Spastic cerebral palsy
| Spastic cerebral palsy | |
|---|---|
 | |
| Spastic hand(hemiplegia) | |
| Classification and external resources | |
| ICD-10 | G80 |
| ICD-9-CM | 343 |
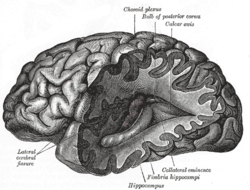
Spastic cerebral palsy is the type of cerebral palsy wherein spasticity is the exclusive impairment present. Itself an umbrella term encompassing spastic hemiplegia, spastic diplegia, spastic quadriplegia and — where solely one limb or one specific area of the body is affected— spastic monoplegia. Spastic cerebral palsy affects the cerebral cortex[1] and is overwhelmingly the most common type of overall cerebral palsy.
The Society for Cerebral Palsy in Europe (SCPE) estimates that the spasticity-only cerebral palsy classification sweeps in 90% of global cerebral palsy cases. But even if the 90% assertion is an exaggeration, more conservative scientific estimates still place the prevalence of spasticity-dominant or spasticity-only cerebral palsy at anywhere from 70–80% of all cases, leaving cases dominated by ataxic cerebral palsy, dyskinetic cerebral palsy and athetoid cerebral palsy trailing at 20–30%.
Presentation
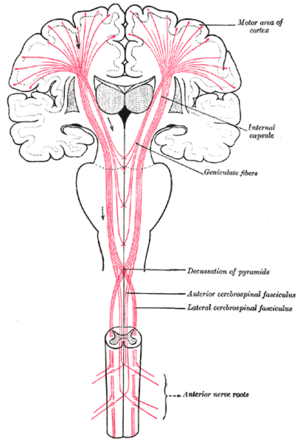
People with the spastic/spasticity type of CP are hypertonic—i.e., they present with very stiff and tight muscle groups, far greater than typical humans—and have what is essentially a neuromuscular mobility impairment (rather than hypotonia or paralysis) which stems from an upper motor neuron lesion in the brain. The corticospinal tract or the motor cortex may be secondarily affected.
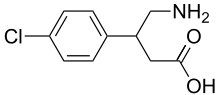
Spastic muscles are continuously contracting, or "tight", because the corresponding nerves permanently over-fire the command to tighten. This is caused by their inability to properly absorb GABA, or gamma amino butyric acid. The tightness, in addition to restricting movement, also acts as an overwhelming opposing force to neighbouring muscles and joints, eventually leaving the entire skeleton deformed. Ankle equines and hip migration are the two most prevalent deformities in cerebral palsy children. [2], [3] Abnormal postures or deformities are usually associated with the antigravity muscles, which are extensors in the leg and the flexors in the arm. At the beginning these deformities are dynamic in nature but over time they become static or fixed also known as joint contractures. This is especially true if physiotherapy is not instituted in a timely and adequate fashion. [2], [3], [4]
Changes in spasticity and corresponding postures may also occur with other brain activity, such as excitement, fear or anxiety, or even pain, which increase muscle tension.
A person with spastic CP will commonly show, in addition to higher muscle tone, persistent primitive reflexes, greater stretch reflexes, plantar reflex, and ankle clonus.[5]
A third of people with cerebral palsy have seizures - this is most common in spastic CP.[6]. Audiovisual, cognitive compromise and behavioral disorders can occur.
Mechanism
The upper motor neuron lesion in the brain impairs the ability of some nerve receptors in the spine to properly receive gamma amino butyric acid (GABA). That leads to hypertonia in the muscles signaled by those damaged nerves. The limbs and body areas in which hypertonia manifests can be any or even all of them, depending which specific nerve groupings within the spine are rendered unable to receive GABA. Thus, spastic CP is often designated by body topography.
Diagnosis

Types
Scientific classifications
In some cases, spastic cerebral palsy is caused by genetic factors.[7] The genetic factors for spastic cerebral palsy include:
| Type | OMIM | Gene | Locus |
|---|---|---|---|
| CPSQ1 | 603513 | GAD1 | 2q31 |
| CPSQ2 | 612900 | ANKRD15 | 9p24.3 |
| CPSQ3 | 612936 | AP4M1 | 7q22.1 |
Although it has its origins in a brain injury, spastic CP can largely be thought of as a collection of orthopaedic and neuromuscular issues because of how it manifests symptomatically over the course of the person's lifespan. It is therefore not the same as "brain damage" and it need not be thought of as such. Spastic quadriplegia in particular, especially if it is combined with verbal speech challenges and strabismus, may be misinterpreted by the general population as alluding to cognitive dimensions to the disability atop the physical ones, but this is false; the intelligence of a person with any type of spastic CP is unaffected by the condition of the spasticity itself.
- Spastic hemiplegia is one side being affected. Generally, injury to muscle-nerves controlled by the brain's left side will cause a right body deficit, and vice versa. Typically, people that have spastic hemiplegia are the most ambulatory of all the forms, although they generally have dynamic equinus (a limping instability) on the affected side and are primarily prescribed ankle-foot orthoses to prevent said equinus.[8]
- Spastic diplegia is the lower extremities affected, with little to no upper-body spasticity. The most common form of the spastic forms (70–80% of known cases), most people with spastic diplegia are fully ambulatory, but are "tight" and have a scissors gait. Flexed knees and hips to varying degrees, and moderate to severe adduction (stemming from tight adductor muscles and comparatively weak abductor muscles), are present. Gait analysis is often done in early life on a semi-regular basis, and assistive devices are often provided like walkers, crutches or canes; any ankle-foot orthotics provided usually go on both legs rather than just one.[9]
- Spastic monoplegia is one single limb being affected.[10]
- Spastic triplegia is three limbs being affected.[11]
- Spastic quadriplegia is all four limbs more or less equally affected.[12] People with spastic quadriplegia are the least likely to be able to walk, or if they can, to desire to walk, because their muscles are too tight and it is too much of an effort to do so. Some children with spastic quadriplegia also have hemiparetic tremors, an uncontrollable shaking that affects the limbs on one side of the body and impairs normal movement. (This is not the same as clonus; see below.)
In spastic cerebral palsy in children with low birth weights, 25% of children had hemiplegia, 37.5% had quadriplegia, and 37.5% had diplegia.[13]
Treatment
In any manifestation of spastic CP, clonus of the affected limb(s) may intermittently result, as well as muscle spasms, each of which results from the pain and/or stress of the tightness experienced, indicating especially hard-working and/or exhausted musculature. The spasticity itself can and usually does also lead to very early onset of muscle-stress symptoms like arthritis and tendinitis, especially in ambulatory individuals in their mid-20s and early-30s. As compared to other types of CP, however, and especially as compared to hypotonic CP or more general paralytic mobility disabilities, spastic CP is typically more easily manageable by the person affected, and medical treatment can be pursued on a multitude of orthopaedic and neurological fronts throughout life.
Physical therapy and occupational therapy regimens of assisted stretching, strengthening, functional tasks, and/or targeted physical activity and exercise are usually the chief ways to keep spastic CP well-managed, although if the spasticity is too much for the person to handle, other remedies may be considered, such as various antispasmodic medications, botox, baclofen, or even a neurosurgery known as a selective dorsal rhizotomy (which eliminates the spasticity by eliminating the nerves causing it).
Prognosis
Spasticity increases as people with spastic CP age.[14] Cerebral palsy, including spastic cerebral palsy, is notable for a glaring overall research deficiency—the fact that it is one of the very few major groups of conditions on the planet in human beings for which medical science has not yet (as of 2011) collected wide-ranging empirical data on the development and experiences of young adults, the middle aged and older adults. An especially puzzling aspect of this lies in the fact that cerebral palsy as defined by modern science was first "discovered" and specifically addressed well over 100 years ago and that it would therefore be reasonable to expect by now that at least some empirical data on the adult populations with these conditions would have long since been collected, especially over the second half of the 20th century when existing treatment technologies rapidly improved and new ones came into being. The vast majority of empirical data on the various forms of cerebral palsy is concerned near-exclusively with children (birth to about 10 years of age) and sometimes pre-teens and early teens (11–13). Some doctors attempt to provide their own personal justifications for keeping their CP specialities purely paediatric, but there is no objectively apparent set of reasons backed by any scientific consensus as to why medical science has made a point of researching adult cases of multiple sclerosis, muscular dystrophy and the various forms of cancer in young and older adults, but has failed to do so with CP.
See also
References
- ↑ James, Susan R.; Nelson, Kristine; Ashwill, Jean (2013). Nursing Care of Children: Principles and Practice. Elsevier Health Sciences. p. 747. ISBN 9780323293457. Retrieved 15 January 2017.
- 1 2 El-Sobky TA, Fayyad TA, Kotb AM, Kaldas B (2017)."Bony reconstruction of hip in cerebral palsy children Gross Motor Function Classification System levels III to V: a systematic review". J Pediatric Orthopaedics B . http://doi.org/10.1097/BPB.0000000000000503. PMID 28953164
- 1 2 Shore BJ, White N, Graham H (2010). " Surgical correction of equinus deformity in children with cerebral palsy: a systematic review". J Child Orthop 4.: 277–90. http://doi.org/10.1007/s11832-010-0268-4
- ↑ Agarwal, Anil; Verma, Indreshwar (December 2012). "Cerebral palsy in children: An overview". Journal of Clinical Orthopaedics and Trauma. 3 (2): 77–81. doi:10.1016/j.jcot.2012.09.001. PMC 3872805. PMID 26403442.
- ↑ Sobralske, Mary C. (2013). "Common Physical or Sensory Disabilities". In Eddy, Linda L. Caring for children with special healthcare needs and their families a handbook for healthcare professionals. Ames, Iowa: Wiley-Blackwell. p. 13. ISBN 9781118783290.
- ↑ Shaikh, SafiyaImtiaz; Hegade, Ganapati (2017). "Role of anesthesiologist in the management of a child with cerebral palsy". Anesthesia: Essays and Researches. 11 (3): 544. doi:10.4103/0259-1162.194569. PMC 5594763. PMID 28928544.
- ↑ "OMIM Entry - # 603513 - CEREBRAL PALSY, SPASTIC QUADRIPLEGIC, 1; CPSQ1". omim.org. Retrieved 16 January 2017.
- ↑ Birol Balaban, Evren Yasar, Ugur Dal, Kamil Yazicioglu, Haydar Mohur & Tunc Alp Kalyon "The effect of hinged ankle-foot orthosis on gait and energy expenditure in spastic hemiplegic cerebral palsy" Disability and Rehabilitation, January 2007; 29(2): 139–144
- ↑ "Spastic diplegia cerebral palsy | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 15 January 2017.
- ↑ "Cerebral palsy spastic monoplegic | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 15 January 2017.
- ↑ Panteliadis, Christos P.; Strassburg, Hans-Michael (2004). Cerebral Palsy: Principles and Management. Thieme. p. 19. ISBN 9781588902955. Retrieved 15 January 2017.
- ↑ "Cerebral palsy spastic quadriplegic | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 15 January 2017.
- ↑ O’Shea, TM (2008). "Diagnosis, Treatment, and Prevention of Cerebral Palsy". Clinical Obstet Gynecol. 51 (4): 816–28. doi:10.1097/GRF.0b013e3181870ba7. PMC 3051278. PMID 18981805.
- ↑ Kent, Ruth M. (2012). "Cerebral palsy". In Barnes, Michael; Good, David. Neurological Rehabilitation Handbook of Clinical Neurology. Oxford: Elsevier Science. pp. 443–459. ISBN 9780444595843.