Patellofemoral pain syndrome
| Patellofemoral pain syndrome | |
|---|---|
| Synonyms | Patellar overload syndrome, runner's knee |
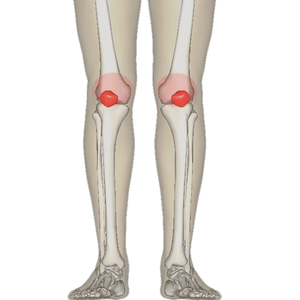 | |
| Diagram of the bones of the lower extremity. Rough distribution of areas affected by PFPS highlighted in red: patella and distal femur. | |
| Specialty | Orthopedics, sports medicine |
Patellofemoral pain syndrome (PFPS), also known as runner's knee, is a condition characterized by knee pain ranging from severe to mild discomfort seemingly originating from the contact of the posterior surface of the patella (back of the kneecap) with the femur (thigh bone). It is "anterior knee pain involving the patella and retinaculum that excludes other intra-articular and peri-patellar pathology".[1]
The population most at risk from PFPS are runners, cyclists, basketball players and other sports participants. Onset can be gradual or the result of a single incident and is often caused by a change in training regimen that includes dramatic increases in training time, distance or intensity, it can be compounded by worn or the wrong type of footwear.[1] Symptoms include discomfort while sitting with bent knees or descending stairs and generalised knee pain.[2] Treatment involves resting and physical therapy that includes stretching and strengthening exercises for the legs.
Signs and symptoms
The onset of the condition is usually gradual,[3] although some cases may appear suddenly following trauma.[1]
- Knee pain - the most common symptom is diffuse peripatellar pain (vague pain around the kneecap) and localized retropatellar pain (pain focused behind the kneecap). Affected individuals typically have difficulty describing the location of the pain, and may place their hands over the anterior patella or describe a circle around the patella (the "circle sign").[1] Pain is usually initiated when load is put on the knee extensor mechanism, e.g. ascending or descending stairs or slopes, squatting, kneeling, cycling, running or prolonged sitting with flexed (bent) knees.[4][5][6] The latter feature is sometimes termed the "movie sign" or "theatre sign" because individuals might experience pain while sitting to watch a film or similar activity.[4] The pain is typically aching with occasional sharp pains.[1]
- Crepitus (joint noises)[4] may be present (but not have relation with pain and function) [7][8]
- Giving-way of the knee[4] may be reported
Causes
In most patients with PFPS an examination of their history will highlight a precipitating event that caused the injury. Changes in activity patterns such as excessive increases in running mileage, repetitions such as running up steps and the addition of strength exercises that affect the patellofemoral joint are commonly associated with symptom onset. Excessively worn or poorly fitted footwear may be a contributing factor. To prevent recurrence the causal behaviour should be identified and managed correctly.[1]
The medical cause of PFPS is thought to be increased pressure on the patellofemoral joint.[4] There are several theorized mechanisms relating to how this increased pressure occurs:
- Increased levels of physical activity[4]
- Malalignment of the patella as it moves through the femoral groove[4]
- Quadriceps muscle imbalance[4]
- Tight anatomical structures, e.g. retinaculum or iliotibial band.[4]
Causes can also be a result of excessive genu valgum and the above mentioned repetitive motions leading to abnormal lateral patellar tracking. Individuals with genu valgum have larger than normal Q-angles causing the weight-bearing line to fall lateral to the centre of the knee causing overstretching of the MCL and stressing the lateral meniscus and cartilages.
The cause of pain and dysfunction often results from either abnormal forces (e.g. increased pull of the lateral quadriceps retinaculum with acute or chronic lateral PF subluxation/dislocation) or prolonged repetitive compressive or shearing forces (running or jumping) on the PF joint. The result is synovial irritation and inflammation and subchondral bony changes in the distal femur or patella known as "bone bruises". Secondary causes of PF Syndrome are fractures, internal knee derangement, osteoarthritis of the knee and bony tumors in or around the knee.[9]
Diagnosis
Examination
Patients can be observed standing and walking to determine patellar alignment.[2] The Q-angle, lateral hypermobility, and J-sign are commonly used determined to determine patellar maltracking.[10] The patellofemoral glide, tilt, and grind tests (Clarke's sign), when performed, can provide strong evidence for PFPS.[1][11] Lastly, lateral instability can be assessed via the patellar apprehension test, which is deemed positive when there is pain or discomfort associated with lateral translation of the patella.[1][2]
Differential diagnosis
The diagnosis of patellofemoral pain syndrome is made by ruling out patellar tendinitis, prepatellar bursitis, plica syndrome, Sinding-Larsen and Johansson syndrome, and Osgood–Schlatter disease.[12]
Classification
Runner's knee
PFPS is one of a handful of conditions sometimes referred to as runner's knee;[1] the other conditions being Chondromalacia patellae, Iliotibial band syndrome, and Plica syndrome.
Chondromalacia patellae
Chondromalacia patellae is a term sometimes treated synonymously with PFPS.[4] However, there is general consensus that PFPS applies only to individuals without cartilage damage,[4] thereby distinguishing it from chondromalacia patellae, a condition characterized by softening of the patellar articular cartilage.[1] Despite this academic distinction, the diagnosis of PFPS is typically made clinically, based only on the history and physical examination rather than on the results of any medical imaging. Therefore, it is unknown whether most persons with a diagnosis of PFPS have cartilage damage or not, making the difference between PFPS and chondromalacia theoretical rather than practical.[4] It is thought that only some individuals with anterior knee pain will have true chondromalacia patellae.[1]
Treatment
As patellofemoral pain syndrome is the most common cause of anterior knee pain in the outpatient,[1] a variety of treatments for patellofemoral pain syndrome are implemented.[13] Most patients with patellofemoral pain syndrome respond well to conservative therapy.[13][14]
Exercises
There is consistent but very low quality evidence that exercise therapy for PFPS reduces pain, improves function and aids long-term recovery.[15] However, there is insufficient evidence to compare the effectiveness of different types of exercises with each other, and exercises with other forms of treatment.[15]
Exercise therapy is the recommended first line treatment of PFPS.[1] Various exercises have been studied and recommended.[16] Exercises are described according to 3 parameters:[5]
- Type of muscle activity (concentric, eccentric or isometric)
- Type of joint movement (dynamic, isometric or static)
- Reaction forces (closed or open kinetic chain)
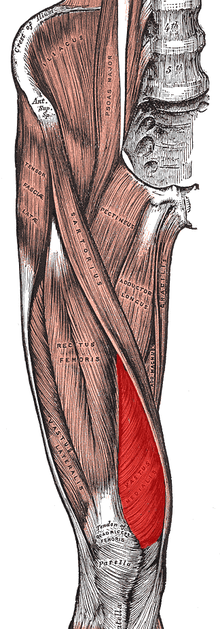
The majority of exercise programs intended to treat PFPS are designed to strengthen the quadriceps muscles.[5] Quadriceps strengthening is considered to be the "gold" standard treatment for PFPS.[13] Quadriceps strengthening is commonly suggested because the quadriceps muscles help to stabilize the patella. Quadriceps weakness and muscle imbalance may contribute to abnormal patellar tracking.[13]
If the strength of the vastus medialis muscle is inadequate, the usually larger and stronger vastus lateralis muscle will pull sideways (laterally) on the kneecap. Strengthening the vastus medialis to prevent or counter the lateral force of the vastus lateralis is one way of relieving PFPS. However, there is growing evidence that support more proximal factors play a much larger role than vastus medialis (VMO) strength deficits or quadriceps imbalance. Hip Abductor, Extensor, and External Rotator weakness (particularly gluteus Maximus and Medius) appear to be prevalent in PPS and strengthening in these areas has demonstrated significant symptom reduction in many patients with PPS as well as helped prevent future more serious injuries such as non contact ACL tears in athletes. <Reference: The Influence of Abnormal Hip Mechanics on Knee Injury: A Biomechanical Perspective. Christopher M. Powers. Journal of Orthopaedic and Sports Physical Therapy 40(2), 42-51, 2010.>. <Anterior Cruciate Ligament Injury Prevention Training in Female Athletes: A Systematic Review of Injury Reduction and Results of Athletic Performance Tests. Frank R Noyes, Sue D Barber Westin. Sports Health 4 (1), 36-46, 2012.
Emphasis during exercise may be placed on coordinated contraction of the medial and lateral parts of the quadriceps as well as of the hip adductor, hip abductor and gluteal muscles.[5] Many exercise programs include stretches designed to improve lower limb flexibility.[5] Electromyographic biofeedback allows visualization of specific muscle contractions and may help individuals performing the exercises to target the intended muscles during the exercise.[5] Electrostimulation may be used to apply external stimuli resulting in contraction of specific muscles and thus exercise.[4]
Inflexibility has often been cited as a source of patellofemoral pain syndrome. Stretching of the laterial knee has been suggested to help.[17]
Medication
Non-steroidal anti-inflammatory drugs (NSAIDs) are widely used to treat PFPS, however there is only very limited evidence that they are effective.[4] NSAIDs may reduce pain in the short term, overall however, after three months pain is not improved.[18] There is no evidence that one type of NSAID is superior to another in PFPS, and therefore some authors have recommended that the NSAID with fewest side effects and which is cheapest should be used.[4]
Glycosaminoglycan polysulfate (GAGPS) inhibits proteolytic enzymes and increases synthesis and degree of polymerization of hyaluronic acid in synovial fluid.[4] There is contradictory evidence that it is effective in PFPS.[4]
Medical imaging
Magnetic resonance imaging rarely can give useful information for managing patellofemoral pain syndrome and treatment should focus on an appropriate rehabilitation program including correcting strength and flexibility concerns.[19] In the uncommon cases where a patient has mechanical symptoms like a locked knee, knee effusion, or failure to improve following physical therapy, then an MRI may give more insight into diagnosis and treatment.[19]
Rest
Patellofemoral pain syndrome may also result from overuse or overload of the PF joint. For this reason, knee activity should be reduced until the pain is resolved.[20][21]
Braces and taping
There is no statistically or clinically significant difference in pain symptoms between taping and non-taping in individuals with PFPS.[18]
Knee braces are ineffective in treating PFPS.[18] The technique of McConnell taping involves pulling the patella medially with tape (medial glide). Findings from some studies suggest that there is limited benefit with patella taping or bracing when compared to quadriceps exercises alone.[13]
Foot orthoses
Low arches can cause overpronation or the feet to roll inward too much increasing load on the patellofemoral joint. Poor lower extremity biomechanics may cause stress on the knees and can be related to the development of patellofemoral pain syndrome, although the exact mechanism linking joint loading to the development of the condition is not clear. Foot orthoses can help to improve lower extremity biomechanics and may be used as a component of overall treatment.[22][23] Foot orthoses may be useful for reducing knee pain in the short term,[24] and may be combined with exercise programs or physical therapy.
Surgery
The scientific consensus is that surgery should be avoided except in very severe cases in which conservative treatments fail.[4] The majority of individuals with PFPS receive nonsurgical treatment.[5]
Alternative medicine
There is no evidence to support the use of acupuncture or low-level laser therapy to treat PFPS.[25] Most studies touting the benefits of alternative therapies for PFPS were conducted with flawed experimental design, and therefore did not produce reliable results.[26]
Epidemiology
Specific populations at high risk of primary PFPS include runners, bicyclists, basketball players, young athletes and females.[27]
See also
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 Dixit, S; DiFiori, JP; Burton, M; Mines, B (Jan 15, 2007). "Management of patellofemoral pain syndrome". American Family Physician. 75 (2): 194–202. PMID 17263214.
- 1 2 3 Essentials of musculoskeletal care. Sarwark, John F. Rosemont, Ill.: American Academy of Orthopaedic Surgeons. 2010. ISBN 9780892035793. OCLC 706805938.
- ↑ Callaghan, MJ; Selfe, J (Apr 18, 2012). "Patellar taping for patellofemoral pain syndrome in adults". The Cochrane Database of Systematic Reviews. 4: CD006717. doi:10.1002/14651858.CD006717.pub2. PMID 22513943.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Heintjes, E; Berger, MY; Bierma-Zeinstra, SM; Bernsen, RM; Verhaar, JA; Koes, BW (2004). "Pharmacotherapy for patellofemoral pain syndrome". The Cochrane Database of Systematic Reviews (3): CD003470. doi:10.1002/14651858.CD003470.pub2. PMID 15266488.
- 1 2 3 4 5 6 7 van der Heijden RA, Lankhorst NE, van Linschoten R, Bierma-Zeinstra SM, van Middelkoop M (2013). "Exercise for treating patellofemoral pain syndrome (Protocol)". Cochrane Database of Systematic Reviews. 2: CD010387. doi:10.1002/14651858.CD010387.
- ↑ Smith TO, Drew BT, Meek TH, Clark AB (2013). "Knee orthoses for treating patellofemoral pain syndrome (Protocol)". Cochrane Database of Systematic Reviews. 5: CD010513. doi:10.1002/14651858.CD010513.
- ↑ de Oliveira DS, Pazzinato MF, Del Priore LB, Ferreira AS, Briani RV, Ferrari D, Bazett-Jones D, de Azevedo FM (2018). ""Knee crepitus is prevalent in women with patellofemoral pain, but is not related with function, physical activity and pain"". Physical Therapy in Sport. 33: 7-11. doi:10.1016/j.ptsp.2018.06.002.
- ↑ de Oliveira Silva D, Barton C, Crossley K, Waiteman M, Taborda B, Ferreira AS, de Azevedo FM (2018). ""Implications of knee crepitus to the overall clinical presentation of women with and without patellofemoral pain"". Physical Therapy in Sport. 33: 89-95. doi:10.1016/j.ptsp.2018.07.007.
- ↑ Plamondon, Tom (12 Aug 2009). "Special tests in the clinical examination of patellofemoral syndrome". Doctors Lounge. Retrieved 2012-08-20.
- ↑ Sheehan, Frances T.; Derasari, Aditya; Fine, Kenneth M.; Brindle, Timothy J.; Alter, Katharine E. (January 2010). "Q-angle and J-sign: Indicative of Maltracking Subgroups in Patellofemoral Pain". Clinical Orthopaedics and Related Research. 468 (1): 266–275. doi:10.1007/s11999-009-0880-0. ISSN 0009-921X. PMC 2795830. PMID 19430854.
- ↑ Gerard A. Malanga, Scott F. Nadler (2006). Musculoskeletal physical examination : an evidence-based approach. Philadelphia, Penns.: Elsevier Mosby. pp. 302–304. ISBN 9781560535911.
- ↑ Prins, Maarten R.; Van Der Wurff, Peter (2009). "Females with patellofemoral is fine pain syndrome have weak hip muscles: A systematic review". Australian Journal of Physiotherapy. 55 (1): 9–15. doi:10.1016/S0004-9514(09)70055-8. PMID 19226237.
- 1 2 3 4 5 Bolgla, LA; Boling, MC (2011). "An update for the conservative management of patellofemoral pain syndrome: A systematic review of the literature from 2000 to 2010". International journal of sports physical therapy. 6 (2): 112–25. PMC 3109895. PMID 21713229.
- ↑ Earl, JE; Vetter, CS (Aug 2007). "Patellofemoral pain". Physical Medicine and Rehabilitation Clinics of North America. 18 (3): 439–58, viii. doi:10.1016/j.pmr.2007.05.004. PMID 17678761.
- 1 2 van der Heijden, RA; Lankhorst, NE; van Linschoten, R; Bierma-Zeinstra, SM; van Middelkoop, M (20 January 2015). "Exercise for treating patellofemoral pain syndrome". The Cochrane Database of Systematic Reviews. 1: CD010387. doi:10.1002/14651858.CD010387.pub2. PMID 25603546.
- ↑ van der Heijden, Rianne A; Lankhorst, Nienke E; van Linschoten, Robbart; Bierma-Zeinstra, Sita MA; van Middelkoop, Marienke; van Middelkoop, Marienke (2013). "Exercise for treating patellofemoral pain syndrome". Reviews. doi:10.1002/14651858.CD010387.
- ↑ Arendt, edited by Stefano Zaffagnini, David Dejour, Elizabeth A. (2010). Patellofemoral pain, instability, and arthritis clinical presentation, imaging, and treatment. Berlin: Springer. p. 134. ISBN 9783642054242.
- 1 2 3 Rodriguez-Merchan, EC (Mar 2014). "Evidence Based Conservative Management of Patello-femoral Syndrome". Archives of bone and joint surgery. 2 (1): 4–6. PMC 4151435. PMID 25207305.
- 1 2 American Medical Society for Sports Medicine (24 April 2014), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American Medical Society for Sports Medicine, retrieved 29 July 2014
, which cites
- Rixe, JA; Glick, JE; Brady, J; Olympia, RP (Sep 2013). "A review of the management of patellofemoral pain syndrome". The Physician and Sportsmedicine. 41 (3): 19–28. doi:10.3810/psm.2013.09.2023. PMID 24113699.
- ↑ Thomeé, R.; Renström, P.; Karlsson, J.; Grimby, G. (2007). "Patellofemoral pain syndrome in young women". Scandinavian Journal of Medicine & Science in Sports. 5 (4): 237–44. doi:10.1111/j.1600-0838.1995.tb00040. PMID 7552769.
- ↑ Tria Jr, AJ; Palumbo, RC; Alicea, JA (1992). "Conservative care for patellofemoral pain". The Orthopedic clinics of North America. 23 (4): 545–54. PMID 1408039.
- ↑ Gross, M. L.; Davlin, L. B.; Evanski, P. M. (1991). "Effectiveness of orthotic shoe inserts in the long-distance runner". The American Journal of Sports Medicine. 19 (4): 409–12. doi:10.1177/036354659101900416. PMID 1897659.
- ↑ Eng, JJ; Pierrynowski, MR (1993). "Evaluation of soft foot orthotics in the treatment of patellofemoral pain syndrome". Physical therapy. 73 (2): 62–8, discussion 68–70. PMID 8421719.
- ↑ Hossain, M; Alexander, P; Burls, A; Jobanputra, P (19 January 2011). "Foot orthoses for patellofemoral pain in adults". The Cochrane Database of Systematic Reviews (1): CD008402. doi:10.1002/14651858.CD008402.pub2. PMID 21249707.
- ↑ Crossley, K; Bennell, K; Green, S; McConnell, J (April 2001). "A systematic review of physical interventions for patellofemoral pain syndrome". Clinical Journal of Sport Medicine. 11 (2): 103–10. doi:10.1097/00042752-200104000-00007. PMID 11403109.
- ↑ Bizzini, M; Childs, JD; Piva, SR; Delitto, A (Jan 2003). "Systematic review of the quality of randomized controlled trials for patellofemoral pain syndrome". The Journal of orthopaedic and sports physical therapy. 33 (1): 4–20. doi:10.2519/jospt.2003.33.7.F4. PMID 12570282.
- ↑ Atanda, Alfred; Reddy, Deepak; Rice, Jaime A.; Terry, Michael A. (November 2009). "Injuries and chronic conditions of the knee in young athletes". Pediatrics in Review. 30 (11): 419–428, quiz 429–430. doi:10.1542/pir.30-11-419. ISSN 1526-3347. PMID 19884282.
External links
| Classification | |
|---|---|
| External resources |
- Patellofemoral pain syndrome at Curlie (based on DMOZ)
- Patellofemoral Joint Syndromes Treatment & Management at eMedicine