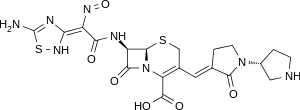
Ceftobiprole
Ceftobiprole (Zevtera/Mabelio) is a new 5th-generation[2] cephalosporin for the treatment of hospital-acquired pneumonia (excluding ventilator-associated pneumonia) and community-acquired pneumonia. It is marketed by Basilea Pharmaceutica in the United Kingdom, Germany, Switzerland and Austria under the trade name Zevtera, in France and Italy under the trade name Mabelio.[3] Like other cephalosporins, ceftobiprole exerts its antibacterial activity by binding to important penicillin-binding proteins and inhibiting their transpeptidase activity which is essential for the synthesis of bacterial cell walls. Ceftobiprole has high affinity for penicillin-binding protein 2a of methicillin-resistant Staphylococcus aureus strains and retains its activity against strains that express divergent mecA gene homologues (mecC or mecALGA251). Ceftobiprole also binds to penicillin-binding protein 2b in Streptococcus pneumoniae (penicillin-intermediate), to penicillin-binding protein 2x in Streptococcus pneumoniae (penicillin-resistant), and to penicillin-binding protein 5 in Enterococcus faecalis.[4]
 | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | International Drug Names |
| Routes of administration | Intravenous |
| ATC code | |
| Legal status | |
| Legal status |
|
| Identifiers | |
| |
| CAS Number |
|
| PubChem CID | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.129.666 |
| Chemical and physical data | |
| Formula | C20H22N8O6S2 |
| Molar mass | 534.57 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Microbiology
Ceftobiprole has shown in vitro antimicrobial activity against a broad range of Gram-positive and Gram-negative pathogens. Among the Gram-positive pathogens, ceftobiprole has demonstrated good in vitro activity against methicillin-resistant Staphylococcus aureus, methicillin-susceptible Staphylococcus aureus and coagulase-negative staphylococci, as well as against strains of methicillin-resistant Staphylococcus aureus with reduced susceptibility to linezolid, daptomycin or vancomycin.[5] Ceftobiprole has also displayed potent activity against Streptococcus pneumoniae (including penicillin-sensitive, penicillin-resistant and ceftriaxone-resistant strains) and Enterococcus faecalis, but not against Enterococcus faecium. For Gram-negative pathogens, ceftobiprole has shown good in vitro activity against Haemophilus influenzae (including both ampicillin-susceptible and ampicillin-non-susceptible isolates), Pseudomonas aeruginosa and strains of Escherichia coli, Klebsiella pneumoniae and Proteus mirabilis that do not produce extended-spectrum β-lactamases (ESBL). Like all other cephalosporins, ceftobiprole was inactive against strains that produce extended-spectrum β-lactamases.[6]
The efficacy of ceftobiprole has been demonstrated in two large randomized, double-blind, phase 3 clinical trials in patients with hospital-acquired and community-acquired pneumonia. Ceftobiprole was non-inferior to ceftazidime plus linezolid in the treatment of hospital-acquired pneumonia (excluding ventilator-acquired pneumonia) and non-inferior to ceftriaxone with or without linezolid in the treatment of community-acquired pneumonia.[7][8]
Pharmacology
(1)_(30204271666).jpg)
Ceftobiprole is the active moiety of the prodrug ceftobiprole medocaril and is available for intravenous treatment only. The recommended dose is 500 mg as 2-hour infusion every 8 hours. It is mainly excreted renally. Dose adjustment is required for patients with moderate or severe renal impairment and for patients with end-stage renal disease, but no dose adjustment is needed by gender, ethnicity or age, in severely obese patients or in patients with hepatic impairment.[9]
Regulatory approvals
(1)_(29608654394).jpg)
Ceftobiprole has been approved for the treatment of adult patients with hospital acquired pneumonia (excluding ventilator-acquired pneumonia) and community-acquired pneumonia in 12 European countries, Canada and Switzerland.[10]
References
- WHO International Working Group for Drug Statistics Methodology (August 27, 2008). "ATC/DDD Classification (FINAL): New ATC 5th level codes". WHO Collaborating Centre for Drug Statistics Methodology. Archived from the original on 2008-05-06. Retrieved 2008-09-05.
- Scheeren, Thomas W. L. (2015-01-01). "Ceftobiprole medocaril in the treatment of hospital-acquired pneumonia". Future Microbiology. 10 (12): 1913–1928. doi:10.2217/fmb.15.115. ISSN 1746-0921. PMID 26573022.
- "Basilea to launch Zevtera®/Mabelio® (ceftobiprole medocaril) in Europe through a commercial services provider". Basilea Pharmaceutica. Archived from the original on 2019-03-31. Retrieved 2016-09-20.
- Syed, Yahiya Y. (2014-09-01). "Ceftobiprole medocaril: a review of its use in patients with hospital- or community-acquired pneumonia". Drugs. 74 (13): 1523–1542. doi:10.1007/s40265-014-0273-x. ISSN 0012-6667. PMID 25117196.
- Zhanel GG, Lam A, Schweizer F, Thomson K, Walkty A, Rubinstein E, Gin AS, Hoban DJ, Noreddin AM, Karlowsky JA (2008). "Ceftobiprole: a review of a broad-spectrum and anti-methicillin-resistant Staphylococcus aureuscephalosporin". American Journal of Clinical Dermatology. 9: 245–54. doi:10.2165/00128071-200809040-00004. PMID 18572975.
- Farrell, David J.; Flamm, Robert K.; Sader, Helio S.; Jones, Ronald N. (2014-07-01). "Ceftobiprole activity against over 60,000 clinical bacterial pathogens isolated in Europe, Turkey, and Israel from 2005 to 2010". Antimicrobial Agents and Chemotherapy. 58 (7): 3882–3888. doi:10.1128/AAC.02465-14. ISSN 1098-6596. PMC 4068590. PMID 24777091.
- Farrell, David J.; Flamm, Robert K.; Sader, Helio S.; Jones, Ronald N. (2014-04-01). "Activity of ceftobiprole against methicillin-resistant Staphylococcus aureus strains with reduced susceptibility to daptomycin, linezolid or vancomycin, and strains with defined SCCmec types". International Journal of Antimicrobial Agents. 43 (4): 323–327. doi:10.1016/j.ijantimicag.2013.11.005. ISSN 1872-7913. PMID 24411474.
- Nicholson, Susan C.; Welte, Tobias; File, Thomas M.; Strauss, Richard S.; Michiels, Bart; Kaul, Pratibha; Balis, Dainius; Arbit, Deborah; Amsler, Karen (2012-03-01). "A randomised, double-blind trial comparing ceftobiprole medocaril with ceftriaxone with or without linezolid for the treatment of patients with community-acquired pneumonia requiring hospitalisation". International Journal of Antimicrobial Agents. 39 (3): 240–246. doi:10.1016/j.ijantimicag.2011.11.005. ISSN 1872-7913. PMID 22230331.
- Awad, Samir S.; Rodriguez, Alejandro H.; Chuang, Yin-Ching; Marjanek, Zsuszanna; Pareigis, Alex J.; Reis, Gilmar; Scheeren, Thomas W. L.; Sánchez, Alejandro S.; Zhou, Xin (2014-07-01). "A phase 3 randomized double-blind comparison of ceftobiprole medocaril versus ceftazidime plus linezolid for the treatment of hospital-acquired pneumonia". Clinical Infectious Diseases. 59 (1): 51–61. doi:10.1093/cid/ciu219. ISSN 1537-6591. PMC 4305133. PMID 24723282.
- Basilea Medical Ltd. Summary of Product Characteristics: Zevtera 500 mg powder for concentrate for solution for infusion. Medicines and Healthcare Products Regulatory Agency.http://www.mhra.gov.uk/spc
- Hebeisen P, Heinze-Krauss I, Angehrn P, et al. (2001). "In vitro and in vivo properties of Ro63-9141, a novel broad-spectrum cephalosporin with activity against methicillin-resistant staphylococci". Antimicrobial Agents and Chemotherapy. 45 (3): 825–36. doi:10.1128/AAC.45.3.825-836.2001. PMC 90381. PMID 11181368.
- Jones RN, Deshpande LM, Mutnick AH, Biedenbach DJ (2002). "In vitro evaluation of BAL9141, a novel parenteral cephalosporin active against oxacillin-resistant staphylococci". Journal of Antimicrobial Chemotherapy. 50 (6): 915–932. doi:10.1093/jac/dkf249. PMID 12461013.