Hematuria
| Hematuria | |
|---|---|
| Synonyms | Haematuria |
|
| |
| Microscopic hematuria | |
| Specialty | Nephrology, urology |
| Differential diagnosis | Kidney stone disease, UTI, cancer, exercise induced hematuria |
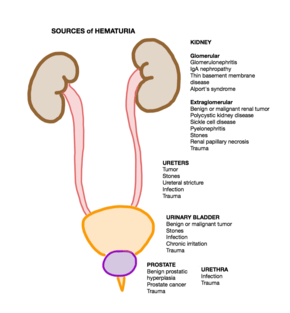
Hematuria is the presence of red blood cells in the urine. Visible hematuria, also known as gross hematuria, is easily identified, as it causes red or brown discoloration of the urine. Microscopic hematuria is invisible to the naked eye and is often found by urinalysis or urine dipstick. Any part of the kidneys or urinary tract (ureters, urinary bladder, prostate, and urethra) can leak blood into the urine. The causes of hematuria are broad, ranging from urinary tract infection to kidney stones to bladder cancer.[1]
Microscopic hematuria is found regularly on routine urinalysis, with a prevalence between 0.18% and 37%.[2] Some studies have shown increased incidence with age and female sex, but others did not show a correlation.[1] In many people, no specific cause is found.[3] Cancer of the kidney, prostate, bladder, or testes is found in 5% of people with microscopic hematuria and up to 40% of those with visible hematuria.[3] Hematuria is common in pediatric populations, with a prevalence of 0.5-2%.[4]
Certain substances can mimic hematuria either by discoloring the urine or by causing a false positive on urine dipstick. Causes of a false positive urine dipstick include hemoglobin (in absence of red blood cells), semen, myoglobin, porphyrins, betanin (after eating beets), and drugs (such as rifampicin, phenazopyridine, and sulphonamides).[4] Substances that mimic hematuria by causing red or brown discoloration of the urine include drugs (such as sulfonamides, quinine, rifampin, phenytoin),[5] betanin, and menses.
Causes
Visible blood

Visible or gross hematuria causes brown or red discoloration of the urine that is visible to the naked eye. It can be painful or painless.
Painful
- Kidney stones–suspected in a person with unilateral sharp flank pain that radiates to the groin, burning on urination, and fever[6][7]
- Infection of the lower urinary tract or bladder–causes visible hematuria, white blood cells in the urine, and lower abdominal pain[6]
- Pyelonephritis, infection of the kidneys–causes fever, white blood cells in the urine, and flank pain[6]
- Polycystic kidney disease–a genetic disorder that causes cysts in the kidney[8]
- Renal vein thrombosis
- Trauma–including blunt trauma to the urinary tract or traumatic foley catheter placement[8]
Painless
The most worrisome cause of painless, visible blood in the urine is kidney or bladder cancer, especially in a person with risk factors such as male sex, age over 35, history of smoking, chronic bladder inflammation, and occupational exposures (to aromatic amines and aniline dyes)[9][10] Between 80-90% of people with bladder cancer initially presented with visible blood in the urine.[7]
Other causes include
- Exercise-induced hematuria occurs in up to 30% of long distance runners and often resolves a few days after stopping running.[11]
Children
More than 50% of visible hematuria in children have an identifiable cause. Common causes of visible hematuria in children are:[12]
- urinary tract infection
- perineal or urethral irritation
- congenital abnormalities–
- Non-vascular—ureteropelvic junction obstruction, posterior urethral valves, urethral prolapse, urethral diverticula, multicystic dysplastic kidney
- Vascular—arteriovenous malformations, hereditary hemorrhagic telangiectasias, renal vascular thromboses
- trauma
- acute nephritis—characterized by visible hematuria, white blood cells in the urine, and a transient decline in renal function, commonly caused by medications
- coagulopathy
- kidney stones
- IgA nephropathy–suspected in a child with dark urine and recent upper respiratory infection[4]
- Post-streptococcal glomerulonephritis–suspected in a child with dark brown urine following recent streptoccocal pharyngitis or impetigo[11]
Non visible blood
Microscopic hematuria does not discolor the urine and is thus found incidentally on urinalysis or light microscopy. It is defined as greater than three red blood cells per high powered field. In many of these cases, no source or cause is found.[3] Any part of the kidneys or urinary system can cause microscopic hematuria. Causes can be separated into glomerular, arising from the filtering system of the kidney, and non-glomerular, arising from the kidney (outside the glomerulus), ureters, urinary bladder, prostate, or urethra.[1]
Glomerular
Inflammation of or injury to the glomeruli can cause leakage of red blood cells, resulting in misshapen cells and red blood cell casts in the urine.[6] Glomerular bleeding is frequently accompanied by proteinuria, or leakage of protein into the urine.
Common causes include
- IgA nephropathy[1]
- Hereditary nephritis (Alport's disease)[1]
- Benign familial hematuria[1]
- Glomerulonephritis–a group of inflammatory diseases of the glomeruli, leading to hematuria, hypertension, and peripheral edema[6]
Non-glomerular
- The three most common causes of microscopic hematuria are[3]
- urinary tract infection–infection of the ureters, bladder, prostate or urethra; signs include cloudy urine, urinary frequency, lower abdominal pain, and pain or burning on urination
- benign prostatic hyperplasia–signs include urinary frequency, nocturia, and an enlarged prostate on digital rectal examination
- urinary tract stones–causes pain and burning on urination, unilateral flank pain, and fever[7]
- Less common causes include[1]
- bladder or ureteral polyps
- medullary sponge kidney
- hypercalciuria or hyperuricosuria
- vigorous exercise
- cancer or tumor of the bladder or prostate
- polycystic kidney disease
- renal papillary necrosis
- sickle cell disease or trait
Children
In many cases of asymptomatic microscopic hematuria without proteinuria, no etiology is found. Common causes of microscopic hematuria in pediatric populations include:[12]
- hypercalciuria–suspected in a child with family history of kidney stones; can be asymptomatic or can cause painful urination
- benign familial hematuria–a genetic disorder causing persistent microscopic hematuria
- IgA nephropathy
- sickle cell trait or disease
- Alport syndrome–a genetic disorder causing recurrent microscopic hematuria with proteinuria, hearing loss, and progressive kidney failure
Diagnosis
Sometimes the cause of hematuria can be determined based on the medical history and urine testing. This is especially true for people ages less than 35, in whom the risk of cancer is low. It is imperative to ascertain key risk factors such as smoking, occupational exposures to benzene, history of recent weight loss and/or history of urologic disorders such as benign enlargement of the prostate or recurrent kidney stones to help with risk stratification.[13] The two most common causes of hematuria are related to kidney stones causing obstruction or infection of the prostate or bladder.[3] Additionally, athletes with vigorous exercise regimens may sometimes have either visible or microscopic hematuria.[14]
The first step in evaluation of Hematuria is to perform a urine dipstick to assess for blood in the urine, followed by a urinalysis with microscopic evaluation for confirmation.[15] If hematuria is present, and is associated with acute onset of unilateral flank pain, it is generally indicative of a presence of a kidney stone and evaluation should be done with a non-contrast CT scan of the abdomen/pelvis. If hematuria is associated fever, pain with urination, urinary frequency or presence of white blood cells in the urine; it is highly suggestive of a urinary tract infection and additional work-up with urine cultures should be done to further evaluate. If neither of these features are present, the next step is to separate the evaluation into visible vs microscopic hematuria.
Visible
For people with visible hematuria and evidence of blood clots, further imaging with an abdominal CT scan should be done and an urgent referral to a urologist made. Otherwise, the next step involves determining if source of bleeding is glomerular in nature as evidenced by presence of inappropriately shaped/dysmorphic red blood cells, presence of protein in the urine, new or worsening hypertension or swelling. If source is glomerular patients should be referred to a nephrologist for further evaluation. Non-glomerular source of bleeding will usually require further work-up by a urologist.
Microscopic
In people with microscopic hematuria, it is important to rule out any possible confounders such as menstruation in women, possible presence of semen in sample or recent rigorous exercise. In menstruating women, tests should be repeated during non-bleeding parts of their cycles. In individuals with history of recent rigorous exercise, urinalysis should be repeated 4–6 weeks following cessation of exercise. All women of child-bearing age should undergo a pregnancy test, and if positive should receive an ultrasound of their kidneys and bladder with further invasive diagnostic work-up deferred until completion of pregnancy.[16]
If diagnostic work-up has been unyielding so far or the aforementioned risk factors are present, it is important to begin a thorough work-up for possible malignancy especially of the bladder and kidney by referring to a Urologist to look at the urethra and bladder with a cystoscopy and also performing additional imaging using CT urography, which provides a thorough view of the complete urinary system.
For individuals with persistent hematuria with no immediate identifiable cause, urinalysis should be repeated once a year, and if it is negative for 2 years then you can stop repeating the tests. However, if it is positive for 3 years, repeat anatomic evaluation should be done.[17]
Management
Management of hematuria is aimed at treating secondary causes of hematuria. If hematuria is a result of a UTI, treatment with antibiotics is usually initiated and urine testing repeated after 6 weeks.[18] If hematuria is secondary to a kidney stone, then management depends on the size of the kidney stone. If the stone is small enough, usually less than 1 cm, then conservative management with analgesics and fluid hydration may be sufficient, however stones that are too big may require removal by a urologist.[19] Another common cause of hematuria is benign enlargement of the prostate (BPH), treatment is aimed at reducing the size of the prostate with medications like finasteride and symptomatic management with drugs like terazonsin or tamsulosin.[20]
For people with exercise induced hematuria, management is conservative and involves cessation of strenuous activities and keeping hydrated.[14] If the cause of hematuria is a result of malignancy, treatment and management depends on the type and stage of cancer and can involve chemotherapy, radiation or surgical resection of the tumor or organ involved.[21][22]
References
- 1 2 3 4 5 6 7 Cohen, Robert A.; Brown, Robert S. (2003-06-05). "Clinical practice. Microscopic hematuria". The New England Journal of Medicine. 348 (23): 2330–2338. doi:10.1056/NEJMcp012694. ISSN 1533-4406. PMID 12788998.
- ↑ Shinagare, Atul B.; Silverman, Stuart G.; Gershanik, Esteban F.; Chang, Steven L.; Khorasani, Ramin. "Evaluating Hematuria: Impact of Guideline Adherence on Urologic Cancer Diagnosis". The American Journal of Medicine. 127 (7): 625–632. doi:10.1016/j.amjmed.2014.02.013. Archived from the original on 2018-05-03.
- 1 2 3 4 5 Sharp, Victoria (December 1, 2013). "Assessment of Asymptomatic Microscopic Hematuria in Adults". American Family Physician. 88 (11): 747–54.
- 1 2 3 Shah, Samir (2014). Step-up to pediatrics. Ronan, Jeanine C.,, Alverson, Brian, (First ed.). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins. pp. 175–176. ISBN 9781451145809. OCLC 855779297.
- ↑ Hematuria Causes Archived 2011-05-13 at the Wayback Machine. Original Date of Publication: 15 Jun 1998. Reviewed by: Stacy J. Childs, M.D., Stanley J. Swierzewski, III, M.D. Last Reviewed: 10 Jul 2008
- 1 2 3 4 5 S.,, Lipsky, Martin. Blueprints family medicine. King, Mitchell S., (Third ed.). Philadelphia, PA. pp. 65–66. ISBN 9781608310876. OCLC 502392894.
- 1 2 3 "Diagnosis and Management of Hematuria". Surgical Clinics of North America. 96 (3): 503–515. 2016-06-01. doi:10.1016/j.suc.2016.02.007. ISSN 0039-6109.
- 1 2 Agabegi, Steven (2013). Step-up to medicine. Agabegi, Elizabeth D., Ring, Adam C. (3rd ed.). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins. pp. 281–282. ISBN 9781609133603. OCLC 794228016.
- ↑ Davis, Rodney; Jones, J. Stephen; Barocas, Daniel A.; Castle, Erik P.; Lang, Erich K.; Leveillee, Raymond J.; Messing, Edward M.; Miller, Scott D.; Peterson, Andrew C. "Diagnosis, Evaluation and Follow-Up of Asymptomatic Microhematuria (AMH) in Adults: AUA Guideline". The Journal of Urology. 188 (6): 2473–2481. doi:10.1016/j.juro.2012.09.078.
- ↑ Step-up to medicine. Agabegi, Steven S., Agabegi, Elizabeth D., Ring, Adam C. (3rd ed.). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins. 2013. ISBN 9781609133603. OCLC 794228016.
- 1 2 "Work-up of Hematuria". Primary Care: Clinics in Office Practice. 41 (4): 737–748. 2014-12-01. doi:10.1016/j.pop.2014.08.007. ISSN 0095-4543.
- 1 2 Pade, Kathryn H.; Liu, Deborah R. (September 2014). "An evidence-based approach to the management of hematuria in children in the emergency department". Pediatric Emergency Medicine Practice. 11 (9): 1–13, quiz 14. ISSN 1549-9650. PMID 25296518.
- ↑ Diagnosis, evaluation, and follow-up of asymptomatic microhematuria (AMH) in adults: American Urological Association (AUA) Guideline "Archived copy" (PDF). Archived from the original (PDF) on 2012-12-24. Retrieved 2012-10-27.
- 1 2 Jones, G. R.; Newhouse, I. (April 1997). "Sport-related hematuria: a review". Clinical Journal of Sport Medicine. 7 (2): 119–125. ISSN 1050-642X. PMID 9113428. Archived from the original on 2017-12-15.
- ↑ MD, Scott Moses,. "Hematuria in Adults". www.fpnotebook.com. Archived from the original on 15 December 2017. Retrieved 3 May 2018.
- ↑ "Etiology and evaluation of hematuria in adults". www.uptodate.com. Archived from the original on 2017-12-15. Retrieved 2017-12-15.
- ↑ Grossfeld, G. D.; Wolf, J. S.; Litwan, M. S.; Hricak, H.; Shuler, C. L.; Agerter, D. C.; Carroll, P. R. (2001-03-15). "Asymptomatic microscopic hematuria in adults: summary of the AUA best practice policy recommendations". American Family Physician. 63 (6): 1145–1154. ISSN 0002-838X. PMID 11277551. Archived from the original on 2017-12-15.
- ↑ Hooton, T. M.; Stamm, W. E. (September 1997). "Diagnosis and treatment of uncomplicated urinary tract infection". Infectious Disease Clinics of North America. 11 (3): 551–581. ISSN 0891-5520. PMID 9378923. Archived from the original on 2018-01-26.
- ↑ Coe, F. L.; Parks, J. H.; Asplin, J. R. (1992-10-15). "The pathogenesis and treatment of kidney stones". The New England Journal of Medicine. 327 (16): 1141–1152. doi:10.1056/NEJM199210153271607. ISSN 0028-4793. PMID 1528210. Archived from the original on 2017-12-15.
- ↑ McVary, Kevin T.; Roehrborn, Claus G.; Avins, Andrew L.; Barry, Michael J.; Bruskewitz, Reginald C.; Donnell, Robert F.; Foster, Harris E.; Gonzalez, Chris M.; Kaplan, Steven A. (May 2011). "Update on AUA guideline on the management of benign prostatic hyperplasia". The Journal of Urology. 185 (5): 1793–1803. doi:10.1016/j.juro.2011.01.074. ISSN 1527-3792. PMID 21420124. Archived from the original on 2017-12-16.
- ↑ Rini, Brian I.; McDermott, David F.; Hammers, Hans; Bro, William; Bukowski, Ronald M.; Faba, Bernard; Faba, Jo; Figlin, Robert A.; Hutson, Thomas (2016). "Society for Immunotherapy of Cancer consensus statement on immunotherapy for the treatment of renal cell carcinoma". Journal for Immunotherapy of Cancer. 4: 81. doi:10.1186/s40425-016-0180-7. ISSN 2051-1426. PMC 5109802. PMID 27891227. Archived from the original on 2018-01-26.
- ↑ Hall, M. Craig; Chang, Sam S.; Dalbagni, Guido; Pruthi, Raj Som; Seigne, John Derek; Skinner, Eila Curlee; Wolf, J. Stuart; Schellhammer, Paul F. (December 2007). "Guideline for the management of nonmuscle invasive bladder cancer (stages Ta, T1, and Tis): 2007 update". The Journal of Urology. 178 (6): 2314–2330. doi:10.1016/j.juro.2007.09.003. ISSN 1527-3792. PMID 17993339. Archived from the original on 2018-01-26.
External links
| Classification | |
|---|---|
| External resources |
![]()