Knee pain
| Knee pain | |
|---|---|
 | |
| Human knee | |
| Classification and external resources | |
| MedlinePlus | 003187 |
Knee pain is pain in or around the knee.
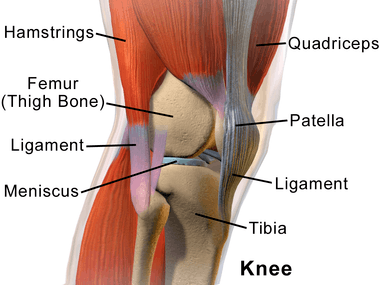
The knee joint consists of an articulation between four bones: the femur, tibia, fibula and patella. There are four compartments to the knee. These are the medial and lateral tibiofemoral compartments, the patellofemoral compartment and the superior tibiofibular joint. The components of each of these compartments can suffer from repetitive strain, injury or disease.
Running long distance can cause pain to the knee joint, as it is high-impact exercise.
Causes
Injuries
Some common injuries include:
- Sprain (Ligament sprain)
- Tear of meniscus[1]
- Strain (Muscle strain)
- Quadriceps muscles
- Hamstring muscles
- Popliteal muscle
- Patellar tendon
- Hamstring tendon
- Popliteal tendon
- Hemarthrosis – Hemarthrosis tends to develop over a relatively short period after injury, from several minutes to a few hours.[2]
Fractures
Diseases
Some of the diseases of cause of knee pain include the following:
- Knee osteoarthritis[1]
- Chondromalacia patella
- Baker's cyst
- Meniscal cyst
- Discoid meniscus
- Osgood-Schlatter disease[1]
- Larsen-Johansson disease[1]
- Knee rheumatoid arthritis[1]
- Osteochondritis dissecans disease
- Synovial chondromatosis disease
- Tumors
- Ankylosing spondylitis
- Reactive arthritis
- Tuberculosis arthritis
- Septic arthritis (Pyogenic arthritis)
- Osteomyelitis
- Hemophilic arthritis
- Gout (Gouty arthritis)
- Neuroma[1]
Inflammations
- Bursitis of the knee
- Prepatellar bursitis - Housemaid's knee (most common)
- Infrapatellar bursitis - Clergyman's knee (Superficial infrapatellar bursitis and Deep infrapatellar bursitis)
- Semimembranosus bursitis
- Tendinitis[1]
- Patellar tendinitis (Jumper's knee)
- Hamstring tendinitis
- Popliteal tendinitis
- Synovitis of the knee
Deformities
Common deformities of the knee include:
- Bipartite patella (two-part kneecap)
- Genu varum (bow legs)
- Genu valgum (knock-knees)
- Genu recurvatum (Knee hyperextension)
- Knee flexion deformity
Syndromes
Dislocations
- Patella dislocation
- Knee joint dislocation (Tibiofemoral joint dislocation)
Cold-induced
A Chinese study concluded that knee pain is significantly more prevalent in people working in cold stores than in those in normal temperature.[3]
One study came to the conclusion that 17% of adolescents with anterior knee pain (a common but benign self-limiting condition) report that their pain is associated with cold weather.[4] The same study indicated that the main activities associated with anterior knee pain are sporting, stair climbing and walking, but also sitting.[4] Some people with anterior knee pain tend to have generally colder knees, and such people also trend towards having to wear extra tights/long johns in the winter.[5]
Cold-induced knee pain may also be due to tenosynovitis of the tendons around the knee, in which cold exposure has a specific role, either as a causative or a contributing factor.[3] Frank arthritis has been reported in children due to frostbite from extreme cold causing direct chondrocyte injury.[6]
There is also a hereditary disease, familial cold autoinflammatory syndrome (FCAS), which often features knee pain, in addition to hives, fever and pain in other joints, following general exposure to cold.[7]
Cold weather also aggravates knee pain in patients already having osteoarthritis, rheumatoid arthritis and fibromyalgia.[8]
Knee pain due to less physical movement
A lower level of physical activity and a work environment where one is required to sit in a chair during the work day is one reason for developing knee joint pain, as the lower degree of physical movement tends to weaken the knee muscles. Blood vessels also can be affected, leading to development of painful conditions.
As age progresses the movement of the knee joint involves higher friction with adjacent tissue and cartilages.
Other causes
- Ligamentous laxity
- Fat pad impingement
- Knee effusion
- Deep vein thrombosis
- Peripheral vascular disease
- Exostosis
Referred knee pain
Referred pain is that pain perceived at a site different from its point of origin but innervated by the same spinal segment.[9] Sometimes knee pain may be related to another area from body. For example, knee pain can come from ankle, foot, hip joints or lumbar spine.
Diagnosis
Knee MRIs should be avoided for knee pain without symptoms or effusion, unless there are non-successful results from a functional rehabilitation program.[10]
In some diagnosis, such as in knee osteoarthritis, magnetic resonance imaging does not prove to be clear for its determination [11]
Management
Although surgery has a role in repairing traumatic injuries and broken bones, surgeries such as arthroscopic lavage do not provide significant or lasting improvements to either pain or function to people with degenerative knee pain, and therefore should almost never be performed.[12] Degenerative knee pain is pain caused by wear and tear, such as osteoarthritis or a meniscal tear. Effective treatments for degenerative knee pain include physical therapy exercises, pain-reducing drugs such as ibuprofen, knee replacement surgery, and weight loss in people who are overweight.[12]
Epidemiology
About 25% of people over the age of 50 experience knee pain from degenerative knee diseases.[12]
Society
In the United States, more than US $3 billion is spent each year on arthroscopic knee surgeries that are known to be ineffective in people with degenerative knee pain.[12]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 van der Heijden, RA; Lankhorst, NE; van Linschoten, R; Bierma-Zeinstra, SM; van Middelkoop, M (20 January 2015). "Exercise for treating patellofemoral pain syndrome". The Cochrane Database of Systematic Reviews. 1: CD010387. doi:10.1002/14651858.CD010387.pub2. PMID 25603546.
- ↑ Darlene Hertling and Randolph M.Kessler. Management of Common Musculoskeletal Disorders. Third Edition. ISBN 0-397-55150-9
- 1 2 Pienimäki, T (2002). "Cold exposure and musculoskeletal disorders and diseases. A review". International journal of circumpolar health. 61 (2): 173–82. doi:10.3402/ijch.v61i2.17450. PMID 12078965.
- 1 2 Sandow, MJ; Goodfellow, JW (1985). "The natural history of anterior knee pain in adolescents". The Journal of Bone and Joint Surgery. British Volume. 67 (1): 36–8. PMID 3968140.
- ↑ Selfe, J.; Sutton, C.; Hardaker, N. J.; Greenhalgh, S.; Karki, A.; Dey, P. (2010). "Anterior knee pain and cold knees: A possible association in women". The Knee. 17 (5): 319–323. doi:10.1016/j.knee.2009.10.005. PMID 19884010.
- ↑ Carrera, G. F.; Kozin, F.; McCarty, D. J. (1979). "Arthritis after frostbite injury in children". Arthritis & Rheumatism. 22 (10): 1082. doi:10.1002/art.1780221006.
- ↑ clinicaltrials.gov > Pathogenesis of Physical Induced Urticarial Syndromes National Institutes of Health Clinical Center (CC), December 2010
- ↑ Arthritis Special Report - Does Weather Affect Arthritis Pain? From Johns Hopkins Health Alerts, Johns Hopkins Hospital
- ↑ Carol Mattson Porth. Pathophysiology:concepts of altered health states. Publisher:Lippincott. Third Edition. Page 853. ISBN 0-397-54723-4
- ↑ American Medical Society for Sports Medicine (24 April 2014), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American Medical Society for Sports Medicine, retrieved 29 July 2014
- Dixit, S; DiFiori, JP; Burton, M; Mines, B (Jan 15, 2007). "Management of patellofemoral pain syndrome". American Family Physician. 75 (2): 194–202. PMID 17263214.
- Atanda A, Jr; Ruiz, D; Dodson, CC; Frederick, RW (Feb 2012). "Approach to the active patient with chronic anterior knee pain". The Physician and Sportsmedicine. 40 (1): 41–50. doi:10.3810/psm.2012.02.1950. PMID 22508250.
- Pappas, E; Wong-Tom, WM (Mar 2012). "Prospective Predictors of Patellofemoral Pain Syndrome: A Systematic Review With Meta-analysis". Sports health. 4 (2): 115–20. doi:10.1177/1941738111432097. PMC 3435911. PMID 23016077.
- Rixe, JA; Glick, JE; Brady, J; Olympia, RP (Sep 2013). "A review of the management of patellofemoral pain syndrome". The Physician and Sportsmedicine. 41 (3): 19–28. doi:10.3810/psm.2013.09.2023. PMID 24113699.
- Roush, MB; Sevier, TL; Wilson, JK; Jenkinson, DM; Helfst, RH; Gehlsen, GM; Basey, AL (Jan 2000). "Anterior knee pain: a clinical comparison of rehabilitation methods". Clinical Journal of Sport Medicine. 10 (1): 22–8. doi:10.1097/00042752-200001000-00005. PMID 10695846.
- ↑ Culvenor AG, Øiestad BE, Hart HF, Stefanik JJ, Guermazi A, Crossley KM (2018). ""Prevalence of knee osteoarthritis features on magnetic resonance imaging in asymptomatic uninjured adults: a systematic review and meta- analysis"". PBritish Journal of Sports Medicine. doi:10.1136/bjsports-2018-099257.
- 1 2 3 4 Siemieniuk RA, Harris IA, Agoritsas T, Poolman RW, Brignardello-Petersen R, Van de Velde S, Buchbinder R, Englund M, Lytvyn L, Quinlan C, Helsingen L, Knutsen G, Olsen NR, Macdonald H, Hailey L, Wilson HM, Lydiatt A, Kristiansen A (2017). "Arthroscopic surgery for degenerative knee arthritis and meniscal tears: a clinical practice guideline". BMJ. 357: j1982. doi:10.1136/bmj.j1982. PMC 5426368. PMID 28490431.
External links
- What I Wish I'd Known About My Knees about ineffective treatments by health writer Jane Brody