Sucralfate
Sucralfate, sold under various brand names, is a medication used to treat stomach ulcers, gastroesophageal reflux disease (GERD), radiation proctitis, and stomach inflammation and to prevent stress ulcers.[2][3][4] Its usefulness in people infected by H. pylori is limited.[2] It is used by mouth and rectally.[2][4]
 | |
| Clinical data | |
|---|---|
| Trade names | Carafate |
| AHFS/Drugs.com | Monograph |
| MedlinePlus | a681049 |
| Pregnancy category |
|
| Routes of administration | By mouth, rectal |
| ATC code |
|
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Bioavailability | 3-5% (local acting) |
| Metabolism | GI; liver: unknown |
| Elimination half-life | unknown |
| Excretion | Feces, urine |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.053.636 |
| Chemical and physical data | |
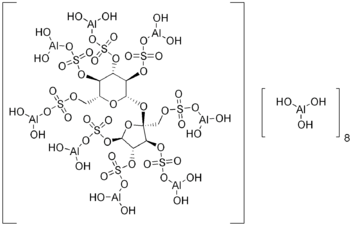
| Formula | C12H54Al16O75S8 |
| Molar mass | 2086.75 g/mol[1] g·mol−1 |
| | |
Common side effects include constipation.[2] Serious side effects may include bezoar formation and encephalopathy.[5] Use appears to be safe in pregnancy and breastfeeding.[5] How it works is unclear but is believed to involve binding to the ulcer and protecting it from further damage.[2][5]
Sucralfate was approved for medical use in the United States in 1981.[2] It is available as a generic medication.[5] In the United States the wholesale cost is about US$0.22 per dose.[6] In 2017, it was the 218th most commonly prescribed medication in the United States, with more than two million prescriptions.[7][8]
Medical uses
Sucralfate is used for the treatment of active duodenal ulcers not related to the use of nonsteroidal anti-inflammatory drugs (NSAIDs), as the mechanism behind these ulcers is due to acid oversecretion.[9] It is not FDA approved for gastric ulcers, but is widely used because of evidence of efficacy.[10] The use for sucralfate in peptic ulcer disease has diminished recently, but it is still the preferred agent for stress ulcer prevention.[11][12][13][14]
Sucralfate has also been used for the following conditions:
- Active duodenal ulcer not related to NSAID use
- Maintenance therapy for resolved duodenal ulcers
- Gastric ulcer not related to NSAID use and gastritis due to GERD—Triple combination therapy with lansoprazole + cisapride + sucralfate can significantly improve symptoms and quality of life and was more cost-effective than ranitidine combination group.[15]
- Aphthous ulcer and stomatitis due to radiation or chemotherapy—The 2013 guidelines of the International Society of Oral Oncology does not recommended sucralfate for the prevention of oral mucositis in head and neck cancer patients receiving radiotherapy or chemoradiation due to a lack of efficacy found in a well-designed, randomized controlled trial.[16]
- Gastro-esophageal reflux disease during pregnancy—First-line drug therapy combined with lifestyle and diet modification.[17]
- Stress ulcer prophylaxis—The use of sucralfate rather than H2 antagonists for stress ulcer prophylaxis, and measures to prevent aspiration, such as continuous subglottic suctioning, have been shown to reduce the risk of ventilator-associated pneumonia (VAP).[18] Sucralfate is less effective for prophylaxis against gastrointestinal bleeding than either a PPI or H2-blocker. For that reason, it is not commonly used for stress ulcer prophylaxis.
- Prevention of stricture formation—Sucralfate has an inhibitory effect on stricture formation in experimental corrosive burns and can be used in the treatment of corrosive esophageal burns to enhance mucosal healing and suppress stricture formation[19]
- Proctitis from ulcerative colitis[20]
- Rectal bleeding due to proctitis from radiation to treat cancers of the cervix, prostate, and colon.[4]
- Grade 1 bleeding experienced immediate relief with sucrasulfate enema for 1 month.
- Grade 2 bleeding, sucrasulfate enema] and/or coagulation were effective.
- Grade 3 bleeding lasted for 1 year despite frequent transfusions and coagulation.
- Grade 2 and 3 rectal bleeding occurred in 8.5% of people. The most significant risk factor was the ICRU-CRBED. Prompt treatment with a combination of sucrasulfate enema and coagulation is effective in controlling Grade 1 and 2 rectal bleeding without the development of fistula or stricture.[21]
- Treatment of anastomotic ulcer after gastric bypass surgery
- Sucralfate suspension is recommended by the US-based National Capital Poison Center (Poison Control) as an intervention for known or suspected button battery ingestions to reduce the risk and severity of injury to the esophagus prior to the battery's endoscopic removal.[22][23]
- Protection against ventilator-associated pneumonia - Reductions in gastric acidity and volumes increase bacterial overgrowth and the incidence of ventilator-associated pneumonia. Sucralfate may be considered to have the advantage over H2-blockers and PPIs in this regard because sucralfate does not change the pH of gastric fluid. A majority of meta-analyses found that sucralfate therapy decreased the incidence of ventilator-associated pneumonia compared to H2-antagonists.[10]
Side effects
The most common side effect seen is constipation (2-3%). Less commonly reported side effects (<0.5%) include flatulence, headache, hypophosphatemia, xerostomia (dry mouth), and bezoar formation.[24][25][26] Use of this drug is not recommended for people with chronic kidney failure, as it might cause aluminium accumulation and toxicity. A few well-controlled studies have been carried out investigating the safety and efficacy of sucralfate in children and pregnant women (Pregnancy Category B).[9][27][28]
Mechanism of action
Sucralfate is a locally acting substance that in an acidic environment (pH < 4) reacts with hydrochloric acid in the stomach to form a cross-linking, viscous, paste-like material capable of acting as an acid buffer for as long as 6 to 8 hours after a single dose.[29] It also attaches to proteins on the surface of ulcers, such as albumin and fibrinogen, to form stable insoluble complexes. These complexes serve as protective barriers at the ulcer surface, preventing further damage from acid, pepsin, and bile.[29] In addition, sucralfate prevents back diffusion of hydrogen ions, and adsorbs both pepsin and bile acids.
It has been thought that sucralfate also stimulates the production of prostaglandin E2, epidermal growth factors (EGF), bFGF, and gastric mucus.[9][30]
Pharmacokinetics
Onset: 1-2 hr (initial onset for peptic ulcer disease (PUD))
Absorption: <5% Orally
Duration: Up to 6 hours due to high affinity for defective mucosa (PUD)
Bioavailability: 5% as sucralfate is considered non-systemic, sucrose octasulfate: 5%, aluminum:0.005%
Metabolism: Not metabolized, excreted unchanged in urine
Names
Brand names include Carafate in U.S.A., Sucramal in Italy, Sucrafil, Sufrate, Sucralpro, Sucralcoat, Pepsigard, Sucral, Hapifate, Sucralpro in India, Sutra or Musin in parts of South-East Asia, Sulcrate in Canada, Discral (sucralfato) in México, Ulsanic in South Africa and Israel, Andapsin in Sweden and Antepsin in Turkey.
References
- Merck Index, 12th Edition, 9049.
- "Sucralfate Monograph for Professionals". Drugs.com. American Society of Health-System Pharmacists.
- Maton PN (November 2003). "Profile and assessment of GERD pharmacotherapy". Cleveland Clinic Journal of Medicine. 70 Suppl 5: S51-70. doi:10.3949/ccjm.70.Suppl_5.S51. PMID 14705381.
- Mendenhall WM, McKibben BT, Hoppe BS, Nichols RC, Henderson RH, Mendenhall NP (October 2014). "Management of radiation proctitis". American Journal of Clinical Oncology. 37 (5): 517–23. doi:10.1097/COC.0b013e318271b1aa. PMID 23241500.
- British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. p. 73. ISBN 9780857113382.
- "NADAC as of 2019-02-27". Centers for Medicare and Medicaid Services. Retrieved 3 March 2019.
- "The Top 300 of 2020". ClinCalc. Retrieved 11 April 2020.
- "Sucralfate - Drug Usage Statistics". ClinCalc. Retrieved 11 April 2020.
- "DailyMed - CARAFATE - sucralfate suspension". dailymed.nlm.nih.gov. Retrieved 2015-11-04.
- Hixson LJ, Kelley CL, Jones WN, Tuohy CD (April 1992). "Current trends in the pharmacotherapy for peptic ulcer disease". Archives of Internal Medicine. 152 (4): 726–32. doi:10.1001/archinte.152.4.726. PMID 1558429.
- Hunt RH (August 1991). "Treatment of peptic ulcer disease with sucralfate: a review". The American Journal of Medicine. 91 (2A): 102S–106S. doi:10.1016/0002-9343(91)90459-b. PMID 1882894.
- Fashner J, Gitu AC (February 2015). "Diagnosis and Treatment of Peptic Ulcer Disease and H. pylori Infection". American Family Physician. 91 (4): 236–42. PMID 25955624.
- "ASHP Therapeutic Guidelines on Stress Ulcer Prophylaxis. ASHP Commission on Therapeutics and approved by the ASHP Board of Directors on November 14, 1998". American Journal of Health-System Pharmacy. 56 (4): 347–79. February 1999. doi:10.1093/ajhp/56.4.347. PMID 10690219.
- Monnig AA, Prittie JE (October 2011). "A review of stress-related mucosal disease". Journal of Veterinary Emergency and Critical Care. 21 (5): 484–95. doi:10.1111/j.1476-4431.2011.00680.x. PMID 22316196.
- Si JM, Wang LJ, Chen SJ, Zhao L, Dai N (2003). "Quality of life and cost-effectiveness of combined therapy for reflux esophagitis". Journal of Zhejiang University. Science. 4 (5): 602–6. doi:10.1631/jzus.2003.0602. PMID 12958722.
- Saunders DP, Epstein JB, Elad S, Allemano J, Bossi P, van de Wetering MD, et al. (November 2013). "Systematic review of antimicrobials, mucosal coating agents, anesthetics, and analgesics for the management of oral mucositis in cancer patients". Supportive Care in Cancer. 21 (11): 3191–207. doi:10.1007/s00520-013-1871-y. PMID 23832272.
- Richter JE (November 2005). "Review article: the management of heartburn in pregnancy". Alimentary Pharmacology & Therapeutics. 22 (9): 749–57. doi:10.1111/j.1365-2036.2005.02654.x. PMID 16225482.
- Safdar N, Crnich CJ, Maki DG (June 2005). "The pathogenesis of ventilator-associated pneumonia: its relevance to developing effective strategies for prevention". Respiratory Care. 50 (6): 725–39, discussion 739–41. PMID 15913465.
- Temir ZG, Karkiner A, Karaca I, Ortaç R, Ozdamar A (2005-01-01). "The effectiveness of sucralfate against stricture formation in experimental corrosive esophageal burns". Surgery Today. 35 (8): 617–22. doi:10.1007/s00595-004-3005-0. PMID 16034539.
- Theodore M. Bayless (14 May 2014). Advanced Therapy of Inflammatory Bowel Disease: Ulcerative Colitis (Volume 1), 3e. PMPH-USA. p. 331. ISBN 978-1-60795-216-9.
- Chun M, Kang S, Kil HJ, Oh YT, Sohn JH, Ryu HS (January 2004). "Rectal bleeding and its management after irradiation for uterine cervical cancer". International Journal of Radiation Oncology, Biology, Physics. 58 (1): 98–105. doi:10.1016/s0360-3016(03)01395-6. PMID 14697426.
- "Guideline". www.poison.org. Retrieved 2018-07-05.
- Anfang RR, Jatana KR, Linn RL, Rhoades K, Fry J, Jacobs IN (January 2019). "pH-neutralizing esophageal irrigations as a novel mitigation strategy for button battery injury". The Laryngoscope. 129 (1): 49–57. doi:10.1002/lary.27312. PMID 29889306.
- "Study of possible correlation between BEZOAR and SUCRALFATE". MedsFacts.com. Archived from the original on 18 September 2016.
- "Carafate Package Insert" (PDF). September 12, 2013. Retrieved November 2, 2015.
- "ASHP Therapeutic Guidelines on Stress Ulcer Prophylaxis. ASHP Commission on Therapeutics and approved by the ASHP Board of Directors on November 14, 1998". American Journal of Health-System Pharmacy. 56 (4): 347–79. February 1999. doi:10.1093/ajhp/56.4.347. PMID 10690219.
- Phupong V, Hanprasertpong T (September 2015). "Interventions for heartburn in pregnancy". The Cochrane Database of Systematic Reviews. 9 (9): CD011379. doi:10.1002/14651858.CD011379.pub2. PMID 26384956.
- Steiner K, Bühring KU, Faro HP, Garbe A, Nowak H (1982-01-01). "Sucralfate: pharmacokinetics, metabolism and selective binding to experimental gastric and duodenal ulcers in animals". Arzneimittel-Forschung. 32 (5): 512–8. PMID 6896647.
- Brogden RN, Heel RC, Speight TM, Avery GS (March 1984). "Sucralfate. A review of its pharmacodynamic properties and therapeutic use in peptic ulcer disease". Drugs. 27 (3): 194–209. doi:10.2165/00003495-198427030-00002. PMID 6368184.
- Korman MG, Bolin TD, Szabo S, Hunt RH, Marks IN, Glise H (1994-08-01). "Sucralfate: the Bangkok review". Journal of Gastroenterology and Hepatology. 9 (4): 412–5. doi:10.1111/j.1440-1746.1994.tb01264.x. PMID 7948825.
- McEvoy GK (2007). AHFS drug information McEvoy GK, ed. Sucralfate. AHFS. pp. 2983–5.