Biotin
Biotin also called vitamin H (the H represents Haar und Haut, German words for "hair and skin"), vitamin B7 or vitamin B8 (in many countries like France, where vitamin B7 is used for Inositol) is a water-soluble B vitamin.[2][3] It is involved in a wide range of metabolic processes, both in humans and in other organisms, primarily related to the utilization of fats, carbohydrates, and amino acids.
 | |
 | |
| Names | |
|---|---|
| IUPAC name
5-[(3aS,4S,6aR)-2-oxohexahydro-1H-thieno[3,4-d]imidazol-4-yl]pentanoic acid | |
| Other names
Vitamin B7; Vitamin H; Coenzyme R; Biopeiderm | |
| Identifiers | |
3D model (JSmol) |
|
| ChEBI | |
| ChEMBL | |
| ChemSpider | |
| DrugBank | |
| ECHA InfoCard | 100.000.363 |
IUPHAR/BPS |
|
| KEGG | |
PubChem CID |
|
| UNII | |
CompTox Dashboard (EPA) |
|
InChI
| |
| |
| Properties | |
| C10H16N2O3S | |
| Molar mass | 244.31 g·mol−1 |
| Appearance | White crystalline needles |
| Melting point | 232 to 233 °C (450 to 451 °F; 505 to 506 K) |
| 22 mg/100 mL | |
| Pharmacology | |
| A11HA05 (WHO) | |
| Hazards | |
| NFPA 704 (fire diamond) | 
1
1
0 |
Except where otherwise noted, data are given for materials in their standard state (at 25 °C [77 °F], 100 kPa). | |
| Infobox references | |
Biotin deficiency can be caused by inadequate dietary intake or inheritance of one or more inborn genetic disorders that affect biotin metabolism.[2][3] Subclinical deficiency can cause mild symptoms, such as hair thinning, brittle fingernails, or skin rash, typically on the face.[2] Neonatal screening for biotinidase deficiency started in the United States in 1984, with many countries testing for this disorder at birth. Individuals born prior to 1984 are unlikely to have been screened, obscuring the true prevalence of the disorder.[2]
Overview
Biotin is an important component of enzymes involved in metabolizing fats and carbohydrates, influencing cell growth, and affecting amino acids involved in protein synthesis.[2][3] Biotin assists in various metabolic reactions involving the transfer of carbon dioxide. It may also be helpful in maintaining a steady blood sugar level. Biotin is often recommended as a dietary supplement for strengthening hair and nails, though scientific data supporting these outcomes are weak.[3] Nevertheless, biotin is found in many cosmetics and health products for the hair and skin.[4][5]
Biotin deficiency is rare.[2] The amounts needed are small, a wide range of foods contain biotin, and intestinal bacteria synthesize biotin, which is then absorbed by the host animal. For that reason, statutory agencies in various countries, for example, the USA[6] and Australia,[7] have not formally established a recommended daily intake of biotin. Instead, an adequate intake (AI) is identified based on the theory that average intake meets needs. Future research could result in biotin AIs with EARs and RDAs (see Dietary Reference Intake section).
A number of rare metabolic disorders exist in which an individual's metabolism of biotin is abnormal, such as deficiency in the holocarboxylase synthetase enzyme which covalently links biotin onto the carboxylase, where the biotin acts as a cofactor.[8]
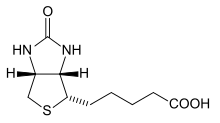
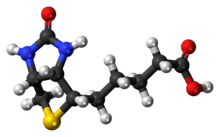
Biotin is composed of a ureido ring fused with a tetrahydrothiophene ring. The ureido ring acts as the carbon dioxide carrier in carboxylation reactions.[9] A valeric acid substituent is attached to one of the carbon atoms of the tetrahydrothiophene ring. Biotin is a coenzyme for multiple carboxylase enzymes, which are involved in the digestion of carbohydrates, synthesis of fatty acids, and gluconeogenesis.[3] Biotin is also required for the catabolism and utilization of the three branched-chain amino acids: leucine, isoleucine, and valine.
Biosynthesis
Biotin has an unusual structure (above figure), with two rings fused together via one of their sides. The two rings are ureido and tetrahydrothiophene moieties. Biotin is a heterocyclic, S-containing monocarboxylic acid. It is made from two precursors, alanine and pimeloyl-CoA via three enzymes. 8-Amino-7-oxopelargonic acid synthase is a pyridoxal 5'-phosphate enzyme. The pimeloyl-CoA could be produced by a modified fatty acid pathway involving a malonyl thioester as the starter. 7,8-Diaminopelargonic acid (DAPA) aminotransferase is unusual in using S-adenosyl methionine (SAM) as the NH2 donor. Dethiobiotin synthetase catalyzes the formation of the ureido ring via a DAPA carbamate activated with ATP. Biotin synthase reductively cleaves SAM into a deoxyadenosine radical, which abstracts an H atom from desthiobiotin to give an intermediate that is trapped by the sulfur donor. This sulfur donor is an iron-sulfur cluster.[10]
Cofactor biochemistry
D-(+)-Biotin is a cofactor responsible for carbon dioxide transfer in several carboxylase enzymes:
- Acetyl-CoA carboxylase alpha
- Acetyl-CoA carboxylase beta
- Methylcrotonyl-CoA carboxylase
- Propionyl-CoA carboxylase
- Pyruvate carboxylase
Biotin is important in fatty acid synthesis, branched-chain amino acid catabolism, and gluconeogenesis.[2][3] It covalently attaches to the epsilon-amino group of specific lysine residues in these carboxylases. This biotinylation reaction requires ATP and is catalyzed by holocarboxylase synthetase.[11] In bacteria, biotin is attached to biotin carboxyl carrier protein (BCCP) by biotin protein ligase (BirA in E. coli).[12] The attachment of biotin to various molecules, biotinylation, is used as an important laboratory technique to study various processes, including protein localization, protein interactions, DNA transcription, and replication. Biotinidase itself is known to be able to biotinylated histone proteins,[13] but little biotin is found naturally attached to chromatin.
Biotin binds tightly to the tetrameric protein avidin (also streptavidin and neutravidin), with a dissociation constant Kd on the order of 10−15 M, which is one of the strongest known protein-ligand interactions.[14] This is often used in different biotechnological applications. Until 2005, very harsh conditions were thought to be required to break the biotin-streptavidin interaction.[15]
Dietary recommendations
The U.S. Institute of Medicine (IOM) updated Estimated Average Requirements (EARs), Recommended Dietary Allowances (RDAs) and Tolerable Upper Intake Levels (ULs) for many vitamins in 1998. At that time there was insufficient information to establish EARs and RDAs for biotin. In instances such as this, the IOM sets Adequate Intakes (AIs) with the understanding that at some later date, when the physiological effects of biotin are better understood, AIs will be replaced by more exact information. Collectively EARs, RDAs, AIs and ULs are referred to as Dietary Reference Intakes (DRIs).[2][16]
The biotin AIs for both males and females (except for in pregnancy and lactation) are: 5 μg/day of biotin for 0-6-month-olds, 6 μg/day of biotin for 7-12-month-olds, 8 μg/day of biotin for 1-3-year-olds, 12 μg/day of biotin for 4-8-year-olds, 20 μg/day of biotin for 9-13-year-olds, 25 μg/day of biotin for 14-18-year-olds, and 30 μg/day of biotin for those 19-years old and older.
The biotin AIs for females who are either pregnant or lactating, respectively, are: 30 μg/day of biotin for pregnant females 14-50-years old; 35 μg/day of biotin for lactating females 14-50-years old.[2][3][16]
The European Food Safety Authority (EFSA) refers to the collective set of information as Dietary Reference Values, with Population Reference Intake instead of RDA, and Average Requirement instead of EAR. AI and UL are defined the same as in the United States. For women and men over age 18, the Adequate Intake is set at 40 μg/day. The AI for pregnancy is 40 μg/day per day, and 45 μg/day during breastfeeding. For children ages 1–17 years, the AIs increase with age from 20 to 35 μg/day.[17]
For the United States food and dietary supplement labeling purposes, the amount in a serving is expressed as a percent of Daily Value (DV). For biotin labeling purposes, 100% of the Daily Value was revised in 2016 to 30 μg/day to bring it into an agreement with the AI.[18] The deadline to be in compliance was set on January 1, 2020, for large companies and January 1, 2021, for small companies.[19]
Safety
The U.S. Institute of Medicine estimates upper limits (ULs) for vitamins and minerals when evidence for a true limit is sufficient. For biotin, however, there is no UL because adverse effects of high biotin intake have not been determined.[16] EFSA also reviewed safety and reached the same conclusion as in the United States that there is insufficient evidence to set a UL for biotin.[20]
Sources
Biotin is synthesized by intestinal bacteria, but there is a lack of good quality studies about how much biotin they provide.[3]
Biotin is stable at room temperature and is not destroyed by cooking. Sources with appreciable content are:[2][3][21]
| Food | µg per serving |
Serving size | µg per 100 g |
|---|---|---|---|
| Chicken liver, cooked | 138 | 74g | 186.5 |
| Beef or pork liver, cooked | up to 35 | 3 ounce | |
| Egg, cooked | up to 25 | large egg | |
| Yeast, baker's, dried | up to 14 | 7 gram packet | up to 200 |
| Avocado | up to 6 | avocado | |
| Peanuts, roasted, salted | can vary between 5 μg and 28 μg |
28g | 18-100 |
| Salmon, cooked | up to 5 | 3 ounce | |
| Sunflower seeds, roasted, salted | 2.4 | 31g | 7.7 |
Raw egg whites contain a protein (avidin) that blocks the absorption of biotin, so people who regularly consume a large number of raw eggs may become biotin-deficient.[16] The dietary biotin intake in Western populations has been estimated to be as high as 60 μg per day.[3] Biotin is also available in dietary supplements,[2] individually or as an ingredient in multivitamins.[3]
Bioavailability
Studies on biotin's bioavailability have been conducted in rats and in chicks. Based on these studies, biotin bioavailability may be low or variable, depending on the type of food being consumed. In general, biotin exists in food as protein-bound form or biocytin.[22] Proteolysis by protease is required prior to absorption. This process assists free biotin release from biocytin and protein-bound biotin. The biotin present in corn is readily available; however, most grains have about a 20-40% bioavailability of biotin.[23]
The wide variability in biotin bioavailability may be due to the ability of an organism to break various biotin-protein bonds from food. Whether an organism has an enzyme with that ability will determine the bioavailability of biotin from the foodstuff.[23]
Factors that affect biotin requirements
The frequency of marginal biotin status is not known, but the incidence of low circulating biotin levels in alcoholics has been found to be much greater than in the general population. Also, relatively low levels of biotin have been reported in the urine or plasma of patients who have had a partial gastrectomy or have other causes of achlorhydria, burn patients, epileptics, elderly individuals, and athletes.[23] Pregnancy and lactation may be associated with an increased demand for biotin. In pregnancy, this may be due to a possible acceleration of biotin catabolism, whereas, in lactation, the higher demand has yet to be elucidated. Recent studies have shown marginal biotin deficiency can be present in human gestation, as evidenced by increased urinary excretion of 3-hydroxyisovaleric acid, decreased urinary excretion of biotin and bisnorbiotin, and decreased plasma concentration of biotin. Additionally, smoking may further accelerate biotin catabolism in women.[24]
Deficiency
Biotin deficiency typically occurs from the absence of the vitamin in the diet, particularly in breastfeeding mothers.[2] Daily consumption of raw egg whites for several months may result in biotin deficiency,[25] due to their avidin content.
Deficiency can be addressed with nutritional supplementation.[25]
Deficiency symptoms include:[2]
- Brittle and thin fingernails
- Hair loss (alopecia)
- Conjunctivitis
- Dermatitis in the form of a scaly, red rash around the eyes, nose, mouth, and genital area.
- Neurological symptoms in adults, such as depression, lethargy, hallucination, and numbness and tingling of the extremities[25]
Symptoms like depression, hallucinations, tingling in the arms and legs, and lack of interest are indications that your biotin levels are low.[26] The neurological and psychological symptoms can occur with only mild deficiencies. Dermatitis, conjunctivitis, and hair loss will generally occur only when deficiency becomes more severe.[25] Individuals with hereditary disorders of biotin deficiency have evidence of impaired immune system function, including increased susceptibility to bacterial and fungal infections.[3] Pregnant women tend to have a higher risk of biotin deficiency. Nearly half of pregnant women have abnormal increases of 3-hydroxyisovaleric acid, which reflects the reduced status of biotin.[3]
Metabolic disorders
Inherited metabolic disorders characterized by deficient activities of biotin-dependent carboxylases are termed multiple carboxylase deficiency. These include deficiencies in the enzymes' holocarboxylase synthetase or biotinidase.[2] Holocarboxylase synthetase deficiency prevents the body's cells from using biotin effectively and thus interferes with multiple carboxylase reactions.[27] Biochemical and clinical manifestations include ketolactic acidosis, organic aciduria, hyperammonemia, skin rash, feeding problems, hypotonia, seizures, developmental delay, alopecia, and coma.
Biotinidase deficiency is not due to inadequate biotin, but rather to a deficiency in the enzymes that process it.[2] Biotinidase catalyzes the cleavage of biotin from biocytin and biotinyl-peptides (the proteolytic degradation products of each holocarboxylase) and thereby recycles biotin. It is also important in freeing biotin from dietary protein-bound biotin.[27] General symptoms include decreased appetite and growth. Dermatologic symptoms include dermatitis, alopecia, and achromotrichia (absence or loss of pigment in the hair). Perosis (a shortening and thickening of bones) is seen in the skeleton. Fatty liver and kidney syndrome and hepatic steatosis also can occur.[23]
History
In 1916, W.G. Bateman observed that a diet high in raw egg whites caused toxic symptoms in dogs, cats, rabbits, and humans.[28] This study was followed in 1927 by Margaret Averil Boas, who found that a diet of only egg whites caused dermatitis, alopecia, and loss of muscular coordination in rats.[29] She called this syndrome "egg white injury". In 1939, six years after he began investigating the cause of egg white injury, Hungarian scientist Paul Gyorgy confirmed the existence of a protecting factor, which he called vitamin H.[30] By this point, many independent groups had isolated the same compound. In 1936, Kögl and Tönnis isolated a growth factor from egg yolk they called "Bios aus Eigelb."[31] After experiments performed with yeast and Rhizobium R, West and Wilson isolated a compound they called co-enzyme R.[32] In 1940, Gyorgy proved that vitamin H, Bios aus Eigelb and coenzyme R were the same substance: biotin.[33]
Use in biotechnology
Biotin is widely used throughout the biotechnology industry to conjugate proteins for biochemical assays.[34] Biotin's small size means the biological activity of the protein will most likely be unaffected. This process is called biotinylation. Because both streptavidin and avidin bind biotin with high affinity (Kd of 10−14 to 10−15 M) and specificity, biotinylated proteins of interest can be isolated from a sample by exploiting this highly stable interaction. The sample is incubated with streptavidin/avidin beads, allowing the capture of the biotinylated protein of interest. Any other proteins binding to the biotinylated molecule will also stay with the bead and all other unbound proteins can be washed away. However, due to the extremely strong streptavidin-biotin interaction, very harsh conditions are needed to elute the biotinylated protein from the beads (typically 6 M guanidine HCl at pH 1.5), which often will denature the protein of interest. To circumvent this problem, beads conjugated to monomeric avidin can be used, which has a decreased biotin-binding affinity of ≈10−8 M, allowing the biotinylated protein of interest to be eluted with excess free biotin.
Interference with medical laboratory results
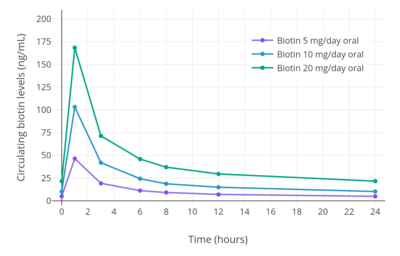
When people are ingesting high levels of biotin in dietary supplements a consequence can be clinically significant interference with diagnostic blood test results.[2][35]
See also
- Biotinylation
- Multiple carboxylase deficiency
- NeutrAvidin
- Photobiotin
References
- Merck Index, 11th Edition, 1244.
- "Biotin – Fact Sheet for Health Professionals". Office of Dietary Supplements, US National Institutes of Health. 8 December 2017. Retrieved 25 February 2018.
- "Biotin". Micronutrient Information Center, Linus Pauling Institute, Oregon State University, Corvallis, OR. 21 October 2015. Retrieved 16 January 2018.
- Fiume MZ (2001). "Final report on the safety assessment of biotin". International Journal of Toxicology. 20 Suppl 4: 1–12. PMID 11800048.
- "Vitamin H (Biotin)". University of Maryland Medical Center. 1 June 2011. Retrieved 4 May 2012.
- Otten JJ, Hellwig JP, Meyers LD, eds. (2006). Dietary Reference Intakes: The Essential Guide to Nutrient Requirements. The National Academies Press. ISBN 0-309-10091-7.
- "National Health and Medical Research Council: Nutrient Reference Values for Australia and New Zealand" (PDF). Archived from the original (PDF) on 2017-01-21. Retrieved 2010-02-19.
- Zempleni J, Hassan YI, Wijeratne SS (November 2008). "Biotin and biotinidase deficiency". Expert Review of Endocrinology & Metabolism. 3 (6): 715–724. doi:10.1586/17446651.3.6.715. PMC 2726758. PMID 19727438.
- Waldrop GL, Holden HM, St Maurice M (November 2012). "The enzymes of biotin dependent CO₂ metabolism: what structures reveal about their reaction mechanisms". Protein Science. 21 (11): 1597–619. doi:10.1002/pro.2156. PMC 3527699. PMID 22969052.
- Marquet A, Bui BT, Florentin D (2001). "Biosynthesis of biotin and lipoic acid". Cofactor Biosynthesis. Vitamins & Hormones. 61. pp. 51–101. doi:10.1016/S0083-6729(01)61002-1. ISBN 978-0-12-709861-6. PMID 11153271.
- Zempleni J, Wijeratne SS, Hassan YI (2009). "Biotin". BioFactors. 35 (1): 36–46. doi:10.1002/biof.8. PMC 4757853. PMID 19319844.
- Chapman-Smith A, Cronan JE (February 1999). "Molecular biology of biotin attachment to proteins". The Journal of Nutrition. 129 (2S Suppl): 477S–484S. doi:10.1093/jn/129.2.477S. PMID 10064313.
- Hymes J, Fleischhauer K, Wolf B (October 1995). "Biotinylation of histones by human serum biotinidase: assessment of biotinyl-transferase activity in sera from normal individuals and children with biotinidase deficiency". Biochemical and Molecular Medicine. 56 (1): 76–83. doi:10.1006/bmme.1995.1059. PMID 8593541.
- Laitinen OH, Hytönen VP, Nordlund HR, Kulomaa MS (December 2006). "Genetically engineered avidins and streptavidins". Cellular and Molecular Life Sciences. 63 (24): 2992–3017. doi:10.1007/s00018-006-6288-z. PMID 17086379.
- Holmberg A, Blomstergren A, Nord O, Lukacs M, Lundeberg J, Uhlén M (February 2005). "The biotin-streptavidin interaction can be reversibly broken using water at elevated temperatures". Electrophoresis. 26 (3): 501–10. doi:10.1002/elps.200410070. PMID 15690449.
- Institute of Medicine (1998). "Biotin". Dietary Reference Intakes for Thiamin, Riboflavin, Niacin, Vitamin B6, Folate, Vitamin B12, Pantothenic Acid, Biotin, and Choline. Washington, DC: The National Academies Press. pp. 374–389. ISBN 0-309-06554-2. Retrieved 2017-08-29.
- "Overview on Dietary Reference Values for the EU population as derived by the EFSA Panel on Dietetic Products, Nutrition and Allergies" (PDF). 2017.
- "Federal Register May 27, 2016 Food Labeling: Revision of the Nutrition and Supplement Facts Labels" (PDF).
- "Changes to the Nutrition Facts Panel - Compliance Date"
- "Tolerable Upper Intake Levels For Vitamins And Minerals" (PDF). European Food Safety Authority. 2006.
- Staggs CG, Sealey WM, McCabe BJ, Teague AM, Mock DM (December 2004). "Determination of the biotin content of select foods using accurate and sensitive HPLC/avidin binding". Journal of Food Composition and Analysis. 17 (6): 767–776. doi:10.1016/j.jfca.2003.09.015. PMC 1450323. PMID 16648879.
- Gropper SS, Smith JL, Groff JL (2005). Advanced nutrition and human metabolism. Belmont. ISBN 0-534-55986-7.
- Combs GF (2008). The Vitamins: Fundamental Aspects in Nutrition and Health. San Diego: Elsevier, Inc. ISBN 978-0-12-183493-7.
- Bowman BA, Russell RM, eds. (2006). "Biotin". Present Knowledge in Nutrition, Ninth Edition, Vol 1. Washington, DC: International Life Sciences Institute. ISBN 978-1-57881-198-4.
- "Biotin: MedlinePlus Supplements". 13 September 2013. Retrieved 2013-09-29.
- "Biotin: Uses, Side Effects, Interactions, Dosage, and Warning". www.webmd.com. Retrieved 2020-02-20.
- Wolf B, Grier RE, Secor McVoy JR, Heard GS (1985). "Biotinidase deficiency: a novel vitamin recycling defect". Journal of Inherited Metabolic Disease. 8 (Suppl 1): 53–8. doi:10.1007/BF01800660. PMID 3930841.
- Bateman WG (June 1916). "The Digestibility and Utilization of Egg Proteins". Journal of Biological Chemistry. 26: 263–91.
- Boas M (1927). "The effect of desiccation on the nutrient value of the protein". Biochemical Journal. 21 (3): 712–24. doi:10.1042/bj0210712. PMC 1251968. PMID 16743887.
- Gyorgy P (December 1939). "The Curative Factor (vitamin H) for Egg White Injury, with Particular Reference to Its Presence in Different Foodstuffs and in Yeast". Journal of Biological Chemistry. 131: 733–44.
- Kögl and Tönnis (1936). "Über das Bios-Problem. Darstellung von krystallisiertem Biotin aus Eigelb. 20. Mitteilung über pflanzliche Wachstumsstoffe". Hoppe-Seyler's Zeitschrift für Physiologische Chemie. 242 (1–2): 43–73. doi:10.1515/bchm2.1936.242.1-2.43.
- West PM, Wilson PW (June 1939). "The Relation of "coenzyme R" to Biotin". Science. 89 (2322): 607–8. Bibcode:1939Sci....89..607W. doi:10.1126/science.89.2322.607. PMID 17751623.
- György P, Rose CS, Eakin RE, Snell EE, Williams RJ (May 1941). "Egg-White Injury as the Result of Nonabsorption or Inactivation of Biotin". Science. 93 (2420): 477–8. Bibcode:1941Sci....93..477G. doi:10.1126/science.93.2420.477. PMID 17757050.
- "Overview of Protein Labeling". Thermo Fisher Scientific. Retrieved 22 April 2012.
- "The FDA Warns that Biotin May Interfere with Lab Tests: FDA Safety Communication". US Food and Drug Administration. 28 November 2017. Retrieved 11 December 2017.