Adhesive capsulitis of shoulder
| Adhesive capsulitis of the shoulder | |
|---|---|
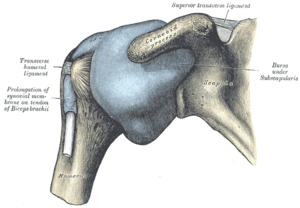 | |
| The right shoulder & glenohumeral joint. | |
| Specialty | Orthopedics |
| Symptoms | Mi d |
Adhesive capsulitis (also known as frozen shoulder) is a painful and disabling disorder of unclear cause in which the shoulder capsule, the connective tissue surrounding the glenohumeral joint of the shoulder, becomes inflamed and stiff, greatly restricting motion and causing chronic pain. Pain is usually constant, worse at night, and with cold weather. Certain movements or bumps can provoke episodes of tremendous pain and cramping. The condition is thought to be caused by injury or trauma to the area and may have an autoimmune component.
Risk factors for frozen shoulder include tonic seizures, diabetes mellitus, stroke, accidents, lung disease, connective tissue diseases, thyroid disease, and heart disease. Treatment may be painful and taxing and consists of physical therapy, occupational therapy, medication, massage therapy, hydrodilatation or surgery. A physician may also perform manipulation under anesthesia, which breaks up the adhesions and scar tissue in the joint to help restore some range of motion. Alternative treatments exist such as the Trigenics OAT Procedure, ART, and the OTZ method. But these can vary in efficacy depending on the type and severity of the frozen shoulder. Pain and inflammation can be controlled with analgesics and NSAIDs.
People who have adhesive capsulitis usually experience severe pain and sleep deprivation for prolonged periods due to pain that gets worse when lying still and restricted movement/positions. The condition can lead to depression, problems in the neck and back, and severe weight loss due to long-term lack of deep sleep. People who have adhesive capsulitis may have difficulty concentrating, working, or performing daily life activities for extended periods of time. The condition tends to be self-limiting and usually resolves over time without surgery. Most people regain about 90% of shoulder motion over time.
Signs and symptoms
Movement of the shoulder is severely restricted, with progressive loss of both active and passive range of motion.[1] The condition is sometimes caused by injury, leading to lack of use due to pain, but also often arises spontaneously with no obvious preceding trigger factor (idiopathic frozen shoulder). Rheumatic disease progression and recent shoulder surgery can also cause a pattern of pain and limitation similar to frozen shoulder. Intermittent periods of use may cause inflammation.
In frozen shoulder, there is a lack of synovial fluid, which normally helps the shoulder joint, a ball and socket joint, move by lubricating the gap between the humerus (upper arm bone) and the socket in the shoulder blade. The shoulder capsule thickens, swells, and tightens due to bands of scar tissue (adhesions) that have formed inside the capsule. As a result, there is less room in the joint for the humerus, making movement of the shoulder stiff and painful. This restricted space between the capsule and ball of the humerus distinguishes adhesive capsulitis from a less complicated, painful, stiff shoulder.[2]
Diagnosis
One sign of a frozen shoulder is that the joint becomes so tight and stiff that it is nearly impossible to carry out simple movements, such as raising the arm. The movement that is most severely inhibited is external rotation of the shoulder.
People complain that the stiffness and pain worsen at night. Pain due to frozen shoulder is usually dull or aching. It can be worsened with attempted motion, or if bumped. A physical therapist, osteopath or chiropractor, physician, physician assistant, or nurse practitioner may suspect the patient has a frozen shoulder if a physical examination reveals limited shoulder movement. Frozen shoulder can be diagnosed if limits to the active range of motion (range of motion from active use of muscles) are the same or almost the same as the limits to the passive range of motion (range of motion from a person manipulating the arm and shoulder). An arthrogram or an MRI scan may confirm the diagnosis, though in practice this is rarely required.
The normal course of a frozen shoulder has been described as having three stages:[3]
- Stage one: The "freezing" or painful stage, which may last from six weeks to nine months, and in which the patient has a slow onset of pain. As the pain worsens, the shoulder loses motion.[4]
- Stage two: The "frozen" or adhesive stage is marked by a slow improvement in pain but the stiffness remains. This stage generally lasts from four to nine months.
- Stage three: The "thawing" or recovery, when shoulder motion slowly returns toward normal. This generally lasts from 5 to 26 months.[5]
MRI and ultrasound
Imaging features of adhesive capsulitis are seen on non-contrast MRI, though MR arthrography and invasive arthroscopy are more accurate in diagnosis.[6] Ultrasound and MRI can help in diagnosis by assessing the coracohumeral ligament, with a width of greater than 3 mm being 60% sensitive and 95% specific for the diagnosis. The condition can also be associated with edema or fluid at the rotator interval, a space in the shoulder joint normally containing fat between the supraspinatus and subscapularis tendons, medial to the rotator cuff. Shoulders with adhesive capsulitis also characteristically fibrose and thicken at the axillary pouch and rotator interval, best seen as dark signal on T1 sequences with edema and inflammation on T2 sequences.[7] A finding on ultrasound associated with adhesive capsulitis is hypoechoic material surrounding the long head of the biceps tendon at the rotator interval, reflecting fibrosis. In the painful stage, such hypoechoic material may demonstrate increased vascularity with Doppler ultrasound.[8]
Prevention
To prevent the problem, a common recommendation is to keep the shoulder joint fully moving to prevent a frozen shoulder. Often a shoulder will hurt when it begins to freeze. Because pain discourages movement, further development of adhesions that restrict movement will occur unless the joint continues to move full range in all directions (adduction, abduction, flexion, rotation, and extension). Physical therapy and occupational therapy can help with continued movement.
However, a 2004 study showed that "supervised neglect" has a higher rate of recovery versus physical therapy and passive stretching.[9]
Management
Management of this disorder focuses on restoring joint movement and reducing shoulder pain, involving medications, physical therapy, and/or surgical intervention. Treatment may continue for months, there is no strong evidence to favor any particular approach.[10]
Medications frequently used include NSAIDs; corticosteroids are used in some cases either through local injection or systemically. Manual therapists like osteopaths, chiropractors and physiotherapists may include massage therapy and daily extensive stretching.[10] Another osteopathic technique used to treat the shoulder is called the Spencer technique.
If these measures are unsuccessful, manipulation of the shoulder under general anesthesia to break up the adhesions is sometimes used.[10] Hydrodilatation or distension arthrography is controversial.[11] Surgery to cut the adhesions (capsular release) may be indicated in prolonged and severe cases; the procedure is usually performed by arthroscopy.[12] Surgical evaluation of other problems with the shoulder, e.g., subacromial bursitis or rotator cuff tear may be needed.
Resistant adhesive capsulitis may respond to open release surgery. This technique allows the surgeon to find and correct the underlying cause of restricted glenohumeral movement such as contracture of coracohumeral ligament and rotator interval.[13]
A study published in 2004 by Diercks and Stevens showed that supervised neglect had a better outcome than intense physical therapy. "Supervised neglect" meant home exercises (pendulum exercises and active exercises within the painless range) and resumption of all activities that were tolerated. "Intense physical therapy" meant passive stretching and manual mobilization together with exercises beyond the pain threshold. Both groups received anti-inflammatory medication (NSAIDs) or analgesics as necessary; neither group received corticosteroid medication or any treatment under anesthesia. The proportion of patients achieving normal or near-normal painless shoulder function at 24 months was 89% in the supervised neglect group, vs 63% in the intense physical therapy group. [9].
Epidemiology
The incidence of adhesive capsulitis is approximately 3 percent in the general population, but some researchers cast doubt on this often cited figure because of how often the disease is misdiagnosed; this would make the disease much rarer than previously thought.[14] Occurrence is rare in children and people under 40 but peaks between 40 and 70 years of age.[10] At least in its idiopathic form, the condition is much more common in women than in men (70% of patients are women aged 40–60). Frozen shoulder is more frequent in diabetic patients and is more severe and more protracted than in the non-diabetic population.[15]
People with diabetes, stroke, lung disease, rheumatoid arthritis, or heart disease are at a higher risk for frozen shoulder. Injury or surgery to the shoulder or arm may cause blood flow damage or the capsule to tighten from reduced use during recovery.[2] Adhesive capsulitis has been indicated as a possible adverse effect of some forms of highly active antiretroviral therapy (HAART). Cases have also been reported after breast and lung surgery.[16]
See also
References
- ↑ Jayson, M. I. V. (1981). "Frozen Shoulder: Adhesive Capsulitis". British Medical Journal (Clinical Research Edition). 283 (6298): 1005–6. doi:10.1136/bmj.283.6298.1005. JSTOR 29503905.
- 1 2 "Frozen shoulder - Causes". Retrieved 2011-07-05.
- ↑ "Your Orthopaedic Connection: Frozen Shoulder". Retrieved 2008-01-28.
- ↑ Burnham M.D., Jeremy. "Frozen Shoulder Diagnosis & Management". Retrieved 25 January 2017.
- ↑ "Reduce Frozen Shoulder Recovery Time". 2016-06-24. Retrieved 2016-07-12.
- ↑ Neviaser TJ. Arthrography of the shoulder. Orthop Clin North Am 1980; 11:205-17
- ↑ Shaikh, A; Sundaram, M (January 2009). "Adhesive capsulitis demonstrated on magnetic resonance imaging". Orthopedics. 32 (1): 2. doi:10.3928/01477447-20090101-20. PMID 19226048.
- ↑ Arend CF. Ultrasound of the Shoulder. Master Medical Books, 2013. Chapter on ultrasound findings of adhesive capsulitis available at ShoulderUS.com
- 1 2 Diercks, RL; Stevens, M. (2004). "Gentle thawing of the frozen shoulder". Journal of Shoulder and Elbow Surgery. 13. doi:10.1016/S1058274604000825. PMID 15383804.
- 1 2 3 4 Ewald, A. (2011). "Adhesive capsulitis: A review". American Family Physician. 83 (4): 417–422. PMID 21322517.
- ↑ Tveitå, Einar Kristian; Tariq, Rana; Sesseng, Solve; Juel, Niels Gunnar; Bautz-Holter, Erik (2008). "Hydrodilatation, corticosteroids and adhesive capsulitis: A randomized controlled trial". BMC Musculoskeletal Disorders. 9: 53. doi:10.1186/1471-2474-9-53. PMC 2374785. PMID 18423042.
- ↑ Baums, M. H.; Spahn, G.; Nozaki, M.; Steckel, H.; Schultz, W.; Klinger, H.-M. (2006). "Functional outcome and general health status in patients after arthroscopic release in adhesive capsulitis". Knee Surgery, Sports Traumatology, Arthroscopy. 15 (5): 638–44. doi:10.1007/s00167-006-0203-x.
- ↑ D’Orsi, Giovanni Maria; Via, Alessio Giai; Frizziero, Antonio; Oliva, Francesco (1911-12-14). "Treatment of adhesive capsulitis: a review". Muscles, Ligaments and Tendons Journal. 2 (2). PMID 23738277. Retrieved 2018-08-17.
- ↑ Bunker, Tim (2009). "Time for a new name for frozen shoulder—contracture of the shoulder". Shoulder&Elbow. doi:10.1111/j.1758-5740.2009.00007.x.
- ↑ "Questions and Answers about Shoulder Problems". Retrieved 2008-01-28.
- ↑ Adam, Rocchi (10 May 2016). "Frozen Shoulder – What, Where, Why and How To Get Relief". Spine Scan. Spine Scan. Retrieved 28 July 2016.
This article contains text from the public domain document "Frozen Shoulder", American Academy of Orthopaedic Surgeons.
Further reading
- Siegel, Lori B.; Cohen, Norman J.; Gall, Eric P. (1999). "Adhesive capsulitis: a sticky issue". American Family Physician. 59 (7): 1843–52. PMID 10208704.
- Radiology image sequence demonstrating CT guided shoulder hydrodilatation
- "Adhesive Capsulitis" from Arend CF. Ultrasound of the Shoulder. Master Medical Books, 2013.
- A "Neuromanual" treatment for frozen shoulder using local anesthetic from the Russian Journal of Manual Therapy, 2012
External links
| Classification | |
|---|---|
| External resources |