department of Drugs: AMA Drug Evaluations (6th ed.). Chicago, IL: American Medical Association. 1986.
- Schwiebert LM, Beck LA, Stellato C, Bickel CA, Bochner BS, Schleimer RP, Schwiebert LA (January 1996). "Glucocorticosteroid inhibition of cytokine production: relevance to antiallergic actions". The Journal of Allergy and Clinical Immunology. 97 (1 Pt 2): 143–52. doi:10.1016/s0091-6749(96)80214-4. PMID 8568145.
- Lee SH (November 2015). "Mechanisms of Glucocorticoid Action in Chronic Rhinosinusitis". Allergy, Asthma & Immunology Research. 7 (6): 534–7. doi:10.4168/aair.2015.7.6.534. PMC 4605925. PMID 26333699.
- "Flo-Pred- prednisolone acetate suspension". DailyMed. 28 February 2019. Retrieved 9 March 2020.
- "Pediapred- prednisolone sodium phosphate solution". DailyMed. 29 January 2020. Retrieved 9 March 2020.
- ReMine SG, McIlrath DC (1980). "Bowel perforation in steroid-treated patients". Annals of Surgery. 192 (4): 581–6. doi:10.1097/00000658-198010000-00016. PMC 1347010. PMID 7425698.
- Cervin A, Andersson M (September 1998). "Intranasal steroids and septum perforation--an overlooked complication? A description of the course of events and a discussion of the causes". Rhinology. 36 (3): 128–32. PMID 9830677.
- Stahn C, Löwenberg M, Hommes DW, Buttgereit F (September 2007). "Molecular mechanisms of glucocorticoid action and selective glucocorticoid receptor agonists" (PDF). Molecular and Cellular Endocrinology. 275 (1–2): 71–8. doi:10.1016/j.mce.2007.05.019. PMID 17630118.
- Elks J (14 November 2014). The Dictionary of Drugs: Chemical Data: Chemical Data, Structures and Bibliographies. Springer. pp. 1011–1012. ISBN 978-1-4757-2085-3. Archived from the original on 10 September 2017.
- Index Nominum 2000: International Drug Directory. Taylor & Francis. January 2000. pp. 869–. ISBN 978-3-88763-075-1. Archived from the original on 10 September 2017.
- "Prohibited List" (PDF). World Anti-Doping Agency. January 2020. Archived (PDF) from the original on 8 August 2011.
External Links
- "Prednisolone". Drug Information Portal. U.S. National Library of Medicine.
- "Prednisolone Ophthalmic". MedlinePlus.
- US patent 2837464, Arthur Nobile, "Process for production of dienes by corynebacteria", published 1958-06-03, issued 1958-06-03, assigned to SCHERING CORP