Short QT syndrome
| Short QT syndrome | |
|---|---|
 | |
| Schematic representation of normal ECG trace (sinus rhythm), with waves, segments, and intervals labeled. | |
| Specialty | Cardiology |
| Symptoms | Passing out, sudden cardiac death [1] |
| Causes | Genetic |
| Diagnostic method | Electrocardiogram (ECG) [1] |
| Treatment | Medication, implantable cardioverter defibrillator (ICD) [1] |
| Medication | Quinidine, Flecainide [1] |
| Prognosis | Risk of sudden cardiac death 0.8% per year [2] |
| Frequency | <300 cases reported worldwide [1] |
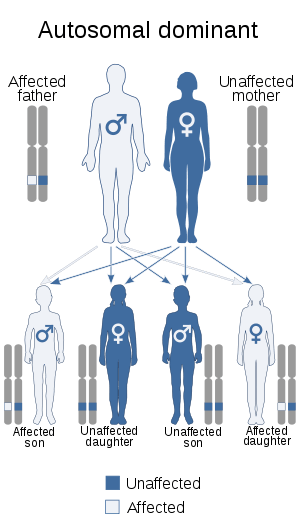
Short QT syndrome is a very rare genetic disease of the electrical system of the heart, and is associated with an increased risk of abnormal heart rhythms and sudden cardiac death. [1] The syndrome gets its name from a characteristic feature seen on an electrocardiogram (ECG). It is caused by mutations in genes encoding ion channels that shorten the cardiac action potential, and appears to be inherited in an autosomal dominant pattern. [1] The condition is diagnosed using a 12-lead ECG. [2] Short QT syndrome can be treated using an implantable cardioverter-defibrillator or medications including quinidine. [3] Short QT syndrome was first described in 2000 [4], and the first genetic mutation associated with the condition was identified in 2004. [5]
Signs and symptoms
Those affected by short QT syndrome have a tendency to develop abnormal heart rhythms.[3] These abnormal heart rhythms can take relatively benign forms such as atrial fibrillation, which may lead to symptoms of palpitations, breathlessness, or fatigue.[3] However, far more dangerous heart rhythm disturbances such as ventricular fibrillation can also occur in those with short QT syndrome, leading to blackouts or even sudden death.[3]
If someone with long QT syndrome is examined while their heart is beating in an abnormal rhythm such as atrial fibrillation, this can be detected by feeling their pulse. No abnormal signs will usually be found when examining someone with short QT syndrome while their heart is beating in a normal rhythm.
Cause
Short QT syndrome is a genetic disorder caused by mutations in genes responsible for producing certain ion channels within heart cells. It appears to be inherited in an autosomal dominant pattern.[1] Some mutations cause an increased flow of potassium out of the cell, while others reduce the flow of calcium into the cell.[1] The common effect of all these mutations is to shorten the cardiac action potential, reflected on the surface ECG as a shortening of the QT interval. A list of the genetic mutations associated with short QT syndrome can be found in the table below.
| Type | OMIM | Gene | Notes |
|---|---|---|---|
| SQT1 | 609620 | KCNH2 | Also known as hERG, encodes the potassium channel KV11.1 responsible for the delayed rectifier potassium current IKr [1] |
| SQT2 | 609621 | KCNQ1 | Encodes the potassium channel responsible for the delayed rectifier potassium current IKs [1] |
| SQT3 | 609622 | KCNJ2 | Encodes the potassium channel Kir2.1 responsible for the inward rectifying potassium current IK1 [1] |
| SQT4 | 114205 | CACNA1C | Encodes the alpha subunit of the L-type calcium channel carrying ICa(L) [1] |
| SQT5 | 114204 | CACNA2D1 | Encodes the alpha2/delta subunit of the L-type calcium channel carrying ICa(L) [1] |
| SQT6 | 106195 | SLC4A3 | Encodes a bicarbonate / chloride exchanger [1][6] |
Diagnosis
Short QT syndrome is diagnosed primarily using an electrocardiogram (ECG), but may also take into account the clinical history, family history, and possibly genetic testing. Whilst diagnostic scoring systems have been proposed that incorporate all of these factors,[7] they have not been universally accepted by international consensus guidelines, and there is uncertainty regarding the precise cutoffs to be used for diagnosis.[8]
12-lead ECG
.svg.png)
The mainstay of diagnosis of short QT syndrome is the 12-lead ECG. The precise QT duration used to diagnose the condition remains controversial with consensus guidelines giving cutoffs varying from 330 ms,[9] 340 ms or even 360 ms when other clinical, familial, or genetic factors are present.[8][9] The QT interval normally varies with heart rate, but this variation occurs to a lesser extent in those with short QT syndrome.[1] It is therefore recommended that the QT interval is assessed at heart rates close to 60 beats per minute.[1] Other features that may be seen on the ECG in short QT syndrome include tall, peaked T-waves and PR segment depression.[1]
Other features supporting diagnosis
Other features that support a diagnosis of short QT syndrome include: a history of ventricular fibrillation or ventricular tachycardia despite an apparently structurally normal heart; a family history of confirmed short QT syndrome; a family history of sudden cardiac death aged <40 years; and identification of a genetic mutation consistent with short QT syndrome.[8][9]
Invasive electrophysiological studies, in which wires are passed into the heart to stimulate and record the heart's electrical impulses, are not currently recommended for diagnosing short QT syndrome or predicting the risk of sudden cardiac death. [9][8]
Treatment
The treatment for short QT syndrome is aimed at preventing abnormal heart rhythms and reducing the risk of sudden cardiac death. It has been difficult to experimentally test potential treatments as the condition is very rare, so the evidence for treatment effectiveness comes largely from consensus opinion.[1] In addition to treating the person identified as having the condition, screening of family members may be recommended.
Implantable cardioverter-defibrillator
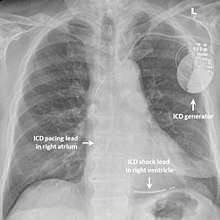
In those with short QT syndrome who have already experienced a life-threatening abnormal heart rhythm such as ventricular fibrillation, an implantable cardioverter-defibrillator (ICD) may be recommended to reduce the chance of sudden death.[3] This device is implanted under the skin and can continually monitor the heart rhythm. If the device detects a dangerous heart rhythm disturbance it can deliver a small electric shock with the aim of restoring a normal rhythm. Implanting an ICD in someone with short QT syndrome who has not yet experienced a life-threatening arrhythmia is more controversial but may be considered.[1][9]
Medication
Medication aimed at correcting the ECG abnormality - the shortened QT interval - has been tried. Quinidine, a class Ia antiarrhythmic agent, has been shown to partially correct the QT interval and make the heart more resilient to artificially-induced abnormal heart rhythms,[3][10] although it is still uncertain at present whether this translates to a lower risk of sudden death.[1][11] Sotalol, another antiarrhythmic, may prolong the QT ins some subtypes of short QT syndrome.[12] Other medications including beta blockers, flecainide, and amiodarone have been tried, but at present there is little evidence to support their use in reducing the risk of sudden death in those with short QT syndrome.[1]
Drugs can also be used to treat the less dangerous abnormal heart rhythm that is also associated with short QT - atrial fibrillation. Propafenone, a class 1c antiarrhythmic, may be helpful in those with short QT to prevent atrial fibrillation.[13] Those who develop atrial fibrillation may also require medication to decrease blood clotting in order to reduce the risk of stroke.[14]
Epidemiology
Short QT syndrome is a very rare condition with, as of 2018, fewer than 300 cases described in the medical literature.[1] As a genetic syndrome, those affected are born with the condition. Symptoms can occur in childhood, potentially presenting as sudden infant death syndrome (also known as cot death), although they may not occur until adulthood. [2] Males and females are equally likely to be affected, and have a similar risk of sudden cardiac death. [2] The risk of sudden cardiac death has been estimated at 0.8% per year, [2] leading to a cumulative risk of sudden cardiac death of 41% by the age of 40. [1]
History
The first report of short QT syndrome to be published was in 2000, describing a family with short QT intervals on the 12-lead ECG, atrial fibrillation occurring at a young age, and a unrelated patient who suffered sudden cardiac death associated with a short QT interval. [2] [4] In 2003, a family was described who had short QT intervals and a high risk of sudden cardiac death. [15] The first genetic mutation causing short QT syndrome was identified in 2004. [5] Criteria for diagnosing the condition were proposed in 2011. [7]
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 Bjerregaard P (August 2018). "Diagnosis and management of short QT syndrome". Heart Rhythm. 15 (8): 1261–1267. doi:10.1016/j.hrthm.2018.02.034. PMID 29501667.
- 1 2 3 4 5 6 Bjerregaard, Preben; Gussak, Ihor (2013), "Short QT Syndrome", Electrical Diseases of the Heart, Springer London, pp. 569–581, doi:10.1007/978-1-4471-4881-4_33, ISBN 9781447148807
- 1 2 3 4 5 6 Schimpf R, Wolpert C, Gaita F, Giustetto C, Borggrefe M (August 2005). "Short QT syndrome". Cardiovascular Research. 67 (3): 357–66. doi:10.1016/j.cardiores.2005.03.026. PMID 15890322.
- 1 2 Gussak, I.; Brugada, P.; Brugada, J.; Wright, R. S.; Kopecky, S. L.; Chaitman, B. R.; Bjerregaard, P. (2000). "Idiopathic short QT interval: a new clinical syndrome?". Cardiology. 94 (2): 99–102. doi:10.1159/000047299. ISSN 0008-6312. PMID 11173780.
- 1 2 Brugada, Ramon; Hong, Kui; Dumaine, Robert; Cordeiro, Jonathan; Gaita, Fiorenzo; Borggrefe, Martin; Menendez, Teresa M.; Brugada, Josep; Pollevick, Guido D. (2004-01-06). "Sudden death associated with short-QT syndrome linked to mutations in HERG". Circulation. 109 (1): 30–35. doi:10.1161/01.CIR.0000109482.92774.3A. ISSN 1524-4539. PMID 14676148.
- ↑ Thorsen K, Dam VS, Kjaer-Sorensen K, Pedersen LN, Skeberdis VA, Jurevičius J, et al. (November 2017). "Loss-of-activity-mutation in the cardiac chloride-bicarbonate exchanger AE3 causes short QT syndrome". Nature Communications. 8 (1): 1696. doi:10.1038/s41467-017-01630-0. PMC 5700076. PMID 29167417.
- 1 2 Gollob MH, Redpath CJ, Roberts JD (February 2011). "The short QT syndrome: proposed diagnostic criteria". Journal of the American College of Cardiology. 57 (7): 802–12. doi:10.1016/j.jacc.2010.09.048. PMID 21310316.
- 1 2 3 4 Priori SG, Blomström-Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, et al. (November 2015). "2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC)Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC)". Europace. 17 (11): 1601–87. doi:10.1093/europace/euv319. PMID 26318695.
- 1 2 3 4 5 Priori SG, Wilde AA, Horie M, Cho Y, Behr ER, Berul C, et al. (December 2013). "HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013". Heart Rhythm. 10 (12): 1932–63. doi:10.1016/j.hrthm.2013.05.014. PMID 24011539.
- ↑ Gaita F, Giustetto C, Bianchi F, Schimpf R, Haissaguerre M, Calò L, et al. (April 2004). "Short QT syndrome: pharmacological treatment". Journal of the American College of Cardiology. 43 (8): 1494–9. doi:10.1016/j.jacc.2004.02.034. PMID 15093889.
- ↑ Maltret A, Wiener-Vacher S, Denis C, Extramiana F, Morisseau-Durand MP, Fressart V, et al. (February 2014). "Type 2 short QT syndrome and vestibular dysfunction: mirror of the Jervell and Lange-Nielsen syndrome?". International Journal of Cardiology. 171 (2): 291–3. doi:10.1016/j.ijcard.2013.11.078. PMID 24380499.
- ↑ Priori SG, Wilde AA, Horie M, Cho Y, Behr ER, Berul C, et al. (December 2013). "HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013". Heart Rhythm. 10 (12): 1932–63. doi:10.1016/j.hrthm.2013.05.014. PMID 24011539.
- ↑ Enriquez A, Antzelevitch C, Bismah V, Baranchuk A (September 2016). "Atrial fibrillation in inherited cardiac channelopathies: From mechanisms to management". Heart Rhythm. 13 (9): 1878–84. doi:10.1016/j.hrthm.2016.06.008. PMID 27291509.
- ↑ January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC, et al. (December 2014). "2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society". Journal of the American College of Cardiology. 64 (21): e1–76. doi:10.1016/j.jacc.2014.03.022. PMID 24685669.
- ↑ Gaita, Fiorenzo; Giustetto, Carla; Bianchi, Francesca; Wolpert, Christian; Schimpf, Rainer; Riccardi, Riccardo; Grossi, Stefano; Richiardi, Elena; Borggrefe, Martin (2003-08-26). "Short QT Syndrome: a familial cause of sudden death". Circulation. 108 (8): 965–970. doi:10.1161/01.CIR.0000085071.28695.C4. ISSN 1524-4539. PMID 12925462.
External links
- "Short QT syndrome". Genetics Home Reference. U.S. National Library of Medicine.
| Classification |
|---|