Trastuzumab emtansine
 | |
| Monoclonal antibody | |
|---|---|
| Type | Whole antibody |
| Source | Humanized (from mouse) |
| Clinical data | |
| Trade names | Kadcyla, Kadccyla |
| License data | |
| Pregnancy category |
|
| Routes of administration | Intravenous infusion |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | N/A |
| Protein binding | 93% (in vitro) |
| Metabolism | Hepatic (CYP3A4/3A5-mediated) |
| Elimination half-life | 4 days |
| Identifiers | |
| CAS Number | |
| ChemSpider |
|
| UNII | |
| KEGG | |
| Chemical and physical data | |
| Formula | C6448H9948N1720O2012S44·(C47H62ClN4O13S)n |
| Molar mass | 148.5 kg/mol |
| | |
Trastuzumab emtansine[1][2] also known as ado-trastuzumab emtansine and sold under the trade name Kadcyla, is an antibody-drug conjugate consisting of the monoclonal antibody trastuzumab (Herceptin) linked to the cytotoxic agent emtansine (DM1).[3][4][5][6] Trastuzumab alone stops growth of cancer cells by binding to the HER2/neu receptor, whereas DM1 enters cells and destroys them by binding to tubulin.[7] Trastuzumab binding to Her2 prevents homodimerization or heterodimerization (Her2/Her3) of the receptor, ultimately inhibiting the activation of MAPK and PI3K/AKT cellular signalling pathways. Because the monoclonal antibody targets HER2, and HER2 is only over-expressed in cancer cells, the conjugate delivers the toxin specifically to tumor cells.[8] The conjugate is abbreviated T-DM1.
In the EMILIA clinical trial of women with advanced HER2 positive breast cancer who were already resistant to trastuzumab alone, it improved median overall survival by 5.8 months (30.9 months vs. 25.1 months) compared to the combination of lapatinib and capecitabine.[8] Based on that trial, the U.S. Food and Drug Administration (FDA) approved marketing on February 22, 2013.[9][10][11]
Trastuzumab emtansine was developed by Genentech, a subsidiary group of Roche, and is manufactured by Lonza.[12] The planned cost is expected to be $9,800 a month, or $94,000 for a typical course of treatment.[10]
Medical use
In the United States, ado-trastuzumab emtansine was approved specifically for treatment of HER2-positive metastatic breast cancer (mBC) in patients who have been treated previously with trastuzumab and a taxane (paclitaxel or docetaxel), and who have already been treated for mBC or developed tumor recurrence within six months of adjuvant therapy.[13]
Approval was based on the EMILIA study, a phase III clinical trial that compared trastuzumab emtansine versus capecitabine (Xeloda) plus lapatinib (Tykerb) in 991 people with unresectable, locally advanced or metastatic HER2-positive breast cancer who had previously been treated with trastuzumab and taxane chemotherapy. This trial showed improved progression-free survival in patients treated with trastuzumab emtansine (median 9.6 vs. 6.4 months), along with improved overall survival (median 30.9 vs. 25.1 months) and safety.[8]
Clinical trials
Since 2013 there have been some more clinical trials:
- First line treatment for metastatic breast cancer: the MARIANNE study[14] compares taxane (docetaxel or paclitaxel) plus trastuzumab vs T-DM1 vs T-DM1 plus pertuzumab as first-line treatment for people with HER2 positive unresectable locally advanced or metastatic breast cancer; On December 19, 2014, Roche reported the results of the MARIANNE study. Neither Kadcyla-containing treatment significantly improved progression-free survival compared to Herceptin and chemotherapy.[15]
- a phase III trial for HER2+ gastric cancer compares T-DM1 to physician's choice of taxane (docetaxel or paclitaxel).[16] On October 22, 2015, Roche and co-developer ImmunoGen disclosed that Kadcyla had failed to meets its primary endpoint in the Phase II/III GATSBY trial investigating the second line treatment of HER2-positive advanced gastric cancer.[17]
- the TH3RESA study is comparing T-DM1 vs treatment of physician's choice for people with HER2 positive metastatic breast cancer previously treated with trastuzumab and lapatinib.[18] Interim results for TH3RESA suggest a doubling of progression-free survival from 3 months to 6 months.[19]
Adverse effects
During clinical trials, the most common adverse effects of trastuzumab emtansine were fatigue, nausea, musculoskeletal pain, thrombocytopenia (low platelet counts), headache, increased liver enzyme levels, and constipation.[13]
Severe adverse events identified during the EMILIA trial included hepatotoxicity (liver damage), including rare cases of liver failure, hepatic encephalopathy, and nodular regenerative hyperplasia; heart damage (dysfunction of the left ventricle); interstitial lung disease, including acute interstitial pneumonitis; thrombocytopenia; and peripheral neuropathy.[13] Overall, trastuzumab emtansine was better tolerated than the control treatment, a combination of lapatinib (Tykerb) and capecitabine (Xeloda), with 43% of patients in the trastuzumab emtansine group experiencing severe toxic effects, versus 59% of those who received lapatinib/capecitabine; furthermore, fewer patients had to stop treatment due to adverse effects than with lapatinib or capecitabine.[13] Anemia, low platelet counts, and peripheral neuropathy were more common among patients who received trastuzumab emtansine, whereas heart damage and gastrointestinal effects, such as vomiting, diarrhea, and stomatitis, were more common with lapatinib/capecitabine.[13]
In the United States, Kadcyla carries black box warnings for liver toxicity, heart damage (reduction in left ventricular ejection fraction), and fetal harm if given to pregnant women.[13]
UK pricing issues
In the UK, Kadcyla was not recommended for use by the National Health Service by advisory body NICE, reportedly because an acceptable pricing agreement could not be reached with Roche.[20] Originally it cost £5,900 a month.[21] and NICE estimated it cost £166,000 per QALY[22] (well over the usual maximum). It has been funded by the English NHS Cancer Drugs Fund but in January 2015 it was proposed to remove it from the approved list.[23] After a secret discount was agreed by Roche the Cancer Drugs Fund will continue to fund it.[21]
In June 2017 the NHS Confederation and NHS Chief Executive Simon Stevens announced that the NHS would be offering Kadcyla to a limited number of women after striking a deal with Roche on the price. [24]
Nomenclature
In the United States, Kadcyla was approved with the generic name "ado-trastuzumab emtansine", rather than the original United States Adopted Name (USAN) issued in 2009, "trastuzumab emtansine". The "ado-" prefix was added at the request of the FDA to help prevent dispensing errors.[25] During preclinical development and clinical trials, the drug was also known as trastuzumab-DM1 or trastuzumab-MCC-DM1 (after the codename for emtansine), both abbreviated T-DM1, and by the codename PRO132365.[5]
Chemical properties
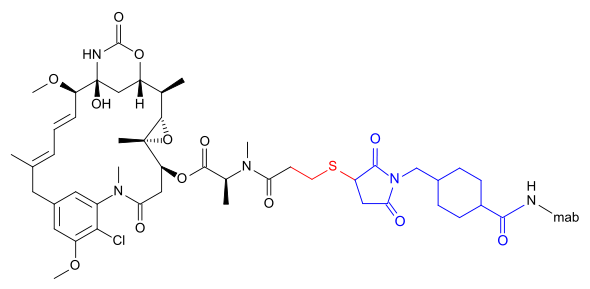
Trastuzumab emtansine is an antibody-drug conjugate (ADC), a combination between a monoclonal antibody and a small-molecule drug. Each molecule of trastuzumab emtansine consists of a single trastuzumab molecule with several molecules of DM1, a cytotoxic maytansinoid, attached.[26] SMCC, or succinimidyl trans-4-(maleimidylmethyl)cyclohexane-1-carboxylate, is a heterobifunctional crosslinker, a type of chemical reagent that contains two reactive functional groups, a succinimide ester and a maleimide. The succinimide group of SMCC reacts with the free amino group of a lysine residue in the trastuzumab molecule and the maleimide moiety of SMCC links to the free sulfhydryl group of DM1, forming a covalent bond between the antibody and the DM1. Each trastuzumab molecule may be linked to zero to eight DM1 molecules (3.5 on average).[26][27] DM1 binds at plus ends of cellular microtubules and thereby inhibits cell division in the target tumor cells.[28]
References
- ↑ Niculescu-Duvaz I (June 2010). "Trastuzumab emtansine, an antibody-drug conjugate for the treatment of HER2+ metastatic breast cancer". Curr. Opin. Mol. Ther. 12 (3): 350–60. PMID 20521224.
- ↑ USAN Council (2009). "Statement On A Nonproprietary Name Adopted By The Usan Council: Trastuzumab Emtansine" (PDF). American Medical Association. Retrieved 2013-02-22.
- ↑ LoRusso PM, Weiss D, Guardino E, Girish S, Sliwkowski MX (October 2011). "Trastuzumab emtansine: a unique antibody-drug conjugate in development for human epidermal growth factor receptor 2-positive cancer". Clin. Cancer Res. 17 (20): 6437–47. doi:10.1158/1078-0432.CCR-11-0762. PMID 22003071.
- ↑ Poon, Kirsten Achilles (2010-05-06). Safety Assessment of Antibody Drug Conjugates (PDF). Drug Development: From Small Molecules to Biologics. NorCal Society of Toxicology 2010 Spring Meeting. Retrieved 2013-02-23.
- 1 2 "Trastuzumab emtansine". NCI Drug Dictionary. Retrieved 2013-02-23.
- ↑ "FDA denies accelerated approval of Genentech's trastuzumab-DM1 (T-DM1) BLA for metastatic breast cancer" (Press release). Genentech. 2010-08-27. Retrieved 2013-02-23.
- ↑ Teicher BA, Doroshow JH (November 2012). "The promise of antibody-drug conjugates". N. Engl. J. Med. 367 (19): 1847–8. doi:10.1056/NEJMe1211736. PMID 23134386.
- 1 2 3 Verma, S; Miles, D; Gianni, L; et al. ( ) (November 2012). "Trastuzumab emtansine for HER2-positive advanced breast cancer". N. Engl. J. Med. 367 (19): 1783–91. doi:10.1056/NEJMoa1209124. PMC 5125250. PMID 23020162.
- ↑ "New data from Phase III EMILIA study showed Roche's trastuzumab emtansine (T-DM1) significantly improved survival of people with HER2-positive metastatic breast cancer" (Press release). Hoffmann-La Roche. 2012-08-27. Retrieved 2013-02-23.
- 1 2 Pollack A (2013-02-22). "F.D.A. Approves a New Drug for Advanced Breast Cancer". The New York Times. Retrieved 2013-02-22.
- ↑ "FDA approves new treatment for late stage breast cancer" (Press release). U.S. Food and Drug Administration. 2013-02-22. Retrieved 2013-02-22.
- ↑ Franklin, Joshua (24 Jul 2014). "Lonza profit boosted by drug production outsourcing". Reuters. Retrieved 28 Jul 2014.
- 1 2 3 4 5 6 "Full Prescribing Information for Kadcyla" (PDF). Genentech. Retrieved 2012-02-23.
- ↑ Clinical trial number NCT01120184 for "A Study of Trastuzumab Emtansine (T-DM1) Plus Pertuzumab/Pertuzumab Placebo Versus Trastuzumab (Herceptin) Plus a Taxane in Patients With Metastatic Breast Cancer (MARIANNE)" at ClinicalTrials.gov. Retrieved 2013-02-23.
- ↑ Roche provides update on Phase III MARIANNE study in people with previously untreated advanced HER2-positive breast cancer (PDF), 2014, retrieved 2015-01-16
- ↑ Clinical trial number NCT01641939 for "A Study of Trastuzumab Emtansine Versus Taxane in Patients With Advanced Gastric Cancer" at ClinicalTrials.gov. Retrieved 2013-02-23.
- ↑ "Roche's Kadcyla Fails Phase II/III Trial for Gastric Cancer". Genetic Engineering & Biotechnology News. October 22, 2015. Retrieved May 26, 2017.
- ↑ Clinical trial number NCT01419197 for "A Study of Trastuzumab Emtansine in Comparison With Treatment of Physician's Choice in Patients With HER2-Positive Breast Cancer Who Have Received at Least Two Prior Regimens of HER2-Directed Therapy (TH3RESA)" at ClinicalTrials.gov. Retrieved 2013-02-23.
- ↑ TDM-1 Heavy Hitter in Heavily Treated Breast Cancer. Oct 2013
- ↑ Triggle, Nick (8 August 2014). "NHS says no to new breast cancer drug Kadcyla". BBC Health News. Retrieved 2014-08-08.
- 1 2 Breast cancer drug Kadcyla to remain on NHS after manufacturer lowers price. Nov 2015
- ↑ Pressure grows on Roche to lower breast cancer drug price. Aug 2014
- ↑ "David Cameron's flagship Cancer Drugs Fund 'is a waste of NHS cash'". Guardian. 10 January 2015. Retrieved 11 January 2015.
- ↑ "NHS U-turn sees breast cancer drug Kadcyla approved for use". NursingNotes. 2017-06-16. Retrieved 2017-06-16.
- ↑ Kim TE, Pazdur R (2013). Summary Review for Regulatory Action (PDF) (Technical report). U.S. Food and Drug Administration. p. 8. Retrieved 2013-02-22.
- 1 2 Girish S, Gupta M, Wang B, et al. (May 2012). "Clinical pharmacology of trastuzumab emtansine (T-DM1): an antibody-drug conjugate in development for the treatment of HER2-positive cancer". Cancer Chemother. Pharmacol. 69 (5): 1229–40. doi:10.1007/s00280-011-1817-3. PMC 3337408. PMID 22271209.
- ↑ Lewis Phillips GD, Li G, Dugger DL, et al. (November 2008). "Targeting HER2-positive breast cancer with trastuzumab-DM1, an antibody-cytotoxic drug conjugate". Cancer Res. 68 (22): 9280–90. doi:10.1158/0008-5472.CAN-08-1776. PMID 19010901.
- ↑ Lopus, Manu (2011). "Antibody-DM1 conjugates as cancer therapeutics". Cancer Letters. 307: 113–118. doi:10.1016/j.canlet.2011.03.017. PMC 3105156. PMID 21481526.