Asystole
| Asystole | |
|---|---|
| Synonyms | Beau's syndrome |
|
| |
| A rhythm strip showing two beats of normal sinus rhythm followed by an atrial beat and asystole | |
| Pronunciation |
|
| Classification and external resources | |
| Specialty | Cardiology |
| ICD-10 | I46.0 |
| ICD-9-CM | 427.5 |
Asystole (1860, from Modern Latin, from Greek privative a "not, without" + systolē "contraction")[1][2] is the absence of ventricular contractions. Asystole is the most serious form of cardiac arrest and is usually irreversible. A cardiac flatline is the state of total cessation of electrical activity from the heart, which means no tissue contraction from the heart muscle and therefore no blood flow to the rest of the body.
Asystole should not be confused with very brief pauses in the heart's electrical activity, even those that produce a temporary flat line, in electrical activity that can occur in certain less severe abnormal rhythms. Asystole is different from very fine occurrences of ventricular fibrillation, though both have a poor prognosis, and untreated fine VF will lead to asystole. Faulty wiring, disconnection of electrodes and leads, and power disruptions should be ruled out.
Asystolic patients (as opposed to those with a "shockable rhythm" such as ventricular fibrillation or ventricular tachycardia, which can be potentially treated with defibrillation) usually present with a very poor prognosis: asystole is found initially in only about 28% of cardiac arrest cases,[3] but only 15% of these patients ever leave the hospital alive, even with the benefit of an intensive care unit, with the rate being lower (only 6%) for those already prescribed drugs for high blood pressure.[4]
Asystole is treated by cardiopulmonary resuscitation (CPR) combined with an intravenous vasopressor such as epinephrine (a.k.a. adrenaline). Sometimes an underlying reversible cause can be detected and treated (the so-called 'Hs and Ts', an example of which is hypokalaemia). Several interventions previously recommended—such as defibrillation (known to be ineffective on asystole, but previously performed in case the rhythm was actually very fine ventricular fibrillation) and intravenous atropine—are no longer part of the routine protocols recommended by most major international bodies.[5] Asystole may be treated with 1 mg epinephrine by IV every 3–5 minutes as needed. Vasopressin is no longer part of ACLS protocol for PEA as of AHA 2015 guidelines due to lack of evidence of benefit vs. Epinephrine only every 3-5 minutes.
Survival rates in a cardiac arrest patient with asystole are much lower than a patient with a rhythm amenable to defibrillation; asystole is itself not a "shockable" rhythm. Out-of-hospital survival rates (even with emergency intervention) are less than 2 percent.[6]
Cause
Possible underlying causes, which may be treatable and reversible in certain cases, include the Hs and Ts.[7][8][9]
- Hypovolemia
- Hypoxia
- Hydrogen ions (acidosis)
- Hypothermia
- Hyperkalemia or Hypokalemia
- Hypoglycemia
- Tablets or Toxins (drug overdose)
- Electric shock
- Tachycardia
- Cardiac Tamponade
- Tension pneumothorax
- Thrombosis (myocardial infarction or pulmonary embolism)
- Trauma (hypovolemia from blood loss)
While the heart is asystolic, there is no blood flow to the brain unless CPR or internal cardiac massage (when the chest is opened and the heart is manually compressed) is performed, and even then it is a small amount. After many emergency treatments have been applied but the heart is still unresponsive, it is time to consider pronouncing the patient dead. Even in the rare case that a rhythm reappears, if asystole has persisted for fifteen minutes or more, the brain will have been deprived of oxygen long enough to cause brain death.
- ECG lead showing asystole (flatline)
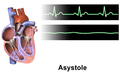 Asystole
Asystole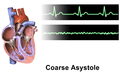 Asystole coarse
Asystole coarse
See also
References
- ↑ Harper, Douglas. "asystole". Online Etymology Dictionary.
- ↑ συστολή. Liddell, Henry George; Scott, Robert; A Greek–English Lexicon at the Perseus Project.
- ↑ Baldzizhar, A; Manuylova, E; Marchenko, R; Kryvalap, Y; Carey, MG (September 2016). "Ventricular Tachycardias: Characteristics and Management". Critical care nursing clinics of North America. 28 (3): 317–29. doi:10.1016/j.cnc.2016.04.004. PMID 27484660.
- ↑ Kutsogiannis, DJ (4 October 2011). "Survival after in-ICU PEA/asystole cardiac arrest unchanged at 20 yrs". CMAJ.
- ↑ AHA Cardiac Recussitation Guidelines, 2010: http://circ.ahajournals.org/cgi/content/full/122/18_suppl_3/S729
- ↑ "Medical Futility in Asystolic Out-of-Hospital Cardiac Arrest". Survey of Anesthesiology. 52 (5): 261. 1 October 2008. doi:10.1097/01.SA.0000318635.97636.a6. Retrieved 7 April 2018 – via journals.lww.com.
- ↑ Mazur G (2004). ACLS: Principles And Practice. Dallas: American Heart Assn. pp. 71–87. ISBN 0-87493-341-2.
- ↑ Barnes TG, Cummins RO, Field J, Hazinski MF (2003). ACLS for experienced providers. Dallas: American Heart Assn. pp. 3–5. ISBN 0-87493-424-9.
- ↑ ECC Committee, Subcommittees and Task Forces of the American Heart Association (Dec 2005). "2005 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care - Part 7.2: Management of Cardiac Arrest". Circulation. 112 (24 Suppl): IV1–203 (7.2 IV58–66). doi:10.1161/CIRCULATIONAHA.105.166550. PMID 16314375.