Clomifene
Clomifene, also known as clomiphene, is a medication used to treat infertility in women who do not ovulate.[3] This includes those who have polycystic ovary syndrome.[3] Use results in a greater chance of twins.[3] It is taken by mouth once a day with a course of treatment generally lasting five days.[3]
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Clomid, Serophene, others[1] |
| Other names | Clomiphene; MRL-41; MRL/41; NSC-35770 |
| AHFS/Drugs.com | Monograph |
| Pregnancy category | |
| Routes of administration | By mouth |
| Drug class | Selective estrogen receptor modulator; Progonadotropin |
| ATC code |
|
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | High (>90%) |
| Metabolism | Liver (with enterohepatic circulation) |
| Elimination half-life | 5–6 days[2] |
| Excretion | Mainly urine, some in bile |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.011.826 |
| Chemical and physical data | |
| Formula | C26H28ClNO |
| Molar mass | 405.966 g·mol−1 |
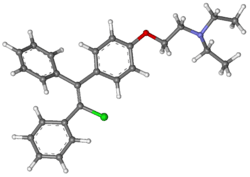
| 3D model (JSmol) | |
| |
InChI
| |
| | |
Common side effects include pelvic pain and hot flashes.[3] Other side effects can include changes in vision, vomiting, trouble sleeping, ovarian cancer, and seizures.[3][4] It is not recommended in people with liver disease, abnormal vaginal bleeding of unknown cause, or who are pregnant.[4][5] Clomifene is in the selective estrogen receptor modulator (SERM) family of medication and is a nonsteroidal medication.[6][5] It works by causing the release of GnRH by the hypothalamus, and subsequently gonadotropin from the anterior pituitary.[4]
Clomifene was approved for medical use in the United States in 1967.[3] It is on the World Health Organization's List of Essential Medicines, the safest and most effective medicines needed in a health system.[7] It is available as a generic medication.[3] The wholesale cost in the developing world is about 0.79 to 2.00 USD for a course of treatment.[8] In the United States the wholesale cost of a course of treatment is 4.80 USD.[9] Its introduction began the era of assisted reproductive technology.[10]
Medical uses
Ovulation induction
Clomifene is one of several alternatives for ovulation induction in those who are infertile due to anovulation or oligoovulation.[11] Evidence is lacking for the use of clomifene in those who are infertile without a known reason.[12] In such cases, studies have observed a clinical pregnancy rate 5.6% per cycle with clomifene treatment vs. 1.3%–4.2% per cycle without treatment.[11]
Proper timing of the drug is important; it should be taken starting on about the fifth day of the cycle, and there should be frequent intercourse.[11][13][14]
The following procedures may be used to monitor induced cycles:[11]
- Follicular monitoring with vaginal ultrasound, starting 4–6 days after the last pill. Serial transvaginal ultrasound can reveal the size and number of developing follicles. It can also provide presumptive evidence of ovulation such as the sudden collapse of the preovulatory follicle, and an increase in fluid volume in the rectouterine pouch. After ovulation, it may reveal signs of luteinization such as loss of clearly defined follicular margins and appearance of internal echoes.
- Serum estradiol levels, starting 4–6 days after the last pill
- Post-coital test 1–3 days before ovulation to check whether there are at least 5 progressive sperm per HPF
- Adequacy of LH surge by urine LH surge tests 3 to 4 days after last clomifene pill
- Mid-luteal progesterone, with at least 10 ng/ml 7–9 days after ovulation being regarded as adequate.
Repeat dosing: This 5-day treatment course can be repeated every 30 days. The dosage may be increased by 50-mg increments in subsequent cycles until ovulation is achieved.[11] It is not recommended by the manufacturer to use clomifene for more than 6 cycles.[14][15]
It is no longer recommended to perform an ultrasound examination to exclude any significant residual ovarian enlargement before each new treatment cycle.[11]
Other uses
Clomifene has also been used with other assisted reproductive technology to increase success rates of these other modalities.[16]
Clomifene is sometimes used in the treatment of male hypogonadism as an alternative to testosterone replacement therapy.[17] The medication has been used at a dosage of 20 to 50 mg three times per week to once day for this indication.[18] It has been found to increase testosterone levels by 2- to 2.5-times in hypogonadal men at such dosages.[18][17] Despite the use of questionnaires in testosterone replacement comparator trials being called into question, clomifene's lower cost, therapeutic benefits, and greater value towards hypogonadism improvement have been noted.[19]
Clomifene has been used in the treatment of gynecomastia.[20] It has been found to be useful in the treatment of some cases of gynecomastia but it is not as effective as tamoxifen or raloxifene for this indication.[21] It has shown variable results for gynecomastia and hence is not recommended for treatment of the condition.[22]
Contraindications
Contraindications include an allergy to the medication, pregnancy, prior liver problems, abnormal vaginal bleeding of unclear cause, ovarian cysts other than those due to polycystic ovarian syndrome, unmanaged adrenal or thyroid problems, and pituitary tumors.[5]
Side effects
The most common adverse drug reaction associated with the use of clomifene (>10% of people) is reversible ovarian enlargement.[14]
Less common effects (1–10% of people) include visual symptoms (blurred vision, double vision, floaters, eye sensitivity to light, scotomata), headaches, vasomotor flushes (or hot flashes), light sensitivity and pupil constriction, abnormal uterine bleeding and/or abdominal discomfort.[14]
Rare adverse events (<1% of people) include: high blood level of triglycerides, liver inflammation, reversible baldness and/or ovarian hyperstimulation syndrome.[14]
Clomifene can lead to multiple ovulation, hence increasing the chance of twins (10% of births instead of ~1% in the general population) and triplets.
Rates of birth defects and miscarriages do not appear to change with the use of clomifene for fertility.[14] Clomifene has been associated with liver abnormalities and a couple of cases of hepatotoxicity.[23]
Cancer association
Some studies have suggested that clomifene if used for more than a year may increase the risk of ovarian cancer.[12] This may only be the case in those who have never been and do not become pregnant.[24] Subsequent studies have failed to support those findings.[11][25]
Clomifene has been shown to be associated with an increased risk of malignant melanomas and thyroid cancer.[26] Thyroid cancer risk was not associated with the number of pregnancies carried to viability.[27]
Pharmacology
Pharmacodynamics
Clomifene is a nonsteroidal triphenylethylene derivative that acts as a selective estrogen receptor modulator (SERM).[28] It consists of a racemic mixture of zuclomifene (~38%) and enclomifene (~62%), each of which has unique pharmacologic properties.[29] It is a mixed agonist and antagonist of the estrogen receptor (ER). Clomifene activates the ERα in the setting of low baseline estrogen levels and partially blocks the receptor in the context of high baseline estrogen levels.[18] Conversely, it is an antagonist of the ERβ.[18] Clomifene is a long-acting ER ligand, with a nuclear retention of greater than 48 hours.[30]
Even though clomifene has some estrogenic effect, the antiestrogenic property is believed to be the primary source for stimulating ovulation.[31] Clomifene appears to act mostly in the hypothalamus where it depletes hypothalamic ERs and blocks the negative feedback effect of circulating endogenous estradiol, which in turn results in an increase in hypothalamic gonadotropin-releasing hormone (GnRH) pulse frequency and circulating concentrations of follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
In normal physiologic female hormonal cycling, at 7 days past ovulation, high levels of estrogen and progesterone produced from the corpus luteum inhibit GnRH, FSH, and LH at the hypothalamus and anterior pituitary. If fertilization does not occur in the post-ovulation period the corpus luteum disintegrates due to a lack of human chorionic gonadotropin (hCG). This would normally be produced by the embryo in the effort of maintaining progesterone and estrogen levels during pregnancy.
Therapeutically, clomifene is given early in the menstrual cycle. It is typically prescribed beginning on day 3 and continuing for 5 days. By that time, FSH levels are rising steadily, causing the development of a few follicles. Follicles, in turn, produce the estrogen, which circulates in serum. In the presence of clomifene, the body perceives a low level of estrogen, similar to day 22 in the previous cycle. Since estrogen can no longer effectively exert negative feedback on the hypothalamus, GnRH secretion becomes more rapidly pulsatile, which results in increased pituitary gonadotropin release. (More rapid, lower amplitude pulses of GnRH lead to increased LH and FSH secretion, while more irregular, larger amplitude pulses of GnRH leads to a decrease in the ratio of LH to FSH.) Increased FSH levels cause the growth of more ovarian follicles, and subsequently rupture of follicles resulting in ovulation. Ovulation occurs most often 6 to 7 days after a course of clomifene.
Clomifene has antiestrogenic effects in the uterus.[32] There is little clinical research on the influence of clomifene in many target tissues, such as lipids, the cardiovascular system, and the breasts.[32][33] Positive effects of clomifene on bone have been observed.[32][33][18] Clomifene has been found to decrease insulin-like growth factor 1 (IGF-1) levels in women.[34]
In normal men, 50 mg/day clomifene for 8 months has been found to increase testosterone levels by around 870 ng/dL in younger men and by around 490 ng/dL in elderly men.[18] Estradiol levels increased by 62 pg/mL in younger men and by 40 pg/mL in elderly men.[18] These findings suggest that the progonadotropic effects of clomifene are stronger in younger men than in older men.[18] In men with hypogonadism, clomifene has been found to increase testosterone levels by 293 to 362 ng/dL and estradiol levels by 5.5 to 13 pg/mL.[18] In a large clinical study of men with low testosterone levels (<400 ng/dL), 25 mg/day clomifene increased testosterone levels from 309 ng/dL to 642 ng/dL after 3 months of therapy.[35] No significant changes in HDL cholesterol, triglycerides, fasting glucose, or prolactin levels were observed, although total cholesterol levels decreased significantly.[35][18]
The
| Medication | Breast | Bone | Liver | Uterus | Vagina | Brain | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Lipids | Coagulation | SHBG | IGF-1 | Hot flashes | Gonadotropins | |||||||||
| Estradiol | + | + | + | + | + | + | + | + | + | + | ||||
| "Ideal SERM" | – | + | + | ± | ± | ± | – | + | + | ± | ||||
| Bazedoxifene | – | + | + | + | + | ? | – | ± | – | ? | ||||
| Clomifene | – | + | + | ? | + | + | – | ? | – | ± | ||||
| Lasofoxifene | – | + | + | + | ? | ? | ± | ± | – | ? | ||||
| Ospemifene | – | + | + | + | + | + | ± | ± | – | ± | ||||
| Raloxifene | – | + | + | + | + | + | ± | – | – | ± | ||||
| Tamoxifen | – | + | + | + | + | + | + | – | – | ± | ||||
| Toremifene | – | + | + | + | + | + | + | – | – | ± | ||||
| Effect: + = Estrogenic / agonistic. ± = Mixed or neutral. – = Antiestrogenic / antagonistic. Sources: See template. | ||||||||||||||
Pharmacokinetics
Clomifene produces N-desmethylclomifene, clomifenoxide (clomifene N-oxide), and 4-hydroxyclomifene as metabolites.[36] Clomifene has an onset of action of 5 to 10 days following course of treatment and an elimination half-life about 5 days. Most clomifene metabolism occurs hepatically, where it undergoes enterohepatic recirculation. Clomifene and its metabolites are excreted primarily through feces (42%), and excretion can occur up to 6 weeks after discontinuation.[29]
Chemistry
Clomifene is a triphenylethylene derivative. It is a mixture of two geometric isomers, enclomifene ((E)-clomifene) and zuclomifene ((Z)-clomifene). These two isomers have been found to contribute to the mixed estrogenic and antiestrogenic properties of clomifene.[10]
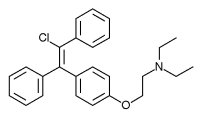 Enclomifene |
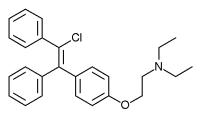 Zuclomifene |
History
A team at William S. Merrell Chemical Company led by Frank Palopoli synthesized clomifene in 1956; after its biological activity was confirmed a patent was filed and issued in November 1959.[10][37] Scientists at Merrell had previously synthesized chlorotrianisene and ethamoxytriphetol.[10]
Clinical studies were conducted under an Investigational New Drug Application; it was third drug for which an IND had been filed under the 1962 Kefauver Harris Amendment to the Federal Food, Drug, and Cosmetic Act that had been passed in response to the thalidomide tragedy.[10] It was approved for marketing in 1967 under the brand name Clomid.[10][38] It was first used to treat cases of oligomenorrhea but was expanded to include treatment of anovulation when women undergoing treatment had higher than expected rates of pregnancy.[39]
The drug is widely considered to have been a revolution in the treatment of female infertility, the beginning of the modern era of assisted reproductive technology, and the beginning of what in the words of Eli Y. Adashi, was "the onset of the US multiple births epidemic".[10][40]
The company was acquired by Dow Chemical in 1980,[41][42] and in 1989 Dow Chemical acquired 67 percent interest of Marion Laboratories, which was renamed Marion Merrell Dow.[41] In 1995 Hoechst AG acquired the pharmaceutical business of Marion Merrell Dow.[43] Hoechst in turn became part of Aventis in 1999,[44]:9–11 and subsequently a part of Sanofi.[45] It became the most widely prescribed drug for ovulation induction to reverse anovulation or oligoovulation.[46]
Society and culture
Brand names
Clomifene is marketed under many brand names worldwide, including Beclom, Bemot, Biogen, Blesifen, Chloramiphene, Clofert, Clomene, ClomHEXAL, Clomi, Clomid, Clomidac, Clomifen, Clomifencitrat, Clomifene, Clomifène, Clomifene citrate, Clomifeni citras, Clomifeno, Clomifert, Clomihexal, Clomiphen, Clomiphene, Clomiphene Citrate, Cloninn, Clostil, Clostilbegyt, Clovertil, Clovul, Dipthen, Dufine, Duinum, Fensipros, Fertab, Fertec, Fertex, Ferticlo, Fertil, Fertilan, Fertilphen, Fertin, Fertomid, Ferton, Fertotab, Fertyl, Fetrop, Folistim, Genoclom, Genozym, Hete, I-Clom, Ikaclomin, Klofit, Klomen, Klomifen, Lomifen, MER 41, Milophene, Ofertil, Omifin, Ova-mit, Ovamit, Ovinum, Ovipreg, Ovofar, Ovuclon, Ovulet, Pergotime, Pinfetil, Profertil, Prolifen, Provula, Reomen, Serofene, Serophene, Serpafar, Serpafar, Surole, Tocofeno, and Zimaquin.[1]
Regulation
Clomifene is included on the World Anti-Doping Agency list of illegal doping agents in sport.[47] It is listed because it is an "anti-estrogenic substance".
Research
Clomifene has been used almost exclusively for ovulation induction in premenopausal women, and has been studied very limitedly in postmenopausal women.[48]
Clomifene was studied for treatment and prevention of breast cancer, but issues with toxicity led to abandonment of this indication, as did the discovery of tamoxifen.[49] Like the structurally related drug triparanol, clomifene is known to inhibit the enzyme 24-dehydrocholesterol reductase and increase circulating desmosterol levels, making it unfavorable for extended use in breast cancer due to risk of side effects like irreversible cataracts.[50][51]
References
- "International brands of clomifene -". Drugs.com. Archived from the original on 20 September 2016. Retrieved 11 September 2016.
- Yilmaz S, Yilmaz Sezer N, Gönenç İM, İlhan SE, Yilmaz E (April 2018). "Safety of clomiphene citrate: a literature review". Cytotechnology. 70 (2): 489–495. doi:10.1007/s10616-017-0169-1. PMC 5851961. PMID 29159661.
- "Clomiphene Citrate". The American Society of Health-System Pharmacists. Archived from the original on 14 September 2017. Retrieved 8 December 2016.
- WHO Model Formulary 2008 (PDF). World Health Organization. 2009. pp. 385–386. ISBN 9789241547659. Archived (PDF) from the original on 13 December 2016. Retrieved 8 December 2016.
- "Clomiphene citrate tablets USP" (PDF). FDA. Retrieved 31 July 2019.
- Ghumman, Surveen (2015). Principles and Practice of Controlled Ovarian Stimulation in ART. Springer. p. 65. ISBN 9788132216865. Archived from the original on 2016-12-27.
- World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- "Clomifene". International Drug Price Indicator Guide. Retrieved 8 December 2016.
- "NADAC as of 2016-12-21 | Data.Medicaid.gov". Centers for Medicare and Medicaid Services. Archived from the original on 24 December 2016. Retrieved 26 December 2016.
- Dickey, RP; Holtkamp, DE (1996). "Development, pharmacology and clinical experience with clomiphene citrate" (PDF). Human Reproduction Update. 2 (6): 483–506. doi:10.1093/humupd/2.6.483. PMID 9111183.
- Practice Committee of the American Society for Reproductive Medicine (August 2013). "Use of clomiphene citrate in infertile women: a committee opinion". Fertil. Steril. 100 (2): 341–8. doi:10.1016/j.fertnstert.2013.05.033. PMID 23809505.
- Hughes, E; Brown, J; Collins, JJ; Vanderkerchove, P (Jan 20, 2010). "Clomiphene citrate for unexplained subfertility in women". The Cochrane Database of Systematic Reviews (1): CD000057. doi:10.1002/14651858.CD000057.pub2. PMC 7052733. PMID 20091498.
- "Clomifene 50mg Tablets - Summary of Product Characteristics (SPC) - (eMC)". Last updated July 2007: UK Electronic Medicines Compendium. Archived from the original on August 22, 2016. Retrieved September 11, 2016.CS1 maint: location (link)
- "Clomiphene citrate tablets label" (PDF). Revised October 2012: FDA. Archived (PDF) from the original on September 27, 2016. Retrieved September 11, 2016.CS1 maint: location (link)
- Trabert, B.; Lamb, E. J.; Scoccia, B.; Moghissi, K. S.; Westhoff, C. L.; Niwa, S.; Brinton, L. A. (2013). "Ovulation-inducing drugs and ovarian cancer risk: Results from an extended follow-up of a large US infertility cohort". Fertility and Sterility. 100 (6): 1660–6. doi:10.1016/j.fertnstert.2013.08.008. PMC 3873340. PMID 24011610.
- Seli, Emre. "Ovulation induction with clomiphene citrate". UpToDate. Archived from the original on 21 December 2016. Retrieved 21 April 2014.
- Bach, Phil Vu; Najari, Bobby B.; Kashanian, James A. (2016). "Adjunct Management of Male Hypogonadism". Current Sexual Health Reports. 8 (4): 231–239. doi:10.1007/s11930-016-0089-7. ISSN 1548-3584.
- Trost, Landon W.; Khera, Mohit (2014). "Alternative Treatment Modalities for the Hypogonadal Patient". Current Urology Reports. 15 (7). doi:10.1007/s11934-014-0417-2. ISSN 1527-2737.
- DiGiorgio, Lorenzo; Sadeghi-Nejad, Hossein (December 2016). "Off label therapies for testosterone replacement". Translational Andrology and Urology. 5 (6): 844–849. doi:10.21037/tau.2016.08.15. PMC 5182219. PMID 28078215.
- Kenneth L. Becker (2001). Principles and Practice of Endocrinology and Metabolism. Lippincott Williams & Wilkins. pp. 1206–. ISBN 978-0-7817-1750-2.
- Agrawal, Sweety; Ganie, Mohd Ashraf; Nisar, Sobia (2017). "Gynaecomastia". Basics of Human Andrology. pp. 451–458. doi:10.1007/978-981-10-3695-8_26. ISBN 978-981-10-3694-1.
- Nordt CA, DiVasta AD (August 2008). "Gynecomastia in adolescents". Curr. Opin. Pediatr. 20 (4): 375–82. doi:10.1097/MOP.0b013e328306a07c. PMID 18622190.
- Ross Cameron; George Feuer; Felix de la Iglesia (6 December 2012). Drug-Induced Hepatotoxicity. Springer Science & Business Media. pp. 565–. ISBN 978-3-642-61013-4.
- Trabert, B; Lamb, EJ; Scoccia, B; Moghissi, KS; Westhoff, CL; Niwa, S; Brinton, LA (Dec 2013). "Ovulation-inducing drugs and ovarian cancer risk: results from an extended follow-up of a large United States infertility cohort". Fertility and Sterility. 100 (6): 1660–6. doi:10.1016/j.fertnstert.2013.08.008. PMC 3873340. PMID 24011610.
- Gadducci, A; Guerrieri, ME; Genazzani, AR (Jan 2013). "Fertility drug use and risk of ovarian tumors: a debated clinical challenge". Gynecological Endocrinology. 29 (1): 30–5. doi:10.3109/09513590.2012.705382. PMID 22946709.
- Yilmaz, Serkan; Yilmaz Sezer, Neslihan; Gönenç, İlknur Münevver; İlhan, Sibel Erkal; Yilmaz, Ebru (April 2018). "Safety of clomiphene citrate: a literature review". Cytotechnology. 70 (2): 489–495. doi:10.1007/s10616-017-0169-1. ISSN 0920-9069. PMC 5851961. PMID 29159661.
- Yu, QingAn; Lv, XiaoYing; Liu, KunPeng; Ma, DaKun; Wu, YaoHua; Dai, WenJie; Jiang, HongChi (2018). "Fertility Drugs Associated with Thyroid Cancer Risk: A Systematic Review and Meta-Analysis". BioMed Research International. 2018: 7191704. doi:10.1155/2018/7191704. ISSN 2314-6133. PMC 5971354. PMID 29862285.
- Seli, Emre; Arici, Aydin. "Ovulation induction with clomiphene citrate". UpToDate. Retrieved 2019-07-30.
- "ClomiPHENE (Professional Patient Advice)". Drugs.com. Retrieved 2019-07-30.
- Benno Runnebaum; Thomas Rabe (17 April 2013). Gynäkologische Endokrinologie und Fortpflanzungsmedizin: Band 1: Gynäkologische Endokrinologie. Springer-Verlag. pp. 88–. ISBN 978-3-662-07635-4.
- "Clomiphene Citrate Drug Information, Professional". Drugs.com. Retrieved 2019-08-06.
- Goldstein, S. R. (2000). "A pharmacological review of selective oestrogen receptor modulators". Human Reproduction Update. 6 (3): 212–224. doi:10.1093/humupd/6.3.212. ISSN 1355-4786. PMID 10874566.
- Haskell, Sally G. (2003). "Selective Estrogen Receptor Modulators". Southern Medical Journal. 96 (5): 469–476. doi:10.1097/01.SMJ.0000051146.93190.4A. ISSN 0038-4348. PMID 12911186.
- Duarte FH, Jallad RS, Bronstein MD (November 2016). "Estrogens and selective estrogen receptor modulators in acromegaly". Endocrine. 54 (2): 306–314. doi:10.1007/s12020-016-1118-z. PMID 27704479.
- Rambhatla A, Mills JN, Rajfer J (2016). "The Role of Estrogen Modulators in Male Hypogonadism and Infertility". Rev Urol. 18 (2): 66–72. doi:10.3909/riu0711 (inactive 2020-03-08). PMC 5010627. PMID 27601965.
- Analytical Profiles of Drug Substances and Excipients. Academic Press. 20 March 1998. pp. 113–. ISBN 978-0-08-086120-3. Archived from the original on 5 November 2017.
- Allen, R.E., Palopoli, F.P., Schumann, E.L. and Van Campen, M.G. Jr. (1959) U.S. Patent No. 2,914,563 Archived 2016-10-26 at the Wayback Machine, Nov. 24, 1959.
- Holtkamp DE, Greslin JG, Root CA, Lerner LJ (October 1960). "Gonadotrophin inhibiting and anti-fecundity effects of chloramiphene". Proc. Soc. Exp. Biol. Med. 105: 197–201. doi:10.3181/00379727-105-26054. PMID 13715563.
- Hughes E, Collins J, Vandekerckhove P (2000). "Clomiphene citrate for ovulation induction in women with oligo-amenorrhoea". Cochrane Database Syst Rev (2): CD000056. doi:10.1002/14651858.CD000056. PMID 10796477. (Retracted, see doi:10.1002/14651858.cd000056.pub2)
- Adashi, Eli Y. (Fall 2014). "Iatrogenic Birth Plurality: The Challenge and Its Possible Solution" (PDF). Harvard Health Policy Review. 14 (1): 9–10. Archived from the original (PDF) on 2016-10-06. Retrieved 2016-09-12.
- Lee, Patrick (18 July 1989). "Dow Chemical to Get Control of Marion Labs : $5-Billion-Plus Deal Is an Effort to Diversify". Los Angeles Times. Archived from the original on 29 June 2016.
- Times, Winston Williams, Special To The New York (11 February 1981). "Dow Broadens Product Lines". The New York Times. ISSN 0362-4331. Archived from the original on 6 October 2016.
- "Hoechst AG to Buy Marion Merrell Dow / Acquisition worth over $7 billion". San Francisco Chronicle. Reuters. May 5, 1995. Archived from the original on October 6, 2016.
- Arturo Bris and Christos Cabolis, Corporate Governance Convergence Through Cross-Border Mergers The Case of Aventis Archived 2014-04-21 at the Wayback Machine, Chapter 4 in Corporate Governance and Regulatory Impact on Mergers and Acquisitions: Research and Analysis on Activity Worldwide Since 1990. Eds Greg N. Gregoriou, Luc Renneboog. Academic Press, 26 July 2007
- Timmons, Heather; Bennhold, Katrin (27 April 2004). "France Helped Broker the Aventis-Sanofi Deal". The New York Times. Archived from the original on 5 November 2017.
- Jerome Frank Strauss; Robert L. Barbieri (13 September 2013). Yen and Jaffe's Reproductive Endocrinology. Elsevier Health Sciences. pp. 518–. ISBN 978-1-4557-2758-2. Archived from the original on 5 November 2017.
- The WADA Prohibited List 2016 (listed as clomiphene) Archived 2016-03-06 at the Wayback Machine
- Palacios, Santiago (2007). "The future of the new selective estrogen receptor modulators". Menopause International. 13 (1): 27–34. doi:10.1258/175404507780456791. ISSN 1754-0453. PMID 17448265.
- Maximov, PY; Lee, TM; Jordan, VC (May 2013). "The discovery and development of selective estrogen receptor modulators (SERMs) for clinical practice". Current Clinical Pharmacology. 8 (2): 135–55. doi:10.2174/1574884711308020006. PMC 3624793. PMID 23062036.
- Hormones and Breast Cancer. Elsevier. 25 June 2013. pp. 13–. ISBN 978-0-12-416676-9. Archived from the original on 5 November 2017.
- Maximov, Philipp Y.; McDaniel, Russell E.; Jordan, V. Craig (2013). "Tamoxifen Goes Forward Alone". Milestones in Drug Therapy: 31–46. doi:10.1007/978-3-0348-0664-0_2. ISBN 978-3-0348-0663-3. ISSN 2296-6064.