Hyaluronidase
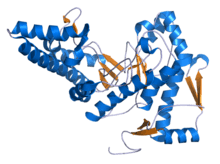
Hyaluronidases are a family of enzymes that catalyse the degradation of hyaluronic acid (HA). Karl Meyer classified these enzymes in 1971, into three distinct groups, a scheme based on the enzyme reaction products.[1] The three main types of hyaluronidases are two classes of eukaryotic endoglycosidase hydrolases and a prokaryotic lyase-type of glycosidase.[2]
| Hyaluronidase | |||||||||
|---|---|---|---|---|---|---|---|---|---|
 | |||||||||
| Identifiers | |||||||||
| EC number | 3.2.1.35 | ||||||||
| CAS number | 37326-33-3 | ||||||||
| Databases | |||||||||
| IntEnz | IntEnz view | ||||||||
| BRENDA | BRENDA entry | ||||||||
| ExPASy | NiceZyme view | ||||||||
| KEGG | KEGG entry | ||||||||
| MetaCyc | metabolic pathway | ||||||||
| PRIAM | profile | ||||||||
| PDB structures | RCSB PDB PDBe PDBsum | ||||||||
| Gene Ontology | AmiGO / QuickGO | ||||||||
| |||||||||
| Hyaluronidase | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Identifiers | |||||||||
| Symbol | Hyaluronidase_1 | ||||||||
| Pfam | PF07212 | ||||||||
| InterPro | IPR009860 | ||||||||
| |||||||||
| Hyaluronidase | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Identifiers | |||||||||
| Symbol | Hyaluronidase_2 | ||||||||
| Pfam | PF07555 | ||||||||
| InterPro | IPR011496 | ||||||||
| |||||||||
In humans, there are five functional hyaluronidases: HYAL1, HYAL2, HYAL3, HYAL4 and HYAL5 (also known as SPAM1 or PH-20); plus a pseudogene, HYAL6 (also known as HYALP1).[3][4] The genes for HYAL1-3 are clustered in chromosome 3, while HYAL4-6 are clustered in chromosome 7.[3] HYAL1 and HYAL2 are the major hyaluronidases in most tissues. GPI-anchored HYAL2 is responsible for cleaving high-molecular weight HA, which is mostly bound to the CD44 receptor. The resulting HA fragments of variable size are then further hydrolized by HYAL1 after being internalized into endo-lysosomes; this generates HA oligosaccharides.[5]
According to their enzymatic mechanism, hyaluronidases are hyaluronoglucosidases (EC 3.2.1.35), i.e. they cleave the (1->4)-linkages between N-acetylglucosamine and glucuronate. The term hyaluronidase may also refer to hyaluronoglucuronidases (EC 3.2.1.36), which cleave (1->3)-linkages. In addition, bacterial hyaluronate lyases (EC 4.2.2.1) may also be referred to as hyaluronidases, although this is uncommon.[6]
Use as a drug
| Clinical data | |
|---|---|
| Trade names | Hylenex, HyQvia, Vitrase, others |
| AHFS/Drugs.com | Professional Drug Facts |
| License data | |
| Pregnancy category | |
| Routes of administration | Subcutaneous |
| ATC code | |
| Legal status | |
| Legal status | |
| Identifiers | |
| |
| CAS Number | |
| DrugBank | |
| ChemSpider |
|
| UNII | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | C2455H3775N617O704S21 |
| Molar mass | 53871.08 g·mol−1 |
| | |
Medical uses
Hyaluronidase ovine (Vitrase) was approved for use in the United States in May 2004.[10] It is a preparation of purified ovine testicular hyaluronidase.[11] It is an endoglycosidase and is indicated as an adjuvant in subcutaneous fluid administration for achieving hydration, for increasing the dispersion and absorption of other injected drugs, or for improving resorption of radiopaque agents, in subcutaneous urography.[11]
Hyaluronidase bovine (Amphadase) was approved for use in the United States in October 2004.[12] It is a preparation of purified bovine testicular hyaluronidase.[13] It is indicated as an adjuvant in subcutaneous fluid administration for achieving hydration, to increase absorption and dispersion of other injected drugs, or in subcutaneous urography for improving resorption of radiopaque agents.[13]
Hyaluronidase bovine (Hydase) was approved for use in the United States in October 2005.[14] It is a preparation of purified bovine testicular hyaluronidase, a protein enzyme.[15] It is indicated as an adjuvant to increase the absorption and dispersion of other injected drugs.[15]
Hyaluronidase human recombinant was approved for use in the United States in December 2005.[16][17] It is a purified preparation of the enzyme recombinant human hyaluronidase and is produced by genetically engineered Chinese Hamster Ovary (CHO) cells containing a DNA plasmid encoding for a soluble fragment of human hyaluronidase (PH20).[18] It is an endoglycosidase and is indicated as an adjuvant in subcutaneous fluid administration for achieving hydration, to increase the dispersion and absorption of other injected drugs, or in subcutaneous urography for improving resorption of radiopaque agents.[18]
Hyaluronidase recombinant human kit was approved for use in the European Union in May 2013,[19] and in the United States in September 2014.[20][21] It is a dual vial unit with one vial of immune globulin infusion 10% (human) and one vial of recombinant human hyaluronidase.[22] It is an immune globulin with a recombinant human hyaluronidase indicated in the United States for the treatment of primary immunodeficiency in adults. This includes, but is not limited to, common variable immunodeficiency, X-linked agammaglobulinemia, congenital agammaglobulinemia, Wiskott-Aldrich syndrome, and severe combined immunodeficiencies.[22] In the European Union it is indicated as replacement therapy in adults, children and adolescents (0-18 years) in:
- Primary immunodeficiency syndromes with impaired antibody production.[19]
- Hypogammaglobulinaemia and recurrent bacterial infections in patients with chronic lymphocytic leukaemia (CLL), in whom prophylactic antibiotics have failed or are contra‑indicated.[19]
- Hypogammaglobulinaemia and recurrent bacterial infections in multiple myeloma (MM) patients.[19]
- Hypogammaglobulinaemia in patients pre‑ and post‑allogeneic hematopoietic stem cell transplantation (HSCT).[19]
By catalyzing the hydrolysis of hyaluronan, a constituent of the extracellular matrix (ECM), hyaluronidase lowers the viscosity of hyaluronan, thereby increasing tissue permeability. It is, therefore, used in medicine in conjunction with other drugs to speed their dispersion and delivery. Common applications are ophthalmic surgery, in combination with local anesthetics. It also increases the absorption rate of parenteral fluids given by hypodermoclysis, and is an adjunct in subcutaneous urography for improving resorption of radiopaque agents. Hyaluronidase is also used for extravasation of hyperosmolar solutions. Hyalurodinase is used by plastic surgeons and dermatologists to reverse the effects of hyaluronic acid injections used as dermal fillers whenever the patient receiving the injections is unhappy with the results.
A form of subcutaneous immunoglobulin (SCIG) that uses Hylenex to allow for a far greater volume of SCIG to be administered than would normally be possible to administer subcutaneously, providing a form of SCIG that can be dosed on a monthly basis, a longer period of time than other forms of SCIG allow. HyQvia had a rate of systemic adverse effects higher than traditional subcutaneous forms of immunoglobulin injection, but lower than those typical in IVIG patients.[23] Also in epidural lysis of adhesions for pain management.
Hyaluronidase is a recommended antidote for vinca alkaloid overdose or extravasation.[24]
Hyaluronidase is available in some fixed-dose combination drug products in the United States: rituximab/hyaluronidase (Rituxan Hycela), trastuzumab/hyaluronidase-oysk (Herceptin Hylecta), daratumumab/hyaluronidase-fihj (Darzalex Faspro).[25][26][27][28][29]
Role in cancer
The role of hyaluronidases in cancer has been historically controversial due to contradictory observations,[30] namely that levels of hyaluronidase (HYAL1/2) are increased in some cancers (colorectal,[31] bladder, prostate, breast and brain), whereas low expression of HYAL1 is correlated with a decrease in survival of pancreatic adenocarcinoma patients.[32] The reason for this apparent contradiction is that both the accumulation of HA (due to increased HAS levels and decreased HYAL levels), and the degradation of HA into HA oligosaccharides by high HYAL levels result in increased tumor malignancy.[5]
Elevated tissue expression of hyaluronic acid and hyaluronidase validates the HA-HAase urine test for bladder cancer.[33] Limited data support a role of lysosomal hyaluronidases in metastasis, while other data support a role in tumor suppression. Other studies suggest no contribution or effects independent of enzyme activity. Non-specific inhibitors (apigenin, sulfated glycosaminoglycans) or crude enzyme extracts have been used to test most hypotheses, making data difficult to interpret. It has been hypothesized that, by helping degrade the ECM surrounding the tumor, hyaluronidases help cancer cells escape from primary tumor masses. However, studies show that removal of hyaluronan from tumors prevents tumor invasion. Hyaluronidases are also thought to play a role in the process of angiogenesis, although most hyaluronidase preparations are contaminated with large amounts of angiogenic growth factors.[34]
Role in pathogenesis
Some bacteria, such as Staphylococcus aureus, Streptococcus pyogenes,[35] and Clostridium perfringens,[36] produce hyaluronidase as a means of using hyaluronan as a carbon source. It is often speculated that Streptococcus and Staphylococcus pathogens use hyaluronidase as a virulence factor to destroy the polysaccharide that holds animal cells together, making it easier for the pathogen to spread through the tissues of the host organism, but no valid experimental data are available to support this hypothesis.
Hyaluronidases are found in the venom of certain lizards and snakes, as well as honeybees, where they are referred to as "spreading factors", having a function akin to bacterial hyaluronidases.[37]
Role in immune response
White blood cells produce hyaluronidase to move more easily through connective tissue to get to infected sites.[38]
Role in fertilization
In mammalian fertilization, hyaluronidase is released by the acrosome of the sperm cell after it has reached the oocyte, by digesting hyaluronan in the corona radiata, thus enabling conception. Gene-targeting studies show that hyaluronidases such as PH20 are not essential for fertilization,[39] although exogenous hyaluronidases can disrupt the cumulus matrix.
The majority of mammalian ova are covered in a layer of granulosa cells intertwined in an extracellular matrix that contains a high concentration of hyaluronan. When a capacitated sperm reaches the ovum, it is able to penetrate this layer with the assistance of hyaluronidase enzymes present on the surface of the sperm. Once this occurs, the sperm is capable of binding with the zona pellucida.[40]
See also
References
- Meyer, K (1971). "Hyaluronidases". In Boyer PD (ed.). Enzymes. V. New York: Academic Press. pp. 307–320. ISBN 978-0-12-122705-0.
- Stern R, Kogan G, Jedrzejas MJ, Soltés L (November 2007). "The many ways to cleave hyaluronan". Biotechnology Advances. 25 (6): 537–57. doi:10.1016/j.biotechadv.2007.07.001. PMID 17716848.
- Csóka AB, Scherer SW, Stern R (September 1999). "Expression analysis of six paralogous human hyaluronidase genes clustered on chromosomes 3p21 and 7q31". Genomics. 60 (3): 356–61. doi:10.1006/geno.1999.5876. PMID 10493834.
- Csoka AB, Frost GI, Stern R (December 2001). "The six hyaluronidase-like genes in the human and mouse genomes". Matrix Biology. 20 (8): 499–508. doi:10.1016/S0945-053X(01)00172-X. PMID 11731267.
- Chanmee T, Ontong P, Itano N (May 2016). "Hyaluronan: A modulator of the tumor microenvironment". Cancer Letters. 375 (1): 20–30. doi:10.1016/j.canlet.2016.02.031. PMID 26921785.
- "Hyaluronidase". ENZYME. ExPASy. Retrieved 17 November 2016.
- "Hyaluronidase Use During Pregnancy". Drugs.com. 14 June 2019. Retrieved 3 February 2020.
- "Hyalase 1500 I.U. Powder for Solution for Injection/Infusion or Hyaluronidase 1500 I.U. Powder for Solution for Injection/Infusion - Summary of Product Characteristics (SmPC)". (emc). 12 March 2015. Retrieved 1 May 2020.
- "HyQvia 100 mg/ml solution for infusion for subcutaneous use - Summary of Product Characteristics (SmPC)". (emc). 15 January 2020. Retrieved 1 May 2020.
- "Drug Approval Package: Vitrase (Hyaluronidase) NDA #021640". U.S. Food and Drug Administration (FDA). 15 November 2004. Retrieved 1 May 2020.
- "Vitrase- hyaluronidase, ovine injection, solution". DailyMed. 29 May 2018. Retrieved 1 May 2020.
- "Drug Approval Package: Amphadase (Hyaluronidase) NDA #021665". U.S. Food and Drug Administration (FDA). 4 February 2005. Retrieved 1 May 2020.
- "Amphadase- hyaluronidase injection". DailyMed. 28 November 2016. Retrieved 1 May 2020.
- "Hydase: FDA-Approved Drugs". U.S. Food and Drug Administration (FDA). 23 March 2020. Retrieved 1 May 2020.
- "Hydase- hyaluronidase injection, solution". DailyMed. 16 November 2015. Retrieved 1 May 2020.
- "Drug Approval Package: Hylenex Recombinant (Hyaluronidase) NDA #021859". U.S. Food and Drug Administration (FDA). 3 January 2006. Retrieved 1 May 2020.
- "Halozyme Therapeutics and Baxter Healthcare Corporation Announce FDA Approval of Hylenex". Archived from the original on October 18, 2007. Retrieved 2008-11-07.
- "Hylenex recombinant (hyaluronidase- human recombinant injection), solution". DailyMed. 1 January 2016. Retrieved 1 May 2020.
- "HyQvia EPAR". European Medicines Agency (EMA). Retrieved 1 May 2020.

- "Hyqvia". U.S. Food and Drug Administration (FDA). 27 February 2015. Archived from the original on 22 July 2017. Retrieved 1 May 2020.
- "Hyqvia Approval Letter". U.S. Food and Drug Administration (FDA). Archived from the original on 22 July 2017. Retrieved 20 November 2015.
- "Hyqvia (immune globulin 10 percent- human with recombinant human hyaluronidase) kit". DailyMed. Retrieved 1 May 2020.
- Sanford M (August 2014). "Human immunoglobulin 10 % with recombinant human hyaluronidase: replacement therapy in patients with primary immunodeficiency disorders". BioDrugs. 28 (4): 411–20. doi:10.1007/s40259-014-0104-3. PMID 24925799.
- "Chemotherapy extravasation guideline" (PDF). WOSCAN Cancer Nursing and Pharmacy Group. September 2009. Retrieved 4 June 2017.
- "Drug Approval Package: Rituxan Hycela". U.S. Food and Drug Administration (FDA). 11 October 2018. Retrieved 1 May 2020.
- "Rituxan Hycela- rituximab and hyaluronidase injection, solution". DailyMed. 3 December 2019. Retrieved 1 May 2020.
- "Drug Approval Package: Herceptin Hylecta". U.S. Food and Drug Administration (FDA). 17 October 2019. Retrieved 1 May 2020.
- "Herceptin Hylecta- trastuzumab and hyaluronidase-oysk injection, solution". DailyMed. 13 May 2019. Retrieved 1 May 2020.
- "Darzalex Faspro: FDA-Approved Drugs". U.S. Food and Drug Administration (FDA). Retrieved 1 May 2020.
- Whatcott CJ, Han H, Posner RG, Hostetter G, Von Hoff DD (September 2011). "Targeting the tumor microenvironment in cancer: why hyaluronidase deserves a second look". Cancer Discovery. 1 (4): 291–6. doi:10.1158/2159-8290.CD-11-0136. PMC 3204883. PMID 22053288.
- Bouga, Helen; Tsouros, Isidoros; Bounias, Dimitrios; Kyriakopoulou, Dora; Stavropoulos, Michael S; Papageorgakopoulou, Nikoletta; Theocharis, Dimitrios A; Vynios, Demitrios H (2010-09-17). "Involvement of hyaluronidases in colorectal cancer". BMC Cancer. Springer Nature. 10 (1): 499. doi:10.1186/1471-2407-10-499. ISSN 1471-2407. PMC 2949809. PMID 20849597.
- Cheng XB, Sato N, Kohi S, Yamaguchi K (2013). "Prognostic impact of hyaluronan and its regulators in pancreatic ductal adenocarcinoma". PLOS ONE. 8 (11): e80765. Bibcode:2013PLoSO...880765C. doi:10.1371/journal.pone.0080765. PMC 3823618. PMID 24244714.
- Hautmann SH, Lokeshwar VB, Schroeder GL, Civantos F, Duncan RC, Gnann R, Friedrich MG, Soloway MS (June 2001). "Elevated tissue expression of hyaluronic acid and hyaluronidase validates the HA-HAase urine test for bladder cancer". The Journal of Urology. 165 (6 Pt 1): 2068–74. doi:10.1016/s0022-5347(05)66296-9. PMID 11371930.
- Rahmanian M, Heldin P (February 2002). "Testicular hyaluronidase induces tubular structures of endothelial cells grown in three-dimensional collagen gel through a CD44-mediated mechanism". International Journal of Cancer. 97 (5): 601–7. doi:10.1002/ijc.10087. PMID 11807784.
- Starr CR, Engleberg NC (January 2006). "Role of hyaluronidase in subcutaneous spread and growth of group A streptococcus". Infection and Immunity. 74 (1): 40–8. doi:10.1128/IAI.74.1.40-48.2006. PMC 1346594. PMID 16368955.
- Zukaite V, Biziulevicius GA (March 2000). "Acceleration of hyaluronidase production in the course of batch cultivation of Clostridium perfringens can be achieved with bacteriolytic enzymes". Letters in Applied Microbiology. 30 (3): 203–6. doi:10.1046/j.1472-765x.2000.00693.x. PMID 10747251.
- Isoyama T, Thwaites D, Selzer MG, Carey RI, Barbucci R, Lokeshwar VB (January 2006). "Differential selectivity of hyaluronidase inhibitors toward acidic and basic hyaluronidases". Glycobiology. 16 (1): 11–21. doi:10.1093/glycob/cwj036. PMID 16166602.
- Tortora, Gerard J. (2013-12-31). Principles of anatomy & physiology. Derrickson, Bryan (14th ed.). Danvers, MA. ISBN 978-1-118-34500-9. OCLC 871018672.
- Baba D, Kashiwabara S, Honda A, Yamagata K, Wu Q, Ikawa M, Okabe M, Baba T (August 2002). "Mouse sperm lacking cell surface hyaluronidase PH-20 can pass through the layer of cumulus cells and fertilize the egg". The Journal of Biological Chemistry. 277 (33): 30310–4. doi:10.1074/jbc.M204596200. PMID 12065596.
- Alberts B (2008). Molecular biology of the cell. New York: Garland Science. p. 1298. ISBN 978-0-8153-4105-5.
External links

- "Hyaluronidase". Drug Information Portal. U.S. National Library of Medicine.
- "Hyaluronidase (Human recombinant)". Drug Information Portal. U.S. National Library of Medicine.
- "Hyaluronidase (ovine)". Drug Information Portal. U.S. National Library of Medicine.
- "Hyaluronidase mixture with Rituximab". Drug Information Portal. U.S. National Library of Medicine.
- "Rituximab and Hyaluronidase Human Injection". MedlinePlus.
- "Trastuzumab and hyaluronidase-oysk Injection". MedlinePlus.
- Hyaluronidase at the US National Library of Medicine Medical Subject Headings (MeSH)