Metabolic acidosis
| Metabolic acidosis | |
|---|---|
 | |
| Davenport diagram | |
| Classification and external resources | |
| Specialty | Endocrinology |
| Patient UK | Metabolic acidosis |
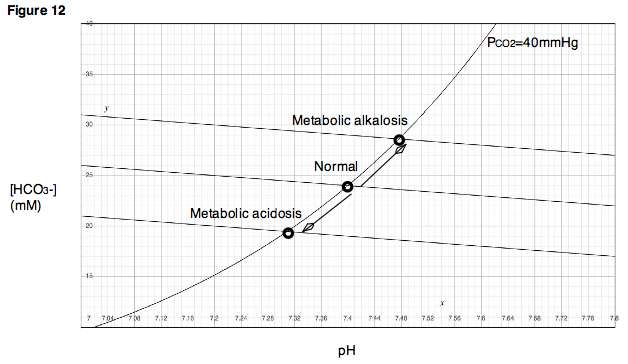
Metabolic acidosis is a condition that occurs when the body produces excessive quantities of acid or when the kidneys are not removing enough acid from the body. If unchecked, metabolic acidosis leads to acidemia, i.e., blood pH is low (less than 7.35) due to increased production of hydrogen ions by the body or the inability of the body to form bicarbonate (HCO3−) in the kidney. Its causes are diverse, and its consequences can be serious, including coma and death. Together with respiratory acidosis, it is one of the two general causes of acidemia.
Terminology :
- Acidosis refers to a process that causes a low pH in blood and tissues.
- Acidemia refers specifically to a low pH in the blood.
In most cases, acidosis occurs first for reasons explained below. Free hydrogen ions then diffuse into the blood, lowering the pH. Arterial blood gas analysis detects acidemia (pH lower than 7.35). When acidemia is present, acidosis is presumed.
Signs and symptoms
Symptoms are not specific, and diagnosis can be difficult unless the patient presents with clear indications for arterial blood gas sampling. Symptoms may include chest pain, palpitations, headache, altered mental status such as severe anxiety due to hypoxia, decreased visual acuity, nausea, vomiting, abdominal pain, altered appetite and weight gain, muscle weakness, bone pain, and joint pain. Those in metabolic acidosis may exhibit deep, rapid breathing called Kussmaul respirations which is classically associated with diabetic ketoacidosis. Rapid deep breaths increase the amount of carbon dioxide exhaled, thus lowering the serum carbon dioxide levels, resulting in some degree of compensation. Overcompensation via respiratory alkalosis to form an alkalemia does not occur.
Extreme acidemia leads to neurological and cardiac complications:
- Neurological: lethargy, stupor, coma, seizures
- Cardiac: Abnormal heart rhythms (e.g., ventricular tachycardia) and decreased response to epinephrine, both leading to low blood pressure
Physical examination occasionally reveals signs of disease, but is otherwise normal. Cranial nerve abnormalities are reported in ethylene glycol poisoning, and retinal edema can be a sign of methanol intoxication. Longstanding chronic metabolic acidosis leads to osteoporosis and can cause fractures.
Causes
Metabolic acidosis occurs when the body produces too much acid, or when the kidneys are not removing enough acid from the body. Several types of metabolic acidosis occur. The main causes are best grouped by their influence on the anion gap.
The anion gap can be spuriously normal in sampling errors of the sodium level, e.g. in extreme hypertriglyceridemia. The anion gap can be increased due to relatively low levels of cations other than sodium and potassium (e.g. calcium or magnesium).
Increased anion gap
Causes of increased anion gap include:
- Lactic acidosis
- Ketoacidosis
- Chronic kidney failure (accumulation of sulfates, phosphates, urea)
- Transient 5-oxoprolinemia due to long-term ingestion of high-doses of acetaminophen (often seen with sepsis, liver failure, kidney failure, or malnutrition)
- Intoxication:
- Propylene glycol (metabolized to L and D-lactate and is often found in infusions for certain intravenous medications used in the intensive care unit)
- Massive rhabdomyolysis
A mnemonic can also be used - MUDPILES[1]
- M-Methanol
- U-Uremia (chronic kidney failure)
- D-Diabetic ketoacidosis
- P-Paraldehyde (rare)
- I-Infection, Iron, Isoniazid, Inborn errors of metabolism
- L-Lactic acidosis (L-lactate and D-lactate)
- E-Ethylene glycol (Note: Ethanol is sometimes included in this mnemonic, as well, although the acidosis caused by ethanol is actually primarily due to the increased production of lactic acid found in such intoxication.)
- S-Salicylates
Pathophysiology
Compensatory mechanisms
Metabolic acidosis is either due to increased generation of acid or an inability to generate sufficient bicarbonate. The body regulates the acidity of the blood by four buffering mechanisms.
- Bicarbonate buffering system
- Intracellular buffering by absorption of hydrogen atoms by various molecules, including proteins, phosphates and carbonate in bone.
- Respiratory compensation. Hyperventilation will cause more carbon dioxide to be removed from the body and thereby increase pH.
- Kidney compensation
Buffer
The decreased bicarbonate that distinguishes metabolic acidosis is therefore due to two separate processes: the buffer (from water and carbon dioxide) and additional renal generation. The buffer reactions are:
The Henderson-Hasselbalch equation mathematically describes the relationship between blood pH and the components of the bicarbonate buffering system:
- Using Henry's Law, we can say that [CO2]=0.03xPaCO2
- (PaCO2 is the pressure of CO2 in arterial blood)
- Adding the other normal values, we get
Diagnosis
Although blood gas sampling is not always essential for the diagnosis of acidosis, a low pH (in either a venous or arterial sample) does support the diagnosis. If the pH is low (under 7.35) and the bicarbonate levels are decreased (<24 mmol/L), metabolic acidemia is present, and metabolic acidosis is presumed. If the patient has other coexisting acid-base disorders, the pH may be low, normal or high in the setting of metabolic acidosis. If a setting of a cause for metabolic acidosis being noted in the patient's history, a low serum bicarbonate indicates metabolic acidosis even without measurement of serum pH.
Other tests relevant in this context are electrolytes (including chloride), glucose, kidney function, and a full blood count. Urinalysis can reveal acidity (salicylate poisoning) or alkalinity (renal tubular acidosis type I). In addition, it can show ketones in ketoacidosis.
To distinguish between the main types of metabolic acidosis, a clinical tool called the anion gap is considered very useful. It is calculated by subtracting the sum of the chloride and bicarbonate levels from the sum of the sodium and potassium levels. As sodium is the main extracellular cation, and chloride and bicarbonate are the main anions, the result should reflect the remaining anions. Normally, this concentration is about 8-16 mmol/L (12±4). An elevated anion gap (i.e. > 16 mmol/L) can indicate particular types of metabolic acidosis, particularly certain poisons, lactate acidosis, and ketoacidosis.
As the differential diagnosis is made, certain other tests may be necessary, including toxicological screening and imaging of the kidneys. It is also important to differentiate between acidosis-induced hyperventilation and asthma; otherwise, treatment could lead to inappropriate bronchodilation.[2]
Treatment
A pH under 7.1 is an emergency, due to the risk of abnormal heart rhythms, and may warrant treatment with intravenous bicarbonate. Bicarbonate is given at 50-100 mmol at a time under scrupulous monitoring of the arterial blood gas readings. This intervention, however, has some serious complications in lactic acidosis, and in those cases, should be used with great care.
If the acidosis is particularly severe and/or intoxication may be present, consultation with the nephrology team is considered useful, as dialysis may clear both the intoxication and the acidosis.
See also
References
- ↑ "Anion Gap: Acid Base Tutorial". University of Connecticut Health Center. Archived from the original on 2008-11-21. Retrieved 2015-02-25.
- ↑ Meert, K. L; Clark, J; Sarnaik, A. P (2007). "Metabolic acidosis as an underlying mechanism of respiratory distress in children with severe acute asthma". Pediatric Critical Care Medicine. 8 (6): 519–23. doi:10.1097/01.PCC.0000288673.82916.9D. PMID 17906597.
External links
| Classification | |
|---|---|
| External resources |