Fosinopril
 | |
| Clinical data | |
|---|---|
| Trade names | Monopril |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a692020 |
| Pregnancy category | |
| Routes of administration | oral |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | ~36% |
| Protein binding | 87% (fosinoprilat) |
| Metabolism | hepatic, GIT mucosa (to fosinoprilat) |
| Elimination half-life | 12 hours (fosinoprilat) |
| Excretion | renal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| Chemical and physical data | |
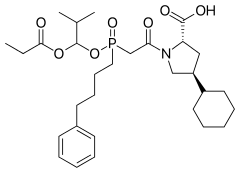
| Formula | C30H46NO7P |
| Molar mass | 563.663 g/mol |
| 3D model (JSmol) | |
| |
| |
| | |
Fosinopril is an angiotensin converting enzyme (ACE) inhibitor[1] used for the treatment of hypertension and some types of chronic heart failure. Fosinopril is the only phosphinate-containing ACE inhibitor marketed, by Bristol-Myers Squibb under the trade name Monopril.

Fosinoprilat and fosinopril
Fosinoprilat proved to have the same problem as enalaprilat and the other carboxylate-containing ACE inhibitors (namely poor oral bioavailability). Addition of a hydrophobic side-chain modulated the ionisation characteristics of the molecule, making it more bioavailable. Fosinopril is administered as a prodrug and is converted in vivo to the active form fosinoprilat.
Congestive heart failure and angiotensin II
In congestive heart failure, the ability of the heart to pump enough blood to satisfy the physiological needs of the body is reduced.[2] This condition has a variety of causes, including damaged heart valves, myocardial infarction, hypertension, vitamin B1 deficiency, and genetic mutations. When subsequent blood flow to the kidneys is reduced, the kidneys respond by increasing the secretion of renin from the juxtaglomerular apparatus. Renin converts the inactive angiotensinogen into angiotensin I, which is converted to angiotensin II (AII) by angiotensin converting enzyme (ACE). AII can have negative effects on the cardiovascular system after events such as heart failure and myocardial infarction. AII causes arterial vasoconstriction and hypertension, resulting in an increase in afterload, increasing the resistance against which the heart works.[3] Additionally, chronic increase in production of AII is associated with structural changes to the myocardium[4] which reduces the functionality of the heart.[3]
Effects of fosinopril on treating heart failure
Fosinopril is de-esterified by the liver or gastrointestinal mucosa and is converted to its active form, fosinoprilat.[5] Fosinoprilat competitively binds to ACE, preventing ACE from binding to and converting angiotensin I to angiotensin II. Inhibiting the production of AII lowers peripheral vascular resistance, decreases afterload, and decreases blood pressure,[3] thus helping to alleviate the negative effects of AII on cardiac performance. In heart failure patients, fosinopril increases exercise tolerance and lowers the frequency of events associated with worsening heart failure, such as dyspnea, the need for supplemental diuretics, fatigue, and hospitalizations.[6] In a study examining the effects of fosinopril on insulin-like growth factor 1 (IGF-1) and IGF binding protein serum concentrations in high cardiovascular risk patients, a six-month treatment of fosinopril was associated with an elevation in IGF-1.[7] Since a decline in IGF-1 is associated with an increased risk of ischemic heart disease, fosinopril may reduce ischemic risk.
Benefits
Unlike other ACE inhibitors that are primarily excreted by the kidneys, fosinopril is eliminated from the body by both renal and hepatic pathways.[8] This characteristic of fosinopril makes the drug a safer choice than other ACE inhibitors for heart failure patients with impaired kidney function resulting from poor perfusion[9] as fosinopril can still be eliminated by the liver, preventing accumulation of the drug in the body.[8]
References
- ↑ Pilote L, Abrahamowicz M, Eisenberg M, Humphries K, Behlouli H, Tu JV (May 2008). "Effect of different angiotensin-converting-enzyme inhibitors on mortality among elderly patients with congestive heart failure". CMAJ. 178 (10): 1303–11. doi:10.1503/cmaj.060068. PMC 2335176. PMID 18458262.
- ↑ Guyton, Arthur C., Hall, John E. (2006). Textbook of Medical Physiology (11th ed.). Philadelphia: Elsevier Saunders. ISBN 0-7216-0240-1
- 1 2 3 Katzung, Bertram G.; Masters, Susan B.; Trevor, Anthony J. (2009). Basic and Clinical Pharmacology. 11th ed. New York: McGraw-Hill. ISBN 978-0-07-160405-5
- ↑ Yamagishi H., Kim S., Nishikimi T., Takeuchi K., Takeda T. (1993). Contribution of cardiac renin-angiotensin system to ventricular remodelling in myocardial-infarcted rats. Journal of Molecular and Cellular Cardiology, 25(11):1369-80.
- ↑ Duchin K.L., Waclawski A.P., Tu J.I., Manning J., Frantz M., Willard D.A. (1991). Pharmacokinetics, Safety, and Pharmacologic Effects of Fosinopril Sodium, an Angiotensin-Converting Enzyme Inhibitor in Healthy Subjects. Journal of Clinical Pharmacology, 31(1):58-64.
- ↑ Erhardt L., MacLean A., Ilgenfritz J., Gelperin K., Blumenthal M. (1995). Fosinopril attenuates clinical deterioration and improves exercise tolerance in patients with heart failure. Fosinopril Efficacy/Safety Trial (FEST) Study Group. European Heart Journal,16(12):1892-9.
- ↑ Giovannini S., Cesari M., Marzetti E., Leeuwenburgh C., Maggio M., Pahor M. (2010). Effects of ACE-inhibition on IGF-1 and IGFBP-3 concentrations in older adults with high cardiovascular risk profile. Journal of Nutrition Health and Aging,14(6):457-60.
- 1 2 Zannad F., Chati Z., Guest M., Plat F. (1998). Differential effects of fosinopril and enalapril in patients with mild to moderate chronic heart failure. Fosinopril in Heart Failure Study Investigators. American Heart Journal, 136(4 Pt 1):672-80.
- ↑ Greenbaum R., Zucchelli P., Caspi A., Nouriel H., Paz R., Sclarovsky S., O'Grady P., Yee K.F., Liao W.C., Mangold B. (2000). Comparison of the pharmacokinetics of fosinoprilat with enalaprilat and lisinopril in patients with congestive heart failure and chronic renal insufficiency. British Journal of Clinical Pharmacology, 49(1):23-31.