Misoprostol
Misoprostol, sold under the brandname Cytotec among others, is a medication used to prevent and treat stomach ulcers, start labor, cause an abortion, and treat postpartum bleeding due to poor contraction of the uterus.[1][2] For abortions it is used by itself and with mifepristone or methotrexate.[3] By itself, effectiveness for abortion is between 66% and 90%.[4][5] Misoprostol is taken by mouth when used to prevent gastric ulcers in persons taking NSAIDs.[2] For labor induction or abortion, it is taken by mouth, dissolved in the mouth, or placed in the vagina.[3][6][7] For postpartum bleeding it may also be used rectally.[8]
 | |
| Clinical data | |
|---|---|
| Trade names | Cytotec, Misodel, other |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a689009 |
| License data |
|
| Pregnancy category | |
| Routes of administration | By mouth, vaginal, under the tongue |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | extensively absorbed |
| Protein binding | 80-90% (active metabolite, misoprostol acid) |
| Metabolism | Liver (extensive to misoprostic acid) |
| Elimination half-life | 20–40 minutes |
| Excretion | Urine (80%) |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.190.521 |
| Chemical and physical data | |
| Formula | C22H38O5 |
| Molar mass | 382.534 g/mol g·mol−1 |
| 3D model (JSmol) | |
| |
InChI
| |
| (verify) | |
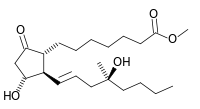
Common side effects include diarrhea and abdominal pain.[2] It is pregnancy category X meaning that it is known to result in negative outcomes for the baby if taken during pregnancy.[2] In rare cases, uterine rupture may occur.[2] It is a prostaglandin analogue — specifically, a synthetic prostaglandin E1 (PGE1).[2]
Misoprostol was developed in 1973.[9] It is on the World Health Organization's List of Essential Medicines, the safest and most effective medicines needed in a health system.[10] It is available as a generic medication.[2] The wholesale cost in the developing world is about 0.36 to 2.00 USD a dose.[11] A month's supply to treat stomach ulcers in the United States is between 100 and 200 USD.[12] The same costs between 30 and 55 EUR in Europe.[13]
Medical uses
Ulcer prevention
Misoprostol is used for the prevention of NSAID-induced gastric ulcers. It acts upon gastric parietal cells, inhibiting the secretion of gastric acid by G-protein coupled receptor-mediated inhibition of adenylate cyclase, which leads to decreased intracellular cyclic AMP levels and decreased proton pump activity at the apical surface of the parietal cell. Because other classes of drugs, especially H2-receptor antagonists and proton pump inhibitors, are more effective for the treatment of acute peptic ulcers, misoprostol is only indicated for use by people who are both taking NSAIDs and are at high risk for NSAID-induced ulcers, including the elderly and people with ulcer complications. Misoprostol is sometimes coprescribed with NSAIDs to prevent their common adverse effect of gastric ulceration (e.g. with diclofenac in Arthrotec).
However, even in the treatment of NSAID-induced ulcers, omeprazole proved to be at least as effective as misoprostol,[14] but was significantly better tolerated, so misoprostol should not be considered a first-line treatment. Misoprostol-induced diarrhea and the need for multiple daily doses (typically four) are the main issues impairing compliance with therapy.
Labor induction
Misoprostol is commonly used for labor induction. It causes uterine contractions and the ripening (effacement or thinning) of the cervix.[15] It can be less expensive than the other commonly used ripening agent, dinoprostone.[16]
Oxytocin has long been used as the standard agent for labor induction, but does not work well when the cervix is not yet ripe. Misoprostol also may be used in conjunction with oxytocin.[16]
Between 2002 and 2012, a misoprostol vaginal insert was studied, and was approved in the EU.[17][18] It was not approved for use in the USA, and the US FDA still considers cervical ripening and labor induction to be outside of the approved uses for misoprostol.[19]
Abortion
Misoprostol is used either alone or in conjunction with another medication (mifepristone or methotrexate) for medical abortions as an alternative to surgical abortion.[20] Medical abortion has the advantage of being less invasive, and more autonomous, self-directed, and discreet. It is preferable to some users because it feels more "natural," as the drugs induce a miscarriage.[21] It is also more easily accessible in places where abortion is illegal.[22] The World Health Organization provides clear guidelines on the use, benefits and risks of misoprostol for abortions.[23]
Misoprostol is most effective when it is used with methotrexate or mifepristone (RU-486).[24] Misoprostol alone is less effective (typically 88% up to eight-weeks gestation). It is not inherently unsafe if medically supervised, but 1% of women will have heavy bleeding requiring medical attention, some women may have ectopic pregnancy, and the 12% of pregnancies that continue after misoprostol failure are more likely to have birth defects and are usually followed up with a more effective method of abortion.[25]
Most large studies recommend a protocol for the use of misoprostol in combination with mifepristone.[26] Together they are effective in around 95% for early pregnancies.[27] Misoprostol alone may be more effective in earlier gestation.[28] WHO guidelines recommend for pregnancies up to 12 weeks to use 12 tablets of 200 mcg (micrograms). The woman should put 4 tablets of misoprostol under the tongue or far up the vagina and let them dissolve for 30 minutes. She should wait 3 hours and repeat with 4 pills under the tongue or in the vagina for 30 minutes. She should wait 3 hours and repeat once more.[24] It works in 90% after first attempt and, in case of failure, the attempt may be repeated after a minimum of 3 days.
Misoprostol can also be used to dilate the cervix in preparation for a surgical abortion, particularly in the second trimester (either alone or in combination with laminaria stents).
Misoprostol by mouth is the least effective treatment for producing complete abortion in a period of 24 hours due to the liver's first-pass effect which reduces the bioavailability of the misoprostol. Vaginal and sublingual routes result in greater efficacy and extended duration of action because these routes of administration allow the drug to be directly absorbed into circulation by bypassing the liver first-pass effect.[29][30]
The following tests are recommended before use for abortion confirmation of pregnancy, hematocrit or Hb tests, and Rh testing.[31] Following use, it is recommended that people attend a follow-up visit 2 weeks after treatment. If used for treatment of complete abortion, a pregnancy test, physical examination of the uterus, and ultrasound should be performed to ensure success of treatment. Surgical management is possible in the case of failed treatment.[29]
Failed miscarriage
Misoprostol may be used to treat the mother in the case of fetal death which did not result in miscarriage. Further research is needed to establish a safe, effective protocol.[32]
Misoprostol is regularly used in some Canadian hospitals for labour induction for fetal deaths early in pregnancy, and for termination of pregnancy for fetal anomalies. A low dose is used initially, then doubled for the remaining doses until delivery. In the case of a previous Caesarian section, however, lower doses are used.
Postpartum bleeding
Misoprostol is also used to prevent and treat post-partum bleeding. Orally administered misoprostol was marginally less effective than oxytocin.[33] The use of rectally administered misoprostol is optimal in cases of bleeding; it was shown to be associated with lower rates of side effects compared to other routes. Rectally administered misoprostol was reported in a variety of case reports and randomised controlled trials.[34][35] However, it is inexpensive and thermostable (thus does not require refrigeration like oxytocin), making it a cost-effective and valuable drug to use in the developing world.[36] A randomised control trial of misoprostol use found a 38% reduction in maternal deaths due to post partum haemorrhage in resource-poor communities.[37] Misoprostol is recommended due to its cost, effectiveness, stability, and low rate of side effects.[38] Oxytocin must also be given by injection, while misprostol can be given orally or rectally for this use, making it much more useful in areas where nurses and physicians are less available.[39]
Other
For cervical ripening in advance of endometrial biopsy to reduce the need for use of a tenaculum or cervical dilator.
Adverse effects
The most commonly reported adverse effect of taking a misoprostol by mouth for the prevention of stomach ulcers is diarrhea. In clinical trials, an average 13% of people reported diarrhea, which was dose-related and usually developed early in the course of therapy (after 13 days) and was usually self-limiting (often resolving within 8 days), but sometimes (in 2% of people) required discontinuation of misoprostol.[40]
The next most commonly reported adverse effects of taking misoprostol by mouth for the prevention of gastric ulcers are: abdominal pain, nausea, flatulence, headache, dyspepsia, vomiting, and constipation, but none of these adverse effects occurred more often than when taking placebos.[40] In practice, fever is almost universal when multiple doses are given every 4 to 6 hours.
There are increased side effects with sublingual or oral misoprostol, compared to a low dose (400 ug) vaginal misoprostol. However, low dose vaginal misoprostol was linked with low complete abortion rate.[29] The study concluded that sublingually administered misoprostol dosed at 600 ug or 400 ug had greater instances of fever and diarrhea due to its quicker onset of action, higher peak concentration and bioavailability in comparison to vaginal or oral misoprostol.[29]
For the indication of medical abortion, bleeding and cramping is commonly experienced after administration of misoprostol. Bleeding and cramping is likely to be greater than that experienced with menses, however, emergency care is advised if bleeding is excessive.[31]
Misoprostol should not be taken by pregnant women with wanted pregnancies to reduce the risk of NSAID-induced gastric ulcers because it increases uterine tone and contractions in pregnancy, which may cause partial or complete abortions, and because its use in pregnancy has been associated with birth defects.[40][41]
All cervical ripening and induction agents can cause uterine hyperstimulation, which can negatively affect the blood supply to the fetus and increases the risk of complications such as uterine rupture.[42] Concern has been raised that uterine hyperstimulation that occurs during a misoprostol-induced labor is more difficult to treat than hyperstimulation during labors induced by other drugs.[43] Because the complications are rare, it is difficult to determine if misoprostol causes a higher risk than do other cervical ripening agents. One estimate is that it would require around 61,000 people enrolled in randomized controlled trials to detect a difference in serious fetal complications and about 155,000 people to detect a difference in serious maternal complications.[44]
Contraindications
It is recommended that medical treatment for missed abortion with misoprostol should only be considered in people without the following contraindications: suspected ectopic pregnancy, use of non-steroidal drugs, signs of pelvic infections or sepsis, unstable hemodynamics, known allergy to misoprostol, previous caesarean section, mitral stenosis, hypertension, glaucoma, bronchial asthma, and remote areas without a hospital nearby.[29]
Pharmacology
Mechanism of action
Misoprostol, a prostaglandin analogue, binds to myometrial cells to cause strong myometrial contractions leading to expulsion of tissue. This agent also causes cervical ripening with softening and dilation of the cervix. Misoprostol binds to and stimulates prostaglandin EP2 receptors, prostaglandin EP3 receptor and prostaglandin EP4 receptor but not Prostaglandin EP1 receptor and therefore is expected to have a more restricted range of physiological and potentially toxic actions than prostaglandin E2 or other analogs which activate all four prostaglandin receptors.[45]
Society and culture
A letter from Searle generated some controversy over the use of misoprostol in labor inductions.[46] The American College of Obstetricians and Gynecologists holds that substantial evidence supports the use of misoprostol for induction of labor, a position it reaffirmed in 2000 in response to the Searle letter.[47] It is on the World Health Organization's List of Essential Medicines, the safest and most effective medicines needed in a health system.[10]
The largest medical malpractice award of nearly $70 million was awarded due to the use of misoprostol to induce labor in a California hospital.[48]
A vaginal form of the medication is sold in the EU under the names Misodel and Mysodelle for use in labor induction.
Black market
Misoprostol is used for self-induced abortions in Brazil, where black market prices exceed US$100 per dose. Illegal medically unsupervised misoprostol abortions in Brazil are associated with a lower complication rate than other forms of illegal self-induced abortion, but are still associated with a higher complication rate than legal, medically supervised surgical and medical abortions. Failed misoprostol abortions are associated with birth defects in some cases.[49][50][51][52][53] Low-income and immigrant populations in New York City have also been observed to use self-administered misoprostol to induce abortions, as this method is much cheaper than a surgical abortion (about $2 per dose).[54] The drug is readily available in Mexico.[55] Use of misoprostol has also increased in Texas in response to increased regulation of abortion providers.[56]
References
- Rostom A, Dube C, Wells G, Tugwell P, Welch V, Jolicoeur E, McGowan J (2002). "Prevention of NSAID-induced gastroduodenal ulcers". Cochrane Database Syst Rev (4): CD002296. doi:10.1002/14651858.CD002296. PMID 12519573.
- "Misoprostol". The American Society of Health-System Pharmacists. Archived from the original on 21 February 2015. Retrieved 20 February 2015.
- Kulier, R; Kapp, N; Gülmezoglu, AM; Hofmeyr, GJ; Cheng, L; Campana, A (9 November 2011). "Medical methods for first trimester abortion". The Cochrane Database of Systematic Reviews (11): CD002855. doi:10.1002/14651858.CD002855.pub4. PMID 22071804.
- Bryant, AG; Regan, E; Stuart, G (January 2014). "An overview of medical abortion for clinical practice". Obstetrical & Gynecological Survey. 69 (1): 39–45. doi:10.1097/OGX.0000000000000017. PMID 25102250.
- Raymond, EG; Harrison, MS; Weaver, MA (January 2019). "Efficacy of Misoprostol Alone for First-Trimester Medical Abortion: A Systematic Review". Obstetrics and Gynecology. 133 (1): 137–147. doi:10.1097/AOG.0000000000003017. PMC 6309472. PMID 30531568.
- Marret, H; Simon, E; Beucher, G; Dreyfus, M; Gaudineau, A; Vayssière, C; Lesavre, M; Pluchon, M; Winer, N; Fernandez, H; Aubert, J; Bejan-Angoulvant, T; Jonville-Bera, AP; Clouqueur, E; Houfflin-Debarge, V; Garrigue, A; Pierre, F; Collège national des gynécologues obstétriciens, français (April 2015). "Overview and expert assessment of off-label use of misoprostol in obstetrics and gynaecology: review and report by the Collège national des gynécologues obstétriciens français". European Journal of Obstetrics, Gynecology, and Reproductive Biology. 187: 80–4. doi:10.1016/j.ejogrb.2015.01.018. PMID 25701235.
- Prager, Sara. "Early Pregnancy Loss" (PDF). ACOG.org. ACOG.
- Blum, J.; Alfirevic, Z.; Walraven, G.; Weeks, A.; Winikoff, B. (December 2007). "Treatment of postpartum hemorrhage with misoprostol". International Journal of Gynecology & Obstetrics. 99: S202–S205. doi:10.1016/j.ijgo.2007.09.013. PMID 17961565.
- Paul, Maureen (2011). "Misoprostol". Management of Unintended and Abnormal Pregnancy: Comprehensive Abortion Care. John Wiley & Sons. ISBN 9781444358476.
- World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- "Misoprostol". International Drug Price Indicator Guide. Archived from the original on 10 May 2017. Retrieved 20 December 2015.
- Hamilton, Richart (2015). Tarascon Pocket Pharmacopoeia 2015 Deluxe Lab-Coat Edition. Jones & Bartlett Learning. p. 271. ISBN 9781284057560.
- "DocMorris - Cytotec 200 µg Tabletten". 6 May 2016. Archived from the original on 6 May 2016. Retrieved 20 May 2016.CS1 maint: unfit url (link)
- Hawkey CJ, Karrasch JA, Szczepañski L, et al. (March 1998). "Omeprazole compared with misoprostol for ulcers associated with nonsteroidal antiinflammatory drugs. Omeprazole versus Misoprostol for NSAID-induced Ulcer Management (OMNIUM) Study Group". N. Engl. J. Med. 338 (11): 727–34. doi:10.1056/NEJM199803123381105. PMID 9494149.
- Wood, Alastair J. J.; Goldberg, Alisa B.; Greenberg, Mara B.; Darney, Philip D. (2001). "Misoprostol and Pregnancy". New England Journal of Medicine. 344 (1): 38–47. doi:10.1056/NEJM200101043440107. PMID 11136959.
- Summers, L (1997). "Methods of cervical ripening and labor induction". Journal of Nurse-Midwifery. 42 (2): 71–85. doi:10.1016/S0091-2182(96)00138-3. PMID 9107114.
- "Ferring's removable misoprostol vaginal delivery system, approved for labour induction in European Decentralised Procedure". Ferring. 17 October 2013. Archived from the original on 3 December 2013. Retrieved 26 November 2013.
- Wing, Deborah. "Misoprostol Vaginal Insert and Time to Vaginal Delivery: A Randomized Controlled Trial". Obstetrics and gynaecology. Wolters Kluwer Health. Archived from the original on 27 May 2014. Retrieved 26 May 2014.
- "Safety Information, Cytotec (misoprostol) Tablets". FDA. 11 December 2012. Archived from the original on 20 January 2017. Retrieved 16 March 2017.
- "WHO | Medical methods for first trimester abortion". apps.who.int. Archived from the original on 14 February 2016. Retrieved 4 February 2016.
- Harvey, S. M.; Beckman, L. J.; Castle, M. A.; Coeytaux, F. (1 October 1995). "Knowledge and perceptions of medical abortion among potential users". Family Planning Perspectives. 27 (5): 203–207. doi:10.2307/2136276. ISSN 0014-7354. JSTOR 2136276. PMID 9104607.
- Bazelon, Emily (28 August 2014). "The Dawn of the Post-Clinic Abortion". The New York Times. ISSN 0362-4331. Archived from the original on 2 March 2016. Retrieved 4 February 2016.
- "Medical methods for first trimester abortion". The WHO Medical Reproductive Library. Archived from the original on 2 August 2014. Retrieved 22 June 2014.
- Organization., World Health (2012). Safe abortion : technical and policy guidance for health systems (Second ed.). Geneva. ISBN 9789241548434. OCLC 812323067.
- What is the "Mexican abortion pill" and how safe is it? Archived 2013-07-30 at the Wayback Machine Jen Gunter, July 27, 2013
- "Annotated Bibliography on Misoprostol Alone for Early Abortion" (PDF). Gynuity Health Projects. Archived from the original (PDF) on 29 September 2007. Retrieved 22 August 2006.
- providing medical abortion in low-resource settings (PDF) (2 ed.). Gynuity Health Projects. 2009. p. 4. Archived from the original (PDF) on 22 February 2016. Retrieved 31 August 2015.
- "Instructions for Use: Abortion Induction with Misoprostol in Pregnancies up to 9 Weeks LMP" (PDF). Gynuity Health Projects. 2003. Archived from the original (PDF) on 29 September 2007. Retrieved 24 August 2006.
- Wu, Hang-lin; Marwah, Sheeba; Wang, Pei; Wang, Qiu-meng; Chen, Xiao-wen (10 May 2017). "Misoprostol for medical treatment of missed abortion: a systematic review and network meta-analysis". Scientific Reports. 7 (1): 1664. doi:10.1038/s41598-017-01892-0. ISSN 2045-2322. PMC 5431938. PMID 28490770.

- "ACOG Practice Bulletin No. 200: Early Pregnancy Loss". Obstetrics and Gynecology. 132 (5): e197–e207. November 2018. doi:10.1097/AOG.0000000000002899. ISSN 1873-233X. PMID 30157093.
- American College of Obstetricians and Gynecologists (March 2014). "Practice bulletin no. 143: medical management of first-trimester abortion". Obstetrics and Gynecology. 123 (3): 676–692. doi:10.1097/01.AOG.0000444454.67279.7d. ISSN 1873-233X. PMID 24553166.
- Lemmers, M; Verschoor, MA; Kim, BV; Hickey, M; Vazquez, JC; Mol, BWJ; Neilson, JP (17 June 2019). "Medical treatment for early fetal death (less than 24 weeks)". The Cochrane Database of Systematic Reviews. 6: CD002253. doi:10.1002/14651858.CD002253.pub4. PMC 6574399. PMID 31206170.
- Villar, J; Gülmezoglu, AM; Hofmeyr, GJ; Forna, F (2002). "Systematic review of randomized controlled trials of misoprostol to prevent postpartum hemorrhage". Obstetrics & Gynecology. 100 (6): 1301–12. doi:10.1016/S0029-7844(02)02371-2. PMID 12468178.
- O'Brien, P; El-Refaey, H; Gordon, A; Geary, M; Rodeck, CH (1998). "Rectally administered misoprostol for the treatment of postpartum hemorrhage unresponsive to oxytocin and ergometrine: A descriptive study". Obstetrics & Gynecology. 92 (2): 212–4. doi:10.1016/S0029-7844(98)00161-6. PMID 9699753.
- Lokugamage, Amali U.; Sullivan, Keith R.; Niculescu, Iosif; Tigere, Patrick; Onyangunga, Felix; Refaey, Hazem El; Moodley, Jagidesa; Rodeck, Charles H. (2001). "A randomized study comparing rectally administered misoprostol versus Syntometrine combined with an oxytocin infusion for the cessation of primary post partum hemorrhage". Acta Obstetricia et Gynecologica Scandinavica. 80 (9): 835–9. doi:10.1034/j.1600-0412.2001.080009835.x. PMID 11531635.
- Bradley, S. E. K.; Prata, N.; Young-Lin, N.; Bishai, D.M. (2007). "Cost-effectiveness of misoprostol to control postpartum hemorrhage in low-resource settings". International Journal of Gynecology & Obstetrics. 97 (1): 52–6. doi:10.1016/j.ijgo.2006.12.005. PMID 17316646.
- Derman, Richard J; Kodkany, Bhalchandra S; Goudar, Shivaprasad S; Geller, Stacie E; Naik, Vijaya A; Bellad, MB; Patted, Shobhana S; Patel, Ashlesha; et al. (2006). "Oral misoprostol in preventing postpartum haemorrhage in resource-poor communities: A randomised controlled trial". The Lancet. 368 (9543): 1248–53. doi:10.1016/S0140-6736(06)69522-6. PMID 17027730.
- Sanghvi, Harshad; Zulkarnain, Mohammad; Chanpong, Gail Fraser (2009). Blouse, Ann; Lewison, Dana (eds.). Prevention of Postpartum Hemorrhage at Home Birth: A Program Implementation Guide (PDF). United States Agency for International Development. Archived (PDF) from the original on 6 December 2013.
- Prata, Ndola; Passano, Paige; Bell, Suzanne; Rowen, Tami; Potts, Malcolm (2012). "New hope: community-based misoprostol use to prevent postpartum haemorrhage". Health Policy and Planning. 28 (4): 339–46. doi:10.1093/heapol/czs068. PMID 22879523.
- Pfizer (September 2006). "Cytotec US Prescribing Information" (PDF). Archived from the original (PDF) on 16 February 2007. Retrieved 15 March 2007.
- Pharmacia (July 2004). "Cytotec UK SPC (Summary of Product Characteristics)". Archived from the original on 28 September 2007. Retrieved 15 March 2007.
- Briggs, G. G.; Wan, SR (2006). "Drug therapy during labor and delivery, part 2". American Journal of Health-System Pharmacy. 63 (12): 1131–9. doi:10.2146/ajhp050265.p2. PMID 16754739.
- Wagner, Marsden (2006). Born in the USA: how a broken maternity system must be fixed to put mothers and infants first. Berkeley: University of California Press. ISBN 0-520-24596-2., which cites:
- Wing DA, Paul RH (July 1996). "A comparison of differing dosing regimens of vaginally administered misoprostol for preinduction cervical ripening and labor induction". Am. J. Obstet. Gynecol. 175 (1): 158–64. doi:10.1016/s0002-9378(96)70267-3. PMID 8694043.
- Wing DA, Rahall A, Jones MM, Goodwin TM, Paul RH (June 1995). "Misoprostol: an effective agent for cervical ripening and labor induction". Am. J. Obstet. Gynecol. 172 (6): 1811–6. doi:10.1016/0002-9378(95)91416-1. PMID 7778637.CS1 maint: multiple names: authors list (link)
- Goldberg & Wing 2003, which cites:
- Weeks, Andrew; Alfirevic, Zarko (2006). "Oral Misoprostol Administration for Labor Induction". Clinical Obstetrics and Gynecology. 49 (3): 658–71. doi:10.1097/00003081-200609000-00023. PMID 16885670.
- Moreno JJ (2017). "Eicosanoid receptors: Targets for the treatment of disrupted intestinal epithelial homeostasis". European Journal of Pharmacology. 796: 7–19. doi:10.1016/j.ejphar.2016.12.004. PMID 27940058.
- Goldberg, A; Wing, D (2003). "Induction of laborthe misoprostol controversy". Journal of Midwifery & Women's Health. 48 (4): 244–8. doi:10.1016/S1526-9523(03)00087-4. PMID 12867908.CS1 maint: ref=harv (link)
- Goldberg & Wing 2003, which cites:
- American College of Obstetricians and Gynecologists (November 1999). "Induction of labor with misoprostol". ACOG Committee Opinion No. 228. Washington, DC.
- American College of Obstetricians and Gynecologists (November 1999). "Response to Searle's drug warning on misoprostol". ACOG Committee Opinion No. 248. Washington, DC.
- "Denver attorney receives 'Case of the Year' honor". Archived from the original on 2 December 2013. Retrieved 3 September 2012.
- Costa, S. H.; Vessey, M. P. (1993). "Misoprostol and illegal abortion in Rio de Janeiro, Brazil". The Lancet. 341 (8855): 1258–61. doi:10.1016/0140-6736(93)91156-G. PMID 8098402.
- Coêlho, Helena Lutéscia; Teixeira, Ana Cláudia; De Fátima Cruz, Maria; Gonzaga, Sandra Luzia; Arrais, Paulo Sérgio; Luchini, Laura; La Vecchia, Carlo; Tognoni, Gianni (1994). "Misoprostol: The experience of women in Fortaleza, Brazil". Contraception. 49 (2): 101–10. doi:10.1016/0010-7824(94)90084-1. PMID 8143449.
- Barbosa, Regina Maria; Arilha, Margareth (1993). "The Brazilian Experience with Cytotec". Studies in Family Planning. 24 (4): 236–40. doi:10.2307/2939191. JSTOR 2939191. PMID 8212093.
- Rocha, J. (1994). "Brazil investigates drug's possible link with birth defects". BMJ. 309 (6957): 757–8. doi:10.1136/bmj.309.6957.757a. PMC 2540993. PMID 7950553.
- Gonzalez, Claudette Hajaj; Vargas, Fernando R.; Perez, Ana Beatriz Alvarez; Kim, Chong Ae; Brunoni, Decio; Marques-Dias, Maria Joaquina; Leone, Clea R.; Neto, Jordão Correa; et al. (1993). "Limb deficiency with or without Möbius sequence in seven Brazilian children associated with misoprostol use in the first trimester of pregnancy". American Journal of Medical Genetics. 47 (1): 59–64. doi:10.1002/ajmg.1320470113. PMID 8368254.
- John Leland (2 October 2005). "Abortion Might Outgrow Its Need for Roe v. Wade". The New York Times. Archived from the original on 18 May 2013. Retrieved 6 March 2014.
- Erik Eckholm (13 July 2013). "In Mexican Pill, a Texas Option for an Abortion". The New York Times. Archived from the original on 14 July 2013. Retrieved 14 July 2013.
- Erica Hellenstein (27 June 2014). "The Rise of the DIY Abortion in Texas". The Atlantic. Archived from the original on 2 March 2017.
External links
- "Misoprostol". Drug Information Portal. U.S. National Library of Medicine.
- Misoprostol.org an independent website containing dosage guidelines and advice on misoprostol use.
- The Mechanism of Action and Pharmacology of Mifepristone, Misoprostol, and Methotrexate