Bladder cancer
| Bladder cancer | |
|---|---|
 | |
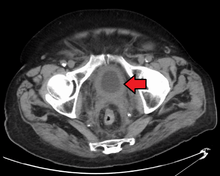
| Transitional cell carcinoma of the bladder. The white in the bladder is contrast. | |
| Specialty | Oncology |
| Symptoms | Blood in the urine, pain with urination[1] |
| Usual onset | 65 to 85 years old[2] |
| Types | Transitional cell carcinoma, squamous cell carcinoma, adenocarcinoma[3] |
| Risk factors | Smoking, family history, prior radiation therapy, frequent bladder infections, certain chemicals[1] |
| Diagnostic method | Cystoscopy with tissue biopsies[4] |
| Treatment | Surgery, radiation therapy, chemotherapy, immunotherapy[1] |
| Prognosis | Five-year survival rates ~77% (US)[2] |
| Frequency | 3.4 million current cases (2015)[5] |
| Deaths | 188,000 per year[6] |
Bladder cancer is any of several types of cancer arising from the tissues of the urinary bladder.[1] It is a disease in which cells grow abnormally and have the potential to spread to other parts of the body.[7][8] Symptoms include blood in the urine, pain with urination, and low back pain.[1]
Risk factors for bladder cancer include smoking, family history, prior radiation therapy, frequent bladder infections, and exposure to certain chemicals.[1] The most common type is transitional cell carcinoma.[3] Other types include squamous cell carcinoma and adenocarcinoma.[3] Diagnosis is typically by cystoscopy with tissue biopsies.[4] Staging of the cancer is typically determined by medical imaging such as CT scan and bone scan.[1]
Treatment depends on the stage of the cancer.[1] It may include some combination of surgery, radiation therapy, chemotherapy, or immunotherapy.[1] Surgical options may include transurethral resection, partial or complete removal of the bladder, or urinary diversion.[1] Typical five-year survival rates in the United States are 77%.[2]
Bladder cancer, as of 2015, affects about 3.4 million people globally with 430,000 new cases a year.[5][9] In 2015 it resulted in 188,000 deaths.[6] Age of onset is most often between 65 and 85 years of age.[2] Males are more often affected than females.[2] In the United States in 2018 81,000 cases and 17,000 deaths are expected making it the 6th most common type of cancer in the region.[2]
Signs and symptoms
Bladder cancer characteristically causes blood in the urine (hematuria), which may be visible (gross/macroscopic hematuria) or detectable only by microscope (microscopic hematuria). Blood in the urine is the most common symptom in bladder cancer, and is painless. Visible blood in the urine may be of only short duration, and a urine test may be required to confirm non visible blood. Between 80-90% of people with bladder cancer initially presented with visible blood.[10] Blood in the urine may also be caused by other conditions, such as bladder or ureteric stones, infection, kidney disease, kidney cancers or vascular malformations, though these conditions (except kidney cancers) would typically be painful.
Other possible symptoms include pain during urination (dysuria), frequent urination, or feeling the need to urinate without being able to do so. These signs and symptoms are not specific to bladder cancer, and may also be caused by non-cancerous conditions, including prostate infections, overactive bladder or cystitis.
Patients with advanced disease refer pelvic or bony pain, lower-extremity swelling, or flank pain. Rarely, a palpable mass can be detected on physical examination.
Causes
Tobacco smoking is the main known contributor to urinary bladder cancer; in most populations, smoking is associated with over half of bladder cancer cases in men and one-third of cases among women,[11] however these proportions have reduced over recent years since there are fewer smokers in Europe and North America.[12] There is an almost linear relationship between smoking duration (in years), pack years and bladder cancer risk. A risk plateau at smoking about 15 cigarettes a day can be observed (meaning that those who smoke 15 cigarettes a day are approximately at the same risk as those smoking 30 cigarettes a day). Quitting smoking reduces the risk, however former smokers will most likely always be at a higher risk of bladder cancer compared to never smokers.[12] Passive smoking does not appear to be a risk.[13]
Thirty percent of bladder tumors probably result from occupational exposure in the workplace to carcinogens such as benzidine. 2-Naphthylamine, which is found in cigarette smoke, has also been shown to increase bladder cancer risk. Occupations at risk are bus drivers, rubber workers, motor mechanics, leather (including shoe) workers, blacksmiths, machine setters, and mechanics.[14] Hairdressers are thought to be at risk as well because of their frequent exposure to permanent hair dyes.
In addition to these major risk factors there are also numerous other modifiable factors that are less strongly (i.e. 10–20% risk increase) associated with bladder cancer, for example, obesity.[15] Although these could be considered as minor effects, risk reduction in the general population could still be achieved by reducing the prevalence of a number of smaller risk factor together.[16]
It has been suggested that mutations at HRAS, KRAS2, RB1, and FGFR3 may be associated in some cases.[17]
Diagnosis

Currently, the best diagnosis of the state of the bladder is by way of cystoscopy, which is a procedure in which a flexible tube bearing a camera and various instruments is introduced into the bladder through the urethra. The procedure allows for a visual inspection of the bladder, for minor remedial work to be undertaken and for samples of suspicious lesions to be taken for a biopsy.
Urine cytology can be obtained in voided urine or at the time of the cystoscopy ("bladder washing"). Cytology is not very sensitive (a negative result cannot reliably exclude bladder cancer).[18] There are newer non-invasive urine bound markers available as aids in the diagnosis of bladder cancer, including human complement factor H-related protein, high-molecular-weight carcinoembryonic antigen, and nuclear matrix protein 22 (NMP22).[19] NMP22 is also available as a prescription home test. Other non-invasive urine based tests include the CertNDx Bladder Cancer Assay, which combines FGFR3 mutation detection with protein and DNA methylation markers to detect cancers across stage and grade, UroVysion, and Cxbladder.
The diagnosis of bladder cancer can also be done with a Hexvix/Cysview guided fluorescence cystoscopy (blue light cystoscopy, Photodynamic diagnosis), as an adjunct to conventional white-light cystoscopy. This procedure improves the detection of bladder cancer and reduces the rate of early tumor recurrence, compared with white light cystoscopy alone. Cysview cystoscopy detects more cancer and reduces recurrence. Cysview is marketed in Europe under the brand name Hexvix.[20][21][22][23]
However, visual detection in any form listed above, is not sufficient for establishing pathological classification, cell type or the stage of the present tumor. A so-called cold cup biopsy during an ordinary cystoscopy (rigid or flexible) will not be sufficient for pathological staging either. Hence, a visual detection needs to be followed by transurethral surgery. The procedure is called transurethral resection of bladder tumor (TURBT). Further, bimanual examination should be carried out before and after the TURBT to assess whether there is a palpable mass or if the tumour is fixed ("tethered") to the pelvic wall. The pathological classification obtained by the TURBT-procedure, is of fundamental importance for making the appropriate choice of ensuing treatment and/or follow-up routines.[24]
Pathological classification
95% of bladder cancers are transitional cell carcinoma. The other 5% are squamous cell carcinoma, adenocarcinoma, sarcoma, small cell carcinoma, and secondary deposits from cancers elsewhere in the body.[25]
Carcinoma in situ (CIS) invariably consists of cytologically high-grade tumour cells.
Staging
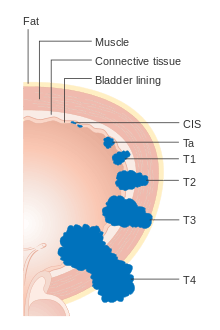
Bladder cancer is staged (classified by the extent of spread of the cancer) and graded (how abnormal and aggressive the cells appear under the microscope) to determine treatments and estimate outcomes.
In the TNM staging system for bladder cancer, the following apply:[26]
T (Primary tumour)
- TX Primary tumour cannot be assessed
- T0 No evidence of primary tumour
- Ta Non-invasive papillary carcinoma
- Tis Carcinoma in situ ('flat tumour')
- T1 Tumour invades subepithelial connective tissue
- T2a Tumour invades superficial muscle (inner half)
- T2b Tumour invades deep muscle (outer half)
- T3 Tumour invades perivesical tissue:
- T3a Microscopically
- T3b Macroscopically (extravesical mass)
- T4a Tumour invades prostate, uterus or vagina
- T4b Tumour invades pelvic wall or abdominal wall
N (Lymph nodes)
- NX Regional lymph nodes cannot be assessed
- N0 No regional lymph node metastasis
- N1 Metastasis in a single lymph node 2 cm or less in greatest dimension
- N2 Metastasis in a single lymph node more than 2 cm but not more than 5 cm in greatest dimension, or multiple lymph nodes, none more than 5 cm in greatest dimension
- N3 Metastasis in a lymph node more than 5 cm in greatest dimension
M (Distant metastasis)
- MX Distant metastasis cannot be assessed
- M0 No distant metastasis
- M1 Distant metastasis.
| Stage | % |
|---|---|
| 0 | 98% |
| I | 88% |
| II | 63% |
| III | 46% |
| IV | 15% |
Numerical
The stages above can be integrated into a numerical staging (with Roman numerals) as follows:[28]
- Stage 0a: Ta, N0, M0
- Stage 0is: Tis, N0, M0
- Stage I: T1, N0, M0
- Stage II: T2a or T2b, N0, M0
- Stage III: T3a, T3b, or T4a, N0, M0
- Stage IV; any of the following:
- T4b, N0, M0
- any T, N1 to N3, M0
- any T, any N, M1
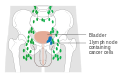 Stage N1 bladder cancer
Stage N1 bladder cancer Advanced bladder cancer
Advanced bladder cancer
Screening
As of 2010 there is insufficient evidence to determine if screening for bladder cancer in people without symptoms is effective or not.[29]
In 2013 a preliminary, small study of 98 samples of urine, all from men—24 who had cancer, and 74 with bladder-related problems but no cancer yet used a gas chromatograph to successfully examine the vapor from heated urine samples to identify cancer.[30]
Prevention
A 2008 study commissioned by the World Health Organisation concluded that "specific fruit and vegetables may act to reduce the risk of bladder cancer."[31] Fruit and yellow-orange vegetables, particularly carrots and those containing selenium,[32] are probably associated with a moderately reduced risk of bladder cancer. Citrus fruits and cruciferous vegetables were also identified as having a possibly protective effect. However an analysis of 47,909 men in the Health Professionals Follow-Up Study showed little correlation between cancer reduction and high consumption of fruits and vegetables overall, or yellow or green leafy vegetables specifically, compared to the statistically significant reduction among those men who consumed large amounts of cruciferous vegetables.
In a 10-year study involving almost 49,000 men, researchers found that men who drank at least 1,44 L of water (around 6 cups) per day had a significantly reduced incidence of bladder cancer when compared with men who drank less. It was also found that: "the risk of bladder cancer decreased by 7% for every 240 mL of fluid added".[33] The authors proposed that bladder cancer might partly be caused by the bladder directly contacting carcinogens that are excreted in urine, although this has not yet been confirmed in other studies.[31]
Treatment


The treatment of bladder cancer depends on how deeply the tumor invades into the bladder wall.
Superficial tumors
Superficial tumors (those not entering the muscle layer) can be "shaved off" using an electrocautery device attached to a cystoscope, which in that case is called a resectoscope. The procedure is called transurethral resection of bladder tumor—TURBT—and serves primarily for pathological staging. In case of non-muscle invasive bladder cancer the TURBT is in itself the treatment, but in case of muscle invasive cancer, the procedure is insufficient for final treatment.[24]
Immunotherapy by intravesicular delivery of Bacillus Calmette–Guérin (BCG) is also used to treat and prevent the recurrence of superficial tumors.[34] BCG is a vaccine against tuberculosis that is prepared from attenuated (weakened) live bovine tuberculosis bacillus, Mycobacterium bovis, that has lost its virulence in humans. BCG immunotherapy is effective in up to 2/3 of the cases at this stage, and in randomized trials has been shown to be superior to standard chemotherapy.[35] The mechanism by which BCG prevents recurrence is unknown, but the presence of bacteria in the bladder may trigger a localized immune reaction which clears residual cancer cells.[36]
Patients whose tumors recurred after treatment with BCG are more difficult to treat.[37] Many physicians recommend cystectomy for these patients. This recommendation is in accordance with the official guidelines of the European Association of Urologists (EAU)[38] and the American Urological Association (AUA)[39] However, many patients refuse to undergo this life changing operation, and prefer to try novel conservative treatment options before opting to this last radical resort. Device assisted chemotherapy is one such group of novel technologies used to treat superficial bladder cancer.[40] These technologies use different mechanisms to facilitate the absorption and action of a chemotherapy drug instilled directly into the bladder. Another technology - electromotive drug administration (EMDA) – uses an electric current to enhance drug absorption after surgical removal of the tumor.[41][42] Another technology, thermotherapy, uses radio-frequency energy to directly heat the bladder wall, which together with chemotherapy shows a synergistic effect, enhancing each other's capacity to kill tumor cells. This technology was studied by different investigators.[43][44][45][46]
Muscle invasive disease
Untreated, superficial tumors may gradually begin to infiltrate the muscular wall of the bladder. Tumors that infiltrate the bladder wall require more radical surgery, where part or all of the bladder is removed (a cystectomy) and the urinary stream is diverted into an isolated bowel loop (called an ileal conduit or urostomy). In some cases, skilled surgeons can create a substitute bladder (a neobladder) from a segment of intestinal tissue, but this largely depends upon patient preference, age of patient, renal function, and the site of the disease.
To treat an invasive tumor, a combination of radiation and chemotherapy in conjunction with transurethral (endoscopic) bladder tumor resection can be used. Review of available large data series on this so-called trimodality therapy has indicated similar long-term cancer specific survival rates, with improved overall quality of life as for patients undergoing radical cystectomy with urinary reconstruction. These patients are usually highly selected and do not have multi-focal disease or carcinoma in-situ, which is associated with a higher rate of recurrence, progression, and death from bladder cancer versus patients who undergo radical cystectomy.[47]
Photodynamic diagnosis may improve surgical outcome on bladder cancer.[48]
For muscle invasive urothelial urinary bladder cancer there are a number of treatment options. The best approach is radical cystectomy, as mentioned. In males, this usually includes also the removal of the prostate; and in females it involves removal of ovaries, uterus and parts of the vagina.
Micrometastatic disease
In order to address the problem of micrometastatic disease which in itself has implications on longtime survival, new treatment options are dearly needed. Micrometastatic dissemination is often not treatable with only major surgery and the concept of neoadjuvant chemotherapy has evolved. In this patients first receive chemotherapy in 3 or 4 cycles, and after that proceed to major surgery. In a number of meta-analyses of randomised prospective trials worldwide, the results have shown survival benefits between 5–8% with this therapy, in a follow up time of 5 years.[49][50][51][52]
 Drug treatment (chemotherapy) into the bladder
Drug treatment (chemotherapy) into the bladder Surgical reconstruction of the bladder following removal.
Surgical reconstruction of the bladder following removal.
Epidemiology

Worldwide
Globally, in 2010, bladder cancer resulted in 170,000 deaths up from 114,000 in 1990.[54] This is an increase of 19.4%, adjusted for increase in total world population.
US
In the United States, bladder cancer is the fourth most common type of cancer in men and the ninth most common cancer in women. More than 50,000 men and 16,000 women are diagnosed with bladder cancer each year. Smoking can only partially explain this higher incidence in men.[55] One other reason is that the androgen receptor, which is much more active in men than in women, plays a major part in the development of the cancer.[56]
UK
Bladder cancer is the seventh most common cancer in the UK (around 10,400 people were diagnosed with the disease in 2011), and it is the seventh most common cause of cancer death (around 5,200 people died in 2012).[57]
See also
References
- 1 2 3 4 5 6 7 8 9 10 "Bladder Cancer Treatment". National Cancer Institute. Archived from the original on 14 July 2017. Retrieved 18 July 2017.
- 1 2 3 4 5 6 "Cancer of the Urinary Bladder – Cancer Stat Facts". seer.cancer.gov. Archived from the original on 8 July 2017. Retrieved 18 July 2017.
- 1 2 3 "Bladder Cancer". National Cancer Institute. Archived from the original on 17 July 2017. Retrieved 18 July 2017.
- 1 2 "Bladder Cancer Treatment". National Cancer Institute. 5 June 2017. Archived from the original on 14 July 2017. Retrieved 18 July 2017.
- 1 2 GBD 2015 Disease and Injury Incidence and Prevalence, Collaborators. (8 October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- 1 2 GBD 2015 Mortality and Causes of Death, Collaborators. (8 October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ↑ "Cancer Fact sheet N°297". World Health Organization. February 2014. Archived from the original on 29 December 2010. Retrieved 10 June 2014.
- ↑ "Defining Cancer". National Cancer Institute. Archived from the original on 25 June 2014. Retrieved 10 June 2014.
- ↑ World Cancer Report 2014. World Health Organization. 2014. pp. Chapter 1.1. ISBN 9283204298.
- ↑ "Diagnosis and Management of Hematuria". Surgical Clinics of North America. 96 (3): 503–515. 2016-06-01. doi:10.1016/j.suc.2016.02.007. ISSN 0039-6109.
- ↑ Zeegers MP; Tan, FE; Dorant, E; Van Den Brandt, PA (2000). "The impact of characteristics of cigarette smoking on urinary tract cancer risk: a meta-analysis of epidemiologic studies". Cancer. 89 (3): 630–9. doi:10.1002/1097-0142(20000801)89:3<630::AID-CNCR19>3.0.CO;2-Q. PMID 10931463.
- 1 2 Osch, Frits H. M. van; Jochems, Sylvia H. J.; Schooten, Frederik-Jan van; Bryan, Richard T.; Zeegers, Maurice P. (2016-04-20). "Quantified relations between exposure to tobacco smoking and bladder cancer risk: a meta-analysis of 89 observational studies". International Journal of Epidemiology: dyw044. doi:10.1093/ije/dyw044. ISSN 0300-5771. PMID 27097748.
- ↑ Lee, PN; Thornton, AJ; Hamling, JS (October 2016). "Epidemiological evidence on environmental tobacco smoke and cancers other than lung or breast". Regulatory toxicology and pharmacology. 80: 134–63. doi:10.1016/j.yrtph.2016.06.012. PMID 27321059.
- ↑ Reulen RC, Zeegers MP (September 2008). "A meta-analysis on the association between bladder cancer and occupation". Scandinavian journal of urology and nephrology. Supplementum. 42 (218): 64–78. doi:10.1080/03008880802325192. PMID 18815919.
- ↑ Sun, Jiang-Wei; Zhao, Long-Gang; Yang, Yang; Ma, Xiao; Wang, Ying-Ying; Xiang, Yong-Bing (24 March 2015). "Obesity and Risk of Bladder Cancer: A Dose-Response Meta-Analysis of 15 Cohort Studies". PLOS ONE. 10 (3): e0119313. doi:10.1371/journal.pone.0119313. ISSN 1932-6203. PMC 4372289. PMID 25803438. Archived from the original on 5 March 2017.
- ↑ Al-Zalabani, AbdulmohsenH.; Stewart, KellyF.J.; Wesselius, Anke; Schols, AnnemieM.W.J.; Zeegers, MauriceP. (2016-03-21). "Modifiable risk factors for the prevention of bladder cancer: a systematic review of meta-analyses". European Journal of Epidemiology: 1–41. doi:10.1007/s10654-016-0138-6. ISSN 0393-2990. PMC 5010611.
- ↑ Online Mendelian Inheritance in Man (OMIM) 109800
- ↑ Lotan, Y.; Roehrborn, C. G. (2003). "Sensitivity and specificity of commonly available bladder tumor markers versus cytology: Results of a comprehensive literature review and meta-analyses". Urology. 61 (1): 109–118, discussion 118. doi:10.1016/S0090-4295(02)02136-2. PMID 12559279.
- ↑ Shariat; Karam, JA; Lotan, Y; Karakiewizc, PI; et al. (2008). "Critical Evaluation of Urinary Markers for Bladder Cancer Detection and Monitoring". Reviews in Urology. 10 (2): 120–135. PMC 2483317. PMID 18660854.
- ↑ "Hexvix". Archived from the original on 21 October 2013.
- ↑ "Photocure—Cysview Hexaminolevulinate (HCL)". Cysview.net. Archived from the original on 27 January 2013. Retrieved 10 January 2013.
- ↑ "Archived copy". Archived from the original on 31 March 2012. Retrieved 22 April 2011. Fluorescence-guided transurethral resection of bladder tumours reduces bladder tumour recurrence due to less residual tumour tissue in Ta/T1 patients
- ↑ "Hexvix guided fluorescence cystoscopy reduces recurrence in patients". Archived from the original on 24 July 2011.
- 1 2 "European Association of Urology (EAU)—Guidelines—Online Guidelines". Uroweb.org. Archived from the original on 28 January 2013. Retrieved 10 January 2013.
- ↑ "Types of Bladder Cancer: TCC & Other Variants | CTCA". CancerCenter.com. Retrieved 2018-08-10.
- ↑ Longe, Jacqueline L. (2005). Gale Encyclopedia Of Cancer: A Guide To Cancer And Its Treatments. Detroit: Thomson Gale. p. 137. ISBN 978-1-4144-0362-5.
- ↑ "Survival rates for bladder cancer by stage". American Cancer Society. Archived from the original on 13 October 2015. Last Medical Review: 02/26/2014
- ↑ "How is bladder cancer staged?". American Cancer Society. Archived from the original on 4 October 2015. Last Medical Review: 02/26/2014
- ↑ Chou R, Dana T (October 2010). "Screening adults for bladder cancer: a review of the evidence for the U.S. preventive services task force". Ann. Intern. Med. 153 (7): 461–8. doi:10.7326/0003-4819-153-7-201010050-00009. PMID 20921545.
- ↑ Roberts, Michelle; online (9 July 2013). "Urine odour test for bladder cancer". BBC News. BBC News. Archived from the original on 30 June 2016. Retrieved 19 June 2016.
- 1 2 Brinkman M, Zeegers MP (September 2008). "Nutrition, total fluid and bladder cancer". Scandinavian Journal of Urology and Nephrology. Supplementum. 42 (218): 25–36. doi:10.1080/03008880802285073. PMID 18815914.
- ↑ Brinkman M, Zeegers MP (2006). "Use of selenium in chemoprevention of bladder cancer". Lancet Oncol. 7 (9): 766–74. doi:10.1016/S1470-2045(06)70862-2. PMID 16945772.
- ↑ Valtin H (November 2002). ""Drink at least eight glasses of water a day." Really? Is there scientific evidence for "8 × 8"?". American Journal of Physiology. 283 (5): R993–R1004. doi:10.1152/ajpregu.00365.2002. PMID 12376390. Archived from the original on 4 February 2015.
- ↑ Alexandroff AB, Jackson AM, O'Donnell MA, James K (May 1999). "BCG immunotherapy of bladder cancer: 20 years on". Lancet. 353 (9165): 1689–94. doi:10.1016/S0140-6736(98)07422-4. PMID 10335805.
- ↑ Lamm, Donald L.; Blumenstein, Brent A.; Crawford, E. David; Montie, James E.; Scardino, Peter; Grossman, H. Barton; Stanisic, Thomas H.; Smith Jr, Joseph A.; Sullivan, Jerry; Sarosdy, Michael F.; Crissman, John D.; Coltman, Charles A. (1991). "A Randomized Trial of Intravesical Doxorubicin and Immunotherapy with Bacille Calmette–Guérin for Transitional-Cell Carcinoma of the Bladder". New England Journal of Medicine. 325 (17): 1205–9. doi:10.1056/NEJM199110243251703. PMID 1922207.
- ↑ "Bladder Cancer Stages, Prognosis, Diagnosis, and Treatment". Archived from the original on 11 October 2013.
- ↑ Witjes JA (May 2006). "Management of BCG failures in superficial bladder cancer: a review". European Urology. 49 (5): 790–7. doi:10.1016/j.eururo.2006.01.017. PMID 16464532.
- ↑ Babjuk W, Oosterlinck W, Sylvester R, et al. (2010). "Guidelines on TaT1 (Non-muscle invasive) Bladder Cancer". European Association of Urology. Archived from the original on 24 April 2010.
- ↑ Bladder Cancer Clinical Guideline Update Panel (2007). Bladder Cancer: Guideline for the Management of Nonmuscle Invasive Bladder Cancer: (Stages Ta, T1, and Tis): 2007 Update. American Urological Association.
- ↑ Witjes JA, Hendricksen K (January 2008). "Intravesical pharmacotherapy for non-muscle-invasive bladder cancer: a critical analysis of currently available drugs, treatment schedules, and long-term results". European Urology. 53 (1): 45–52. doi:10.1016/j.eururo.2007.08.015. PMID 17719169.
- ↑ Di Stasi SM, Riedl C (June 2009). "Updates in intravesical electromotive drug administration of mitomycin-C for non-muscle invasive bladder cancer". World Journal of Urology. 27 (3): 325–30. doi:10.1007/s00345-009-0389-x. PMID 19234707.
- ↑ Kos, Bor; Vásquez, Juan Luis; Miklavčič, Damijan; Hermann, Gregers G G; Gehl, Julie (2016). "Investigation of the mechanisms of action behind Electromotive Drug Administration (EMDA)". PeerJ. 4 (e2309). doi:10.7717/peerj.2309. PMC 5012313. PMID 27635313. Archived from the original on 9 October 2016. Retrieved 24 August 2016.
- ↑ Nativ O, Witjes JA, Hendricksen K, et al. (October 2009). "Combined thermo-chemotherapy for recurrent bladder cancer after bacillus Calmette-Guerin". The Journal of Urology. 182 (4): 1313–7. doi:10.1016/j.juro.2009.06.017. PMID 19683278.
- ↑ Colombo R, Da Pozzo LF, Salonia A, et al. (December 2003). "Multicentric study comparing intravesical chemotherapy alone and with local microwave hyperthermia for prophylaxis of recurrence of superficial transitional cell carcinoma". Journal of Clinical Oncology. 21 (23): 4270–6. doi:10.1200/JCO.2003.01.089. PMID 14581436.
- ↑ Alfred Witjes J, Hendricksen K, Gofrit O, Risi O, Nativ O (June 2009). "Intravesical hyperthermia and mitomycin-C for carcinoma in situ of the urinary bladder: experience of the European Synergo working party". World Journal of Urology. 27 (3): 319–24. doi:10.1007/s00345-009-0384-2. PMC 2694311. PMID 19234857.
- ↑ Halachmi S, Moskovitz B, Maffezzini M, et al. (April 2009). "Intravesical mitomycin C combined with hyperthermia for patients with T1G3 transitional cell carcinoma of the bladder". Urologic Oncology. 29 (3): 259–264. doi:10.1016/j.urolonc.2009.02.012. PMID 19395285.
- ↑ Smelser WW, Austenfeld MA, Holzbeierlein JM, Lee EK. Where are we with bladder preservation for muscle-invasive bladder cancer in 2017?. Indian J Urol 2017;33:111-7 http://www.indianjurol.com/text.asp?2017/33/2/111/203415 Archived 10 September 2017 at the Wayback Machine.
- ↑ O'Brien T, Thomas K (November 2010). "Bladder cancer: Photodynamic diagnosis can improve surgical outcome". Nature Reviews Urology. 7 (11): 598–9. doi:10.1038/nrurol.2010.183. PMID 21068759.
- ↑ Advanced Bladder Cancer (ABC) Meta-analysis Collaboration (August 2005). "Neoadjuvant chemotherapy in invasive bladder cancer: update of a systematic review and meta-analysis of individual patient data advanced bladder cancer (ABC) meta-analysis collaboration". Eur. Urol. 48 (2): 202–5, discussion 205–6. doi:10.1016/j.eururo.2005.04.006. PMID 15939524.
- ↑ Grossman HB, Natale RB, Tangen CM, et al. (August 2003). "Neoadjuvant chemotherapy plus cystectomy compared with cystectomy alone for locally advanced bladder cancer". N. Engl. J. Med. 349 (9): 859–66. doi:10.1056/NEJMoa022148. PMID 12944571.
- ↑ Hall R. Updated results of a randomised controlled trial of neoadjuvant cisplatin (C), methotrexate (m) and vinblastin (V) chemotherapy for muscle-invasive bladder cancer. Proc Am Soc Clin Oncol 2002;21:178A, abstr 710.
- ↑ Sherif A, Holmberg L, Rintala E, et al. (March 2004). "Neoadjuvant cisplatinum based combination chemotherapy in patients with invasive bladder cancer: a combined analysis of two Nordic studies". Eur. Urol. 45 (3): 297–303. doi:10.1016/j.eururo.2003.09.019. PMID 15036674.
- ↑ "WHO Disease and injury country estimates". World Health Organization. 2009. Archived from the original on 11 November 2009. Retrieved 11 November 2009.
- ↑ Lozano, R; et al. (15 December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. PMID 23245604.
- ↑ Hemelt M, Zeegers MP (2000). "The effect of smoking on the male excess of bladder cancer: a meta-analysis and geographical analyses". Int J Cancer. 124 (2): 412–9. doi:10.1002/ijc.23856. PMID 18792102.
- ↑ "Scientists Find One Reason Why Bladder Cancer Hits More Men". University of Rochester Medical Center. 20 April 2007. Archived from the original on 11 January 2009. Retrieved 20 April 2007.
- ↑ "Bladder cancer statistics". Cancer Research UK. Archived from the original on 17 October 2014.
External links
| Classification | |
|---|---|
| External resources |
- Bladder cancer at Curlie (based on DMOZ)
- Clinically reviewed bladder cancer information for patients, from Cancer Research UK
- Cancer.Net: Bladder Cancer