''Acanthamoeba'' keratitis
| Acanthamoeba keratitis | |
|---|---|
 | |
|
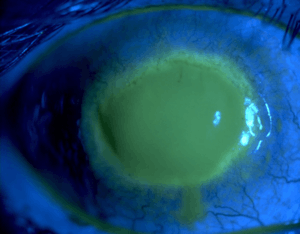
Eye with Acanthamoeba keratitis (fluorescein observation) | |
| Specialty |
Ophthalmology, Infectious disease |
Acanthamoeba keratitis is a rare disease in which amoebae invade the cornea of the eye. It may result in permanent visual impairment or blindness.[1][2]
Causes
In the United States, it is nearly always associated with contact lens use, as Acanthamoeba can survive in the space between the lens and the eye.[3][4][5][6] To prevent the condition, contact lenses must be properly disinfected before wearing, and should be removed when swimming or surfing.
However, there have been many cases of Acanthamoeba in those who do not wear contact lenses, elsewhere in the world.[7][8]
Life cycle
Species within the genus, Acanthamoeba, are generally free-living trophozoites. These trophozoites are relatively ubiquitous and can live in, but are not restricted to, tap water, freshwater lakes,rivers and soil.[9] Besides the trophozoite stage, a cyst stage may also be present. Both of these stages are usually unnucleated and reproduce by the means of binary fission. In unfavorable conditions, the trophozoites encyst to produce double-walled cysts.[10]

Diagnosis
To detect Acanthamoeba on a contact lens in a laboratory, the contact lens is placed on a non-nutrient agar saline plate seeded with a gram-negative bacteria such as E. coli. If Acanthamoeba are present, they will reproduce readily and become visible on the plate under 10-20X objective on an inverted microscope. Polymerase chain reaction can also be used to confirm a diagnosis of Acanthamoeba keratitis, especially when contact lenses are not involved. Acanthameoba is also characterized by a brawny edema and hazy view into the anterior chamber. Late stages of the disease also produces a ring shaped corneal ulcer.[11] Signs and symptoms include severe pain, severe keratitis (similar to stromal herpetic disease), corneal perineuritis, and ring ulcer (late in the disease process).[10]
Prevention
According to the American Optometric Association, the following steps can be taken to prevent Acanthamoeba keratitis:
Always wash and dry your hands before handling contact lenses, ordinary water should never come in contact with your lenses. Rub and rinse the surface of the contact lens before storing. Use only sterile products recommended by your optometrist to clean and disinfect your lenses. Saline solution and rewetting drops are not designed to disinfect lenses. Avoid using tap water to wash or store contact lenses. Contact lens solution must be discarded upon opening the case, and fresh solution used each time the lens is placed in the case. Replace lenses using your doctor’s prescribed schedule. Do not sleep in contact lenses unless prescribed by your doctor and never after swimming. Never swap lenses with someone else. Never put contact lenses in your mouth. See your optometrist regularly for contact lens evaluation.[12]
Treatment
One treatment used is polyhexamethylene biguanide, PHMB.[13]
Propamidine isethionate has also shown some effectiveness.[14]
Another possible agent is chlorhexidine.[15]
Keratoplasty may sometimes be required.[14]
A combined regimen of propamidine, miconazole nitrate, and neomycin has also been suggested.[16][17]
A recent Cochrane review found one study[18] that compared the effectiveness of chlorhexidine eye drops against PHMB eye drops, for eyes with Acanthamoeba keratitis. The differences between treatments were not statistically significant; the review found that 86% of eyes treated with chlorhexidine eye drops reported a resolution of infection, compared to 78% of eyes treated with PHMB eye drops.[19] The study also found that 71% of eyes treated with chlorhexidine eye drops reported improved visual acuity after treatment, compared to 57% of eyes in the PMGB group; these results were also not significant.[19]
Epidemiology
A study in Austria found over the course of the testing, a total of 154 cases of Acanthamoeba keratitis. The age of the positive tests ranged from 8 to 82 years old and 58% of the people were female. The data showed that 89% of the infected patients were contact lens wearers and 19% required a corneal transplant.[20]
References
- ↑ Lorenzo-Morales, Jacob; Khan, Naveed A.; Walochnik, Julia (2015). "An update on Acanthamoeba keratitis: diagnosis, pathogenesis and treatment". Parasite. 22: 10. doi:10.1051/parasite/2015010. ISSN 1776-1042. PMC 4330640. PMID 25687209.

- ↑ "CDC - Acanthamoeba Infection - General Information - Acanthamoeba Keratitis FAQs". Cdc.gov. Retrieved 2013-08-02.
- ↑ Auran, JD; Starr MB; Jakobiec FA (1987). "Acanthamoeba keratitis. A review of the literature". Cornea. 6 (1): 2–26. doi:10.1097/00003226-198706010-00002. PMID 3556011.
- ↑ JOHN D.T. (1993) Opportunistically pathogenic free-living amebae. In: J.P. Kreier and J.R. Baker (Eds.), Parasitic Protozoa. Vol. 3. Academic Press, New York, pp. 143–246.
- ↑ Badenoch, PR; Adams M; Coster DJ (February 1995). "Corneal virulence, cytopathic effect on human keratocytes and genetic characterization of Acanthamoeba". International Journal for Parasitology. 25 (2): 229–39. doi:10.1016/0020-7519(94)00075-Y. PMID 7622330.
- ↑ Niederkorn, JY; Alizadeh H; Leher H; McCulley JP (May 1999). "The pathogenesis of Acanthamoeba keratitis". Microbes and Infection. 1 (6): 437–43. doi:10.1016/S1286-4579(99)80047-1. PMID 10602676.
- ↑ Sharma, S; Garg, P; Rao, GN (2000). "Patient characteristics, diagnosis, and treatment of non-contact lens related Acanthamoeba keratitis". The British Journal of Ophthalmology. 84 (10): 1103–8. doi:10.1136/bjo.84.10.1103. PMC 1723254. PMID 11004092.
- ↑ Bharathi JM, Srinivasan M, Ramakrishnan R, Meenakshi R, Padmavathy S, Lalitha PN (2007). "A study of the spectrum of Acanthamoeba keratitis: a three-year study at a tertiary eye care referral center in South India". Indian J Ophthalmol. 55 (1): 37–42. doi:10.4103/0301-4738.29493. PMID 17189885.
- ↑ "Acanthamoeba-General Information-Acanthamoeba keratitis". CDC.
- 1 2 "Free-living Amebic Infections". CDC.
- ↑ Pasricha, Gunisha; Savitri Sharma; Prashant Garg; Ramesh K. Aggarwal (July 2003). "Use of 18S rRNA Gene-Based PCR Assay for Diagnosis of Acanthamoeba Keratitis in Non-Contact Lens Wearers in India". Journal of Clinical Microbiology. 41 (7): 3206–3211. doi:10.1128/JCM.41.7.3206-3211.2003. PMC 165372. PMID 12843065.
- ↑ "Acanthamoeba". AOA.
- ↑ Sharma S, Garg P, Rao GN (October 2000). "Patient characteristics, diagnosis, and treatment of non-contact lens related Acanthamoeba keratitis". Br J Ophthalmol. 84 (10): 1103–8. doi:10.1136/bjo.84.10.1103. PMC 1723254. PMID 11004092.
- 1 2 Lindsay RG, Watters G, Johnson R, Ormonde SE, Snibson GR (September 2007). "Acanthamoeba keratitis and contact lens wear". Clin Exp Optom. 90 (5): 351–60. doi:10.1111/j.1444-0938.2007.00172.x. PMID 17697181.
- ↑ Hammersmith KM (August 2006). "Diagnosis and management of Acanthamoeba keratitis". Current Opinion in Ophthalmology. 17 (4): 327–31. doi:10.1097/01.icu.0000233949.56229.7d. PMID 16900022.
- ↑ "Acanthamoeba: Treatment & Medication - eMedicine Infectious Diseases". Retrieved 2009-02-27.
- ↑ S. Singh; M. P. Sachdeva (July 23, 1994). "Acanthamoeba keratitis". BMJ. 309 (6949): 273. doi:10.1136/bmj.309.6949.273. PMC 2540756. PMID 7802782.
- ↑ Lim N, Goh D, Bunce C, Xing W, Fraenkel G, Poole TR, Ficker L (2008). "Comparison of polyhexamethylene biguanide and chlorhexidine as monotherapy agents in the treatment of Acanthamoeba keratitis". Am J Ophthalmol. 145 (1): 130–135. doi:10.1016/j.ajo.2007.08.040. PMID 17996208.
- 1 2 Alkharashi M, Lindsley K, Law HA, Sikder S (2015). "Medical interventions for acanthamoeba keratitis". Cochrane Database Syst Rev. 2: CD0010792. doi:10.1002/14651858.CD010792.pub2. PMC 4730543. PMID 25710134.
- ↑ Walochnik, J; Sheikl, U; Haller-Schober, EM (2014). "Twenty Years of Acanthamoeba Diagnostics in Austria". The Journal of Eukaryotic Microbiology. 62 (1): 3–11. doi:10.1111/jeu.12149. PMC 4342769.
External links
| Classification | |
|---|---|
| External resources |