Atorvastatin
 | |
 | |
| Clinical data | |
|---|---|
| Pronunciation | /əˌtɔːrvəˈstætən/ |
| Trade names | Lipitor, Atorva |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a600045 |
| License data |
|
| Pregnancy category | |
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Bioavailability | 12% |
| Metabolism | Hepatic (CYP3A4) |
| Elimination half-life | 14 hours |
| Excretion | Bile |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| PDB ligand | |
| ECHA InfoCard |
100.125.464 |
| Chemical and physical data | |
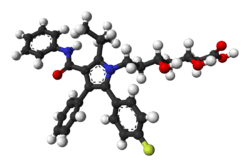
| Formula | C33H35FN2O5 |
| Molar mass | 558.64 |
| 3D model (JSmol) | |
| |
| |
| (verify) | |
Atorvastatin, marketed under the trade name Lipitor among others,[1] is a member of the medication class known as statins, which are used primarily as a lipid-lowering agent and for prevention of events associated with cardiovascular disease. Like all statins, atorvastatin works by inhibiting HMG-CoA reductase, an enzyme found in liver tissue that plays a key role in production of cholesterol in the body.
Atorvastatin was first made in August 1985 at Warner-Lambert's Parke-Davis research facility in Ann Arbor, Michigan[2] by a team led by Bruce Roth.[3][4][5][6][7] From 1996 to 2012 under the trade name Lipitor, atorvastatin became the world's best-selling medication to that point, with more than US$125 billion in sales over approximately 14.5 years.[8] As of 2016, in the UK, atorvastatin costs about £2 per month.[9]
Medical uses
The primary uses of atorvastatin is for the treatment of dyslipidemia and the prevention of cardiovascular disease:[10]
Dyslipidemia
- Hypercholesterolemia[11] (heterozygous familial and nonfamilial) and mixed dyslipidemia (Fredrickson types IIa and IIb) to reduce total cholesterol, LDL-C,[12] apo-B,[13] triglycerides[14] levels, and CRP[15] as well as increase HDL levels.
- Heterozygous familial hypercholesterolemia[11] in pediatric patients
- Homozygous familial hypercholesterolemia[11][16]
- Hypertriglyceridemia (Fredrickson Type IV)
- Primary dysbetalipoproteinemia (Fredrickson Type III)
- Combined hyperlipidemia[17]
Cardiovascular disease
- Primary prevention of heart attack, stroke, and need for revascularization procedures in patients who have risk factors such as age, smoking, high blood pressure, low HDL-C, and a family history of early heart disease, but have not yet developed clinically evident coronary artery disease.[18]
- Secondary prevention of myocardial infarction, stroke, unstable angina,[19][20] and revascularization in people with established coronary artery disease.[21][22]
- Myocardial infarction and stroke prophylaxis in patients with type II diabetes[23][24][25]
Other uses
There have been recent studies suggesting that high-dose statin therapy plays a plaque-stabilizing role in people suffering from acute coronary syndrome and thrombotic stroke.[26][27]
Administration
Atorvastatin may be used in combination with bile acid sequestrants and ezetimibe to increase the reduction in cholesterol levels. However, It is not recommended to combine statin medication treatment with certain other cholesterol-lowering medications, particularly fibrates, because this may increase the risk of myopathy-related adverse effects.[18]
While many statin medications should be administered at bedtime for optimal effect, atorvastatin can be dosed at any time of day, as long as it is continually dosed once daily at the same time.[28][29]
Specific populations
- Geriatric: Plasma concentrations of atorvastatin in healthy elderly subjects are higher than those in young adults, and clinical data suggests a greater degree of LDL-lowering at any dose for patients in the population as compared to young adults.[18]
- Pediatric: Pharmacokinetic data is not available for this population.[18]
- Gender: Plasma concentrations are generally higher in women than in men, but there is no clinically significant difference in the extent of LDL reduction between men and women.[18]
- Renal impairment: Renal disease has no influence on plasma concentrations of atorvastatin and dosing need not be adjusted in these patients.[18]
- Hemodialysis: Hemodialysis will not significantly alter medication levels or change clinical effect of atorvastatin.[18]
- Hepatic impairment: In patients with chronic alcoholic liver disease, levels of atorvastatin may be significantly increased depending upon the extent of liver disease.[18]
Contraindications
- Active liver disease: cholestasis, hepatic encephalopathy, hepatitis, and jaundice
- Unexplained elevations in AST or ALT levels
- Pregnancy: Atorvastatin may cause fetal harm by affecting serum cholesterol and triglyceride levels, which are essential for fetal development.[18]
- Breastfeeding: Small amounts of other statin medications have been found to pass into breast milk, although atorvastatin has not been studied, specifically.[18] Due to risk of disrupting a breastfeeding infant's metabolism of lipids, atorvastatin is not regarded as compatible with breastfeeding.[30]
- Markedly elevated CPK levels or if a myopathy is suspected or diagnosed after dosing of atorvastatin has begun. Very rarely, atorvastatin may cause rhabdomyolysis,[31] and it may be very serious leading to acute renal failure due to myoglobinuria. If rhabdomyolysis is suspected or diagnosed, atorvastatin therapy should be discontinued immediately.[32] The likelihood of developing a myopathy is increased by the co-administration of cyclosporine, fibric acid derivatives, erythromycin, niacin, and azole antifungals.[33]
Adverse effects
Major
- Type 2 diabetes mellitus, an uncommon class effect of all statins.[34][35][36][37]
- Myopathy with elevation of creatine kinase (CK, aka CPK)[38] and rhabdomyolysis are the most serious side effects, occurring rarely at a rate of 2.3 to 9.1 per 10,000 person-years among patients taking atorvastatin.[17][33][39] As mentioned previously, atorvastatin should be discontinued immediately if this occurs.
- Persistent liver enzyme abnormalities occurred in 0.7% of patients who received atorvastatin in clinical trials. It is recommended that hepatic function be assessed with laboratory tests before beginning atorvastatin treatment and repeated as clinically indicated thereafter. If evidence of serious liver injury occurs while a patient is taking atorvastatin, it should be discontinued and not restarted until the etiology of the patient's liver dysfunction is defined. If no other cause is found, atorvastatin should be discontinued permanently.[18]
Common
The following have been shown to occur in 1–10% of patients taking atorvastatin in clinical trials:
High-dose atorvastatin have also been associated with worsening blood sugar control.[40][41]
Other
In 2014, the Food and Drug Administration (FDA) reported memory loss, forgetfulness and confusion with all statin products including atorvastatin. The symptoms were not serious, and they were rare and reversible on cessation of treatment with the medication.[34]
Interactions
Interactions with clofibrate, fenofibrate, gemfibrozil, which are fibrates used in accessory therapy in many forms of hypercholesterolemia, usually in combination with statins, increase the risk of myopathy and rhabdomyolysis.[38][42][43]
Co-administration of atorvastatin with one of CYP3A4 inhibitors such as itraconazole,[44] telithromycin, and voriconazole, may increase serum concentrations of atorvastatin, which may lead to adverse reactions. This is less likely to happen with other CYP3A4 inhibitors such as diltiazem, erythromycin, fluconazole, ketoconazole, clarithromycin, cyclosporine, protease inhibitors, or verapamil,[45] and only rarely with other CYP3A4 inhibitors, such as amiodarone and aprepitant.[32] Often, bosentan, fosphenytoin, and phenytoin, which are CYP3A4 inducers, can decrease the plasma concentrations of atorvastatin. Only rarely, though, barbiturates, carbamazepine, efavirenz, nevirapine, oxcarbazepine, rifampin, and rifamycin,[46] which are also CYP3A4 inducers, can decrease the plasma concentrations of atorvastatin. Oral contraceptives increased AUC values for norethisterone and ethinylestradiol; these increases should be considered when selecting an oral contraceptive for a woman taking atorvastatin.[47]
Antacids can rarely decrease the plasma concentrations of statin medications, but do not affect the LDL-C-lowering efficacy.[48]
Niacin also is proved to increase the risk of myopathy or rhabdomyolysis.[32]
Some statins may also alter the concentrations of other medications, such as warfarin or digoxin, leading to alterations in effect or a requirement for clinical monitoring.[32] The increase in digoxin levels due to atorvastatin is a 1.2 fold elevation in the area under the curve (AUC), resulting in a minor drug-drug interaction. The American Heart Association states that the combination of digoxin and atorvastatin is reasonable.[49] In contrast to some other statins, atorvastatin does not interact with warfarin concentrations in a clinically meaningful way (similar to pitavastatin).[49]
Vitamin D supplementation lowers atorvastatin and active metabolite concentrations, yet synergistically reduces LDL and total cholesterol concentrations.[50] Grapefruit juice components are known inhibitors of intestinal CYP3A4.
Co-administration of grapefruit juice with atorvastatin may cause an increase in Cmax and AUC, which can lead to adverse reactions or overdose toxicity.[51]
A few cases of myopathy have been reported when atorvastatin is given with colchicine.[18]
Mechanism of action
As with other statins, atorvastatin is a competitive inhibitor of HMG-CoA reductase. Unlike most others, however, it is a completely synthetic compound. HMG-CoA reductase catalyzes the reduction of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG-CoA) to mevalonate, which is the rate-limiting step in hepatic cholesterol biosynthesis. Inhibition of the enzyme decreases de novo cholesterol synthesis, increasing expression of low-density lipoprotein receptors (LDL receptors) on hepatocytes. This increases LDL uptake by the hepatocytes, decreasing the amount of LDL-cholesterol in the blood. Like other statins, atorvastatin also reduces blood levels of triglycerides and slightly increases levels of HDL-cholesterol.
Recent studies have shown that in patients suffering from acute coronary syndrome, high-dose statin treatment may play a plaque-stabilizing role. At high doses, statins have anti-inflammatory effects, incite reduction of the necrotic plaque core, and improve endothelial function, leading to plaque stabilization and, sometimes, plaque regression. However, there is an increased risk of statin-associated adverse effects with such high-dose statin treatment.[26] There is a similar thought process and risks associated with using high-dose statins to prevent recurrence of thrombotic stroke.[27]
Pharmacodynamics
The liver is the primary site of action of atorvastatin, as this is the principal site of both cholesterol synthesis and LDL clearance. It is the dosage of atorvastatin, rather than systemic medication concentration, which correlates with extent of LDL-C reduction.[18] In a Cochrane systematic review the dose-related magnitude of atorvastatin on blood lipids was determined. Over the dose range of 10 to 80 mg/day total cholesterol was reduced by 27.0% to 37.9%, LDL cholesterol by 37.1% to 51.7% and triglycerides by 18.0% to 28.3%.[52]
Pharmacokinetics
Absorption
Atorvastatin undergoes rapid absorption when taken orally, with an approximate time to maximum plasma concentration (Tmax) of 1–2 h. The absolute bioavailability of the medication is about 14%, but the systemic availability for HMG-CoA reductase activity is approximately 30%. Atorvastatin undergoes high intestinal clearance and first-pass metabolism, which is the main cause for the low systemic availability. Administration of atorvastatin with food produces a 25% reduction in Cmax (rate of absorption) and a 9% reduction in AUC (extent of absorption), although food does not affect the plasma LDL-C-lowering efficacy of atorvastatin. Evening dose administration is known to reduce the Cmax and AUC by 30% each. However, time of administration does not affect the plasma LDL-C-lowering efficacy of atorvastatin.
Distribution
The mean volume of distribution of atorvastatin is approximately 381 L. It is highly protein bound (≥98%), and studies have shown it is likely secreted into human breastmilk.
Metabolism
Atorvastatin metabolism is primarily through cytochrome P450 3A4 hydroxylation to form active ortho- and parahydroxylated metabolites, as well as various beta-oxidation metabolites. The ortho- and parahydroxylated metabolites are responsible for 70% of systemic HMG-CoA reductase activity. The ortho-hydroxy metabolite undergoes further metabolism via glucuronidation. As a substrate for the CYP3A4 isozyme, it has shown susceptibility to inhibitors and inducers of CYP3A4 to produce increased or decreased plasma concentrations, respectively. This interaction was tested in vitro with concurrent administration of erythromycin, a known CYP3A4 isozyme inhibitor, which resulted in increased plasma concentrations of atorvastatin. It is also an inhibitor of cytochrome 3A4.
Excretion
Atorvastatin is primarily eliminated via hepatic biliary excretion, with less than 2% recovered in the urine. Bile elimination follows hepatic and/or extrahepatic metabolism. There does not appear to be any entero-hepatic recirculation. Atorvastatin has an approximate elimination half-life of 14 hours. Noteworthy, the HMG-CoA reductase inhibitory activity appears to have a half-life of 20–30 hours, which is thought to be due to the active metabolites. Atorvastatin is also a substrate of the intestinal P-glycoprotein efflux transporter, which pumps the medication back into the intestinal lumen during medication absorption.[32]
In hepatic insufficiency, plasma concentrations of atorvastatin are significantly affected by concurrent liver disease. Patients with Child-Pugh Stage A liver disease show a four-fold increase in both Cmax and AUC. People with Child Pugh stage B liver disease show a 16-fold increase in Cmax and an 11-fold increase in AUC.
Geriatric patients (>65 years old) exhibit altered pharmacokinetics of atorvastatin compared to young adults, with mean AUC and Cmax values that are 40% and 30% higher, respectively. Additionally, healthy elderly patients show a greater pharmacodynamic response to atorvastatin at any dose; therefore, this population may have lower effective doses.[33]
Pharmacogenetics
Several genetic polymorphisms have been found to be associated with a higher incidence of undesirable side effects of atorvastatin. This phenomenon is suspected to be related to increased plasma levels of pharmacologically active metabolites, such as atorvastatin lactone and p-hydroxyatorvastatin. Atorvastatin and its active metabolites may be monitored in potentially susceptible patients using specific chromatographic techniques.[53]
Chemical synthesis


The first synthesis of atorvastatin at Parke-Davis that occurred during drug discovery was racemic followed by chiral chromatographic separation of the enantiomers. An early enantioselective route to atorvastatin made use of an ester chiral auxiliary to set the stereochemistry of the first of the two alcohol functional groups via a diastereoselective aldol reaction.[3][54]
Once the compound entered pre-clinical development, process chemistry developed a cost-effective and scalable synthesis.[3] In atorvastatin's case, a key element of the overall synthesis was ensuring stereochemical purity in the final drug substance, and hence establishing the first stereocenter became a key aspect of the overall design. The final commercial production of atorvastatin relied on a chiral pool approach, where the stereochemistry of the first alcohol functional group was carried into the synthesis—through the choice of isoascorbic acid, an inexpensive and easily sourced plant-derived natural product.[3][55]
History
Bruce Roth, who was hired by Warner-Lambert as a chemist in 1982, had synthesized an "experimental compound" codenamed CI 981 – later called atorvastatin.[4][56] Warner-Lambert management was concerned that atorvastatin was a me-too version of rival Merck & Co.'s orphan drug lovastatin (brand name Mevacor). Mevacor, which was first marketed in 1987, was the industry's first statin and Merck's synthetic version – simvastatin – was in the advanced stages of development.[56] Nevertheless, Bruce Roth and his bosses, Roger Newton and Ronald Cresswell, in 1985 convinced company executives to move the compound into expensive clinical trials. Early results comparing atorvastatin vs. simvastatin demonstrated that atorvastatin was significantly more potent and displayed fewer side effects.[56]
In 1994 the findings of a Merck-funded study were published in The Lancet concluding the efficacy of statins in lowering cholesterol in 4444 Scandinavian patients proving for the first time not only that a "statin reduced 'bad' LDL cholesterol but also that it led to a sharp drop in fatal heart attacks among patients with heart disease."[56][57] In 1996 Warner-Lambert entered into a co-marketing agreement with Pfizer to sell Lipitor and in 2000 Pfizer acquired Warner-Lambert 2000 for $90.2 billion.[2][3][5][6] Lipitor was on the market by 1996.[7][58] By 2003 Lipitor had become the best selling pharmaceutical in the United States.[4] From 1996 to 2012 under the trade name Lipitor, atorvastatin became the world's best-selling medication of all time, with more than $125 billion in sales over approximately 14.5 years.[8] Lipitor alone "provided up to a quarter of Pfizer Inc.'s annual revenue for years."[8]
Pfizer's patent on atorvastatin expired in November 2011.[59]
Formulations

Atorvastatin calcium tablets are marketed by Pfizer under the trade name Lipitor[60] for oral administration. Tablets are white, elliptical, and film-coated. Pfizer also packages the medication in combination with other medications, such as with amlodipine (brand name Caduet).[61] Pfizer recommends that patients do not break tablets in half to take half-doses, even when this is recommended by their doctors.[33]
Generic availability
Pfizer's US patent on Lipitor expired on 30 November 2011.[59] Initially, generic atorvastatin was manufactured only by Watson Pharmaceuticals and India's Ranbaxy Laboratories. Prices for the generic version did not drop to the level of other generics—$10 or less for a month's supply—until other manufacturers began to supply the medication in May 2012.[62]
In other countries, atorvastatin calcium is made in tablet form by generic medication makers under various brand names including Stator, Atorvastatin Teva, Litorva, Torid, Atoris, Atorlip, Mactor, Lipvas, Sortis, Torvast, Torvacard, Totalip, and Tulip.[63] Pfizer also makes its own generic version under the name Zarator.[64]
Medication recalls
On 9 November 2012, Indian drugmaker Ranbaxy Laboratories Ltd. voluntarily recalled 10-, 20- and 40-mg doses of its generic version of atorvastatin in the United States.[65][66] The lots of atorvastatin, packaged in bottles of 90 and 500 tablets, were recalled due to possible contamination with very small glass particles similar to the size of a grain of sand (less than 1 mm in size). The FDA received no reports of injury from the contamination.[67] Ranbaxy also issued recalls of bottles of 10-milligram tablets in August 2012 and March 2014, due to concerns that the bottles might contain larger, 20-milligram tablets and thus cause potential dosing errors.[68][69]
References
- ↑ "Pfizer product promotion page (Lipitor)". Retrieved 2011-12-05.
- 1 2 Winslow, Ron (2000-01-24). "The Birth of a Blockbuster: Lipitor's Route out of the Lab". The Wall Street Journal. Retrieved 2011-10-26.
- 1 2 3 4 5 Roth BD (2002). "The discovery and development of atorvastatin, a potent novel hypolipidemic agent". Progress in Medicinal Chemistry. Progress in Medicinal Chemistry. 40: 1–22. doi:10.1016/S0079-6468(08)70080-8. ISBN 978-0-444-51054-9. PMID 12516521.
- 1 2 3 Simons, John (20 January 2003). "The $10 Billion Pill Hold the fries, please. Lipitor, the cholesterol-lowering medication, has become the bestselling pharmaceutical in history. Here's how Pfizer did it". Fortune.
- 1 2 US patent 4681893, Roth Bruce D., "Trans-6-[2-(3- or 4-carboxamido-substituted pyrrol-1-yl)alkyl]-4-hydroxypyran-2-one inhibitors of cholesterol synthesis", issued 1987-07-21
- 1 2 Hoefle ML (2000). "The Early History of Parke-Davis and Company" (PDF). Bull. Hist. Chem. 25 (1): 28–34.
- 1 2 "Pfizer Gets Its Deal to Buy Warner-Lambert for $90.2 Billion". The New York Times. 2000.
- 1 2 3 "Lipitor becomes world's top-selling drug". Crain's New York Business via Associated Press. 28 December 2011. Retrieved 24 November 2011.
- ↑ Collins R, Reith C, Emberson J, Armitage J, Baigent C, Blackwell L, et al. (September 2016). "Interpretation of the evidence for the efficacy and safety of statin therapy". Lancet. 388: 2532–2561. doi:10.1016/S0140-6736(16)31357-5. PMID 27616593.
- ↑ "Atorvastatin Calcium". Drugs.com. Retrieved 3 April 2011.
- 1 2 3 McCrindle BW, Ose L, Marais AD (July 2003). "Efficacy and safety of atorvastatin in children and adolescents with familial hypercholesterolemia or severe hyperlipidemia: a multicenter, randomized, placebo-controlled trial". The Journal of Pediatrics. 143 (1): 74–80. doi:10.1016/S0022-3476(03)00186-0. PMID 12915827.
- ↑ Nissen SE, Nicholls SJ, Sipahi I, Libby P, Raichlen JS, Ballantyne CM, Davignon J, Erbel R, Fruchart JC, Tardif JC, Schoenhagen P, Crowe T, Cain V, Wolski K, Goormastic M, Tuzcu EM (April 2006). "Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial". JAMA. 295 (13): 1556–65. doi:10.1001/jama.295.13.jpc60002. PMID 16533939.
- ↑ Nawrocki JW, Weiss SR, Davidson MH, Sprecher DL, Schwartz SL, Lupien PJ, Jones PH, Haber HE, Black DM (May 1995). "Reduction of LDL cholesterol by 25% to 60% in patients with primary hypercholesterolemia by atorvastatin, a new HMG-CoA reductase inhibitor". Arteriosclerosis, Thrombosis, and Vascular Biology. 15 (5): 678–82. doi:10.1161/01.ATV.15.5.678. PMID 7749881.
- ↑ Bakker-Arkema RG, Davidson MH, Goldstein RJ, Davignon J, Isaacsohn JL, Weiss SR, Keilson LM, Brown WV, Miller VT, Shurzinske LJ, Black DM (January 1996). "Efficacy and safety of a new HMG-CoA reductase inhibitor, atorvastatin, in patients with hypertriglyceridemia". JAMA. 275 (2): 128–33. doi:10.1001/jama.1996.03530260042029. PMID 8531308.
- ↑ Ozaki K, Kubo T, Imaki R, Shinagawa H, Fukaya H, Ohtaki K, Ozaki S, Izumi T, Aizawa Y (August 2006). "The anti-atherosclerotic effects of lipid lowering with atorvastatin in patients with hypercholesterolemia". Journal of Atherosclerosis and Thrombosis. 13 (4): 216–9. doi:10.5551/jat.13.216. PMID 16908955.
- ↑ Marais AD, Firth JC, Bateman ME, Byrnes P, Martens C, Mountney J (August 1997). "Atorvastatin: an effective lipid-modifying agent in familial hypercholesterolemia". Arteriosclerosis, Thrombosis, and Vascular Biology. 17 (8): 1527–31. doi:10.1161/01.ATV.17.8.1527. PMID 9301631.
- 1 2 Rossi S, ed. (2006). Australian medicines handbook 2006. Adelaide, S. Aust: Australian Medicines Handbook Pty Ltd. ISBN 0-9757919-2-3.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 "LIPITOR (atorvastatin calcium) Tablets for oral administration" (PDF). Full Prescribing Information. Pfizer Inc. Retrieved 18 April 2014.
- ↑ Sever PS, Dahlöf B, Poulter NR, Wedel H, Beevers G, Caulfield M, Collins R, Kjeldsen SE, Kristinsson A, McInnes GT, Mehlsen J, Nieminen M, O'Brien E, Ostergren J (April 2003). "Prevention of coronary and stroke events with atorvastatin in hypertensive patients who have average or lower-than-average cholesterol concentrations, in the Anglo-Scandinavian Cardiac Outcomes Trial--Lipid Lowering Arm (ASCOT-LLA): a multicentre randomised controlled trial". Lancet. 361 (9364): 1149–58. doi:10.1016/S0140-6736(03)12948-0. PMID 12686036.
- ↑ Law MR, Wald NJ, Rudnicka AR (June 2003). "Quantifying effect of statins on low density lipoprotein cholesterol, ischaemic heart disease, and stroke: systematic review and meta-analysis". BMJ. 326 (7404): 1423. doi:10.1136/bmj.326.7404.1423. PMC 162260. PMID 12829554.
- ↑ Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB (May 1998). "Prediction of coronary heart disease using risk factor categories" (PDF). Circulation. 97 (18): 1837–47. doi:10.1161/01.CIR.97.18.1837. PMID 9603539.
- ↑ Jones P, Kafonek S, Laurora I, Hunninghake D (March 1998). "Comparative dose efficacy study of atorvastatin versus simvastatin, pravastatin, lovastatin, and fluvastatin in patients with hypercholesterolemia (the CURVES study)". The American Journal of Cardiology. 81 (5): 582–7. doi:10.1016/S0002-9149(97)00965-X. PMID 9514454.
- ↑ Colhoun HM, Betteridge DJ, Durrington PN, Hitman GA, Neil HA, Livingstone SJ, Thomason MJ, Mackness MI, Charlton-Menys V, Fuller JH (2004). "Primary prevention of cardiovascular disease with atorvastatin in type 2 diabetes in the Collaborative Atorvastatin Diabetes Study (CARDS): multicentre randomised placebo-controlled trial". Lancet. 364 (9435): 685–96. doi:10.1016/S0140-6736(04)16895-5. PMID 15325833.
- ↑ Neil HA, DeMicco DA, Luo D, Betteridge DJ, Colhoun HM, Durrington PN, Livingstone SJ, Fuller JH, Hitman GA (November 2006). "Analysis of efficacy and safety in patients aged 65-75 years at randomization: Collaborative Atorvastatin Diabetes Study (CARDS)". Diabetes Care. 29 (11): 2378–84. doi:10.2337/dc06-0872. PMID 17065671.
- ↑ Gentile S, Turco S, Guarino G, Sasso CF, Amodio M, Magliano P, Salvatore T, Corigliano G, Agrusta M, De Simone G, Gaeta I, Oliviero B, Torella R (December 2000). "Comparative efficacy study of atorvastatin vs simvastatin, pravastatin, lovastatin and placebo in type 2 diabetic patients with hypercholesterolaemia". Diabetes, Obesity & Metabolism. 2 (6): 355–62. doi:10.1046/j.1463-1326.2000.00106.x. PMID 11225965.
- 1 2 Rosa GM, Carbone F, Parodi A, Massimelli EA, Brunelli C, Mach F, Vuilleumier N, Montecucco F (May 2014). "Update on the efficacy of statin treatment in acute coronary syndromes". European Journal of Clinical Investigation. 44 (5): 501–15. doi:10.1111/eci.12255. PMID 24601937.
- 1 2 Furie KL (July 2012). "High-dose statins should only be used in atherosclerotic strokes". Stroke: A Journal of Cerebral Circulation. 43 (7): 1994–5. doi:10.1161/STROKEAHA.111.633339. PMID 22581818.
- ↑ "Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III)". JAMA. 285 (19): 2486–97. May 2001. doi:10.1001/jama.285.19.2486. PMID 11368702.
- ↑ Grundy SM, Cleeman JI, Merz CN, Brewer HB, Clark LT, Hunninghake DB, Pasternak RC, Smith SC, Stone NJ (July 2004). "Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines". Circulation. 110 (2): 227–39. doi:10.1161/01.CIR.0000133317.49796.0E. PMID 15249516.
- ↑ "TOXNET". toxnet.nlm.nih.gov. U.S. National Library of Medicine. Retrieved 29 May 2018.
- ↑ Hermann M, Bogsrud MP, Molden E, Asberg A, Mohebi BU, Ose L, Retterstøl K (June 2006). "Exposure of atorvastatin is unchanged but lactone and acid metabolites are increased several-fold in patients with atorvastatin-induced myopathy". Clinical Pharmacology and Therapeutics. 79 (6): 532–9. doi:10.1016/j.clpt.2006.02.014. PMID 16765141.
- 1 2 3 4 5 Williams D, Feely J (2002). "Pharmacokinetic-pharmacodynamic drug interactions with HMG-CoA reductase inhibitors". Clinical Pharmacokinetics. 41 (5): 343–70. doi:10.2165/00003088-200241050-00003. PMID 12036392.
- 1 2 3 4 5 6 7 8 9 Lipitor: Prescribing Information. Pfizer. June 2009.
- 1 2 "FDA Expands Advice on Statin Risks". Food and Drug Administration (FDA). 31 January 2014. Retrieved 24 November 2015.
- ↑ "Controlling Cholesterol with Statins". Food and Drug Administration (FDA). 6 November 2017. Retrieved 29 December 2017.
- ↑ Salynn, Boyles (9 January 2012), Statins May Raise Diabetes Risk in Older Women: Study: Middle-Aged, Older Statin Users Had More Type 2 Diabetes, WebMD Health News, retrieved 24 November 2015
- ↑ Statins and Risk of New-Onset Diabetes Mellitus | Circulation
- 1 2 Ghirlanda G, Oradei A, Manto A, Lippa S, Uccioli L, Caputo S, Greco AV, Littarru GP (March 1993). "Evidence of plasma CoQ10-lowering effect by HMG-CoA reductase inhibitors: a double-blind, placebo-controlled study". Journal of Clinical Pharmacology. 33 (3): 226–9. doi:10.1002/j.1552-4604.1993.tb03948.x. PMID 8463436.
- ↑ Macedo AF, Taylor FC, Casas JP, Adler A, Prieto-Merino D, Ebrahim S (March 2014). "Unintended effects of statins from observational studies in the general population: systematic review and meta-analysis". BMC Medicine. 12: 51. doi:10.1186/1741-7015-12-51. PMC 3998050. PMID 24655568.
- ↑ Mayo Clinic Staff. "Statin Side Effects: Weigh the Risks and Benefits". The Mayo Clinic. Retrieved 19 April 2014.
- ↑ Kostapanos MS, Liamis GL, Milionis HJ, Elisaf MS (September 2010). "Do statins beneficially or adversely affect glucose homeostasis?". Current Vascular Pharmacology. 8 (5): 612–31. doi:10.2174/157016110792006879. PMID 20507274.
- ↑ Steiner G (December 2007). "Atherosclerosis in type 2 diabetes: a role for fibrate therapy?". Diabetes & Vascular Disease Research. 4 (4): 368–74. doi:10.3132/dvdr.2007.067. PMID 18158710.
- ↑ Graham DJ, Staffa JA, Shatin D, Andrade SE, Schech SD, La Grenade L, Gurwitz JH, Chan KA, Goodman MJ, Platt R (December 2004). "Incidence of hospitalized rhabdomyolysis in patients treated with lipid-lowering drugs". JAMA. 292 (21): 2585–90. doi:10.1001/jama.292.21.2585. PMID 15572716.
- ↑ Mazzu AL, Lasseter KC, Shamblen EC, Agarwal V, Lettieri J, Sundaresen P (October 2000). "Itraconazole alters the pharmacokinetics of atorvastatin to a greater extent than either cerivastatin or pravastatin". Clinical Pharmacology and Therapeutics. 68 (4): 391–400. doi:10.1067/mcp.2000.110537. PMID 11061579.
- ↑ Neuvonen PJ, Niemi M, Backman JT (December 2006). "Drug interactions with lipid-lowering drugs: mechanisms and clinical relevance". Clinical Pharmacology and Therapeutics. 80 (6): 565–81. doi:10.1016/j.clpt.2006.09.003. PMID 17178259.
- ↑ Backman JT, Luurila H, Neuvonen M, Neuvonen PJ (August 2005). "Rifampin markedly decreases and gemfibrozil increases the plasma concentrations of atorvastatin and its metabolites". Clinical Pharmacology and Therapeutics. 78 (2): 154–67. doi:10.1016/j.clpt.2005.04.007. PMID 16084850.
- ↑ "Lipitor". U.S. National Library of Medicine.
- ↑ McKenney JM (May 2005). "Efficacy and safety of rosuvastatin in treatment of dyslipidemia". American Journal of Health-System Pharmacy. 62 (10): 1033–47. PMID 15901588.
- 1 2 Wiggins, Barbara S.; Saseen, Joseph J.; Page, Robert L.; Reed, Brent N.; Sneed, Kevin; Kostis, John B.; Lanfear, David; Virani, Salim; Morris, Pamela B. (22 November 2016). "Recommendations for Management of Clinically Significant Drug-Drug Interactions With Statins and Select Agents Used in Patients With Cardiovascular Disease: A Scientific Statement From the American Heart Association". Circulation. 134 (21): e468–e495. doi:10.1161/CIR.0000000000000456.
- ↑ Schwartz JB (February 2009). "Effects of vitamin D supplementation in atorvastatin-treated patients: a new drug interaction with an unexpected consequence". Clinical Pharmacology and Therapeutics. 85 (2): 198–203. doi:10.1038/clpt.2008.165. PMID 18754003.
- ↑ Kane GC, Lipsky JJ (September 2000). "Drug-grapefruit juice interactions". Mayo Clinic Proceedings. 75 (9): 933–42. doi:10.4065/75.9.933. PMID 10994829.
- ↑ Adams, Stephen P.; Tsang, Michael; Wright, James M. (2015-03-11). Lipid-lowering efficacy of atorvastatin. Cochrane Database of Systematic Reviews. John Wiley & Sons, Ltd. doi:10.1002/14651858.cd008226.pub3.
- ↑ Deshmukh HA, Colhoun HM, Johnson T, McKeigue PM, Betteridge DJ, Durrington PN, Fuller JH, Livingstone S, Charlton-Menys V, Neil A, Poulter N, Sever P, Shields DC, Stanton AV, Chatterjee A, Hyde C, Calle RA, Demicco DA, Trompet S, Postmus I, Ford I, Jukema JW, Caulfield M, Hitman GA (May 2012). "Genome-wide association study of genetic determinants of LDL-c response to atorvastatin therapy: importance of Lp(a)". Journal of Lipid Research. 53 (5): 1000–11. doi:10.1194/jlr.P021113. PMC 3329377. PMID 22368281.
- ↑ Roth BD, Blankley CJ, Chucholowski AW, Ferguson E, Hoefle ML, Ortwine DF, Newton RS, Sekerke CS, Sliskovic DR, Wilson M (1991). "Inhibitors of Cholesterol Biosynthesis. 3. Tetrahydro-4-hydroxy-6-[2-(1H-pyrrol-1-yl)ethyl]-2H-pyran 2-one Inhibitors of HMG-CoA Reductase. 2. Effects of Introducing Substituents at Positions Three and Four of the Pyrrole Nucleus". J. Med. Chem. 34: 357–366. doi:10.1021/jm00105a056.
- ↑ Jie Jack Li; Douglas S. Johnson; Drago R. Sliskovic; Bruce D. Roth (2004). "Chapter 9. Atorvastatin Calcium (Lipitor)". Contemporary Drug Synthesis. John Wiley & Sons, Inc. pp. 113–125. ISBN 0-471-21480-9.
- 1 2 3 4 Andrew, Jack (28 November 2009). "The fall of the world's best-selling drug". Financial Times. Retrieved 24 November 2015.
- ↑ "www.accessdata.fda.gov".
- 1 2 CNN Wire Staff (30 November 2011). "Lipitor loses patent, goes generic". CNN. Retrieved 18 November 2012.
- ↑ Medical Product Reviews. "Atorvastatin Calcium (Lipitor Tablets) - Uses, Dosage and Side Effects". Retrieved 3 May 2012.
- ↑ News Medical. "Lipitor - What is Lipitor?". Retrieved 3 May 2012.
- ↑ "Price to UK for 28 tablets from £3.25 (10mg) to £10.00 (80mg)". National Health Service. June 2012. Archived from the original on 20 September 2012. Retrieved 31 July 2012.
- ↑ "Pfizer 2008 Annual Report" (PDF). Pfizer. 23 April 2009. Retrieved 7 August 2009.
- ↑ Rapley, Lisa (31 May 2012). "Atorvastatin sole funding announced". PharmacyToday.co.nz. Archived from the original on 17 July 2014. Retrieved 16 July 2014.
- ↑ "Ranbaxy recalls generic Lipitor doses", Associated Press in Chicago Sun-Times, 23 November 2012 – via HighBeam Research (subscription required)
- ↑ Johnson, Linda A. (24 November 2012). "Ranbaxy recalls generic Lipitor doses". The Boston Globe. Associated Press. Retrieved 29 December 2017.
- ↑ "FDA Statement on Ranbaxy Atorvastatin Recall". FDA. 30 December 2012. Retrieved 19 April 2014.
- ↑ Loftus, Peter (7 March 2014). "Ranbaxy Recalls More Than 64,000 Bottles of Generic Lipitor in U.S.". The Wall Street Journal.
- ↑ Siddiqui, Zeba; Sikka, Kanika (8 March 2014). "Indian drugmaker Ranbaxy recalls more than 64,000 bottles of its generic version of Lipitor". The Washington Post. Retrieved 29 December 2017.
Further reading
- "Highlights of prescribing information" (PDF). Lipitor (atorvastatin calcium) Tablets for oral administration. Pfizer. 2009-06-01. Retrieved 2011-10-26.
- Maggon K (June 2005). "Best-selling human medicines 2002-2004". Drug Discovery Today. 10 (11): 739–42. doi:10.1016/S1359-6446(05)03468-9. PMID 15922927.
- Simons J (2003-01-20). "The $10 Billion Pill Hold the fries, please. Lipitor, the cholesterol-lowering drug, has become the bestselling pharmaceutical in history. Here's how Pfizer did it". Fortune. Retrieved 2011-10-26.
- Winslow, Ron (2000-01-24). "The Birth of a Blockbuster: Lipitor's Route out of the Lab". The Wall Street Journal. Retrieved 2011-10-26.
- "Ann Arbor chemist wins national award for drug discovery". ScienceBlog. American Chemical Society. 2003-03-01. Retrieved 2011-10-26.
- Rowe A (2008-08-20). "Meet the Guy Who Invented Lipitor". Wired. Retrieved 2011-10-26.
- Bernstein M (2008-08-16). "Chemical Society To Honor 'Heroes Of Chemistry' During National Meeting". Medical News Today. Retrieved 2011-10-26.
- He L (2003-09-27). "Bruce D. Roth, Pfizer Inc, USA". Chinese Academy of Sciences·Institute of Process Engineering. Retrieved 2011-10-26.
External links
- Atorvastatin bound to proteins in the PDB
- Lipitor.com – manufacturer's site
- MedlinePlus Drug information: Atorvastatin (Systemic) – information from USP DI Advice for the Patient
- U.S. National Library of Medicine: Drug Information Portal - Atorvastatin