Pressure ulcer
| Pressure ulcer | |
|---|---|
| Synonyms | decubitus ulcers |
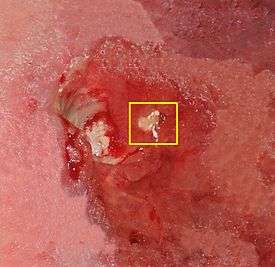 | |
| Stage IV decubitus displaying the tuberosity of the ischium protruding through the tissue and possible onset of osteomyelitis | |
| Specialty | Plastic surgery |
Pressure ulcers, also known as pressure sores, decubitus ulcers, and bedsores, and now referred to as pressure injuries are localized damage to the skin and/or underlying tissue that usually occur over a bony prominence as a result of pressure or pressure in combination with shear and/or friction. The most common sites are the skin overlying the sacrum, coccyx, heels or the hips, but other sites such as the elbows, knees, ankles, back of shoulders, or the back of the cranium can be affected.
Pressure ulcers occur due to pressure applied to soft tissue resulting in completely or partially obstructed blood flow to the soft tissue. Shear is also a cause, as it can pull on blood vessels that feed the skin. Pressure ulcers most commonly develop in individuals who are not moving about, such as those being bedridden or confined to a wheelchair. It is widely believed that other factors can influence the tolerance of skin for pressure and shear, thereby increasing the risk of pressure ulcer development. These factors are protein-calorie malnutrition, microclimate (skin wetness caused by sweating or incontinence), diseases that reduce blood flow to the skin, such as arteriosclerosis, or diseases that reduce the sensation in the skin, such as paralysis or neuropathy. The healing of pressure ulcers may be slowed by the age of the person, medical conditions (such as arteriosclerosis, diabetes or infection), smoking or medications such as anti-inflammatory drugs.
Although often prevented and treatable if detected early, pressure ulcers can be very difficult to prevent in critically ill people, frail elders and individuals with impaired mobility such as wheelchair users (especially where spinal injury is involved). Primary prevention is to redistribute pressure by regularly turning the person. The benefit of turning to avoid further sores is well documented since at least the 19th century. In addition to turning and re-positioning the person in the bed or wheelchair, eating a balanced diet with adequate protein and keeping the skin free from exposure to urine and stool is very important.
The rate of pressure ulcers in hospital settings is high; the prevalence in European hospitals ranges from 8.3% to 23%, and the prevalence is 26% in Canadian healthcare settings.[1] In 2013, there were 29,000 documented deaths from pressure ulcers globally, up from 14,000 deaths in 1990.[2]
Presentation
Complications
Pressure ulcers can trigger other ailments, cause considerable suffering, and can be expensive to treat. Some complications include autonomic dysreflexia, bladder distension, bone infection, pyarthroses, sepsis, amyloidosis, anemia, urethral fistula, gangrene and very rarely malignant transformation (Marjolin's ulcer - secondary carcinomas in chronic wounds). Sores may recur if those with pressure ulcers do not follow recommended treatment or may instead develop seromas, hematomas, infections, or wound dehiscence. Paralyzed individuals are the most likely to have pressure sores recur. In some cases, complications from pressure sores can be life-threatening. The most common causes of fatality stem from kidney failure and amyloidosis. Pressure ulcers are also painful, with individuals of all ages and all stages of pressure ulcers reporting pain.
Cause
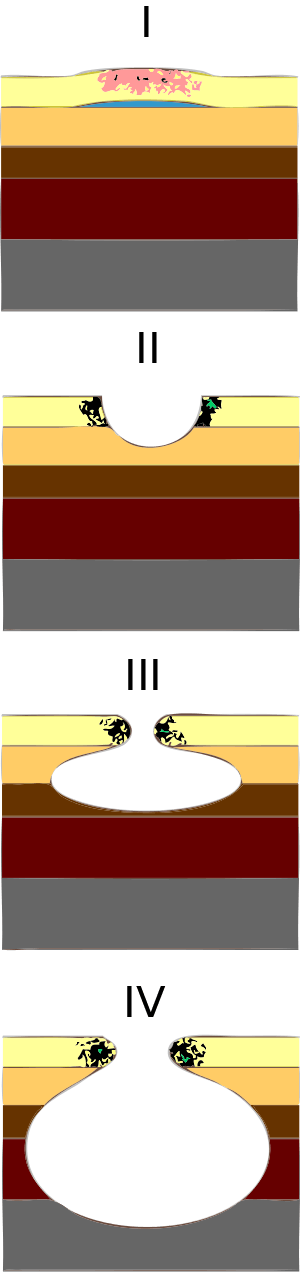
There are four mechanisms that contribute to pressure ulcer development:[3]
- External (interface) pressure applied over an area of the body, especially over the bony prominences can result in obstruction of the blood capillaries, which deprives tissues of oxygen and nutrients, causing ischemia (deficiency of blood in a particular area), hypoxia (inadequate amount of oxygen available to the cells), edema, inflammation, and, finally, necrosis and ulcer formation. Ulcers due to external pressure occur over the sacrum and coccyx, followed by the trochanter and the calcaneus (heel).
- Friction is damaging to the superficial blood vessels directly under the skin. It occurs when two surfaces rub against each other. The skin over the elbows and can be injured due to friction. The back can also be injured when patients are pulled or slid over bed sheets while being moved up in bed or transferred onto a stretcher.
- Shearing is a separation of the skin from underlying tissues. When a patient is partially sitting up in bed, their skin may stick to the sheet, making them susceptible to shearing in case underlying tissues move downward with the body toward the foot of the bed. This may also be possible on a patient who slides down while sitting in a chair.
- Moisture is also a common pressure ulcer culprit. Sweat, urine, feces, or excessive wound drainage can further exacerbate the damage done by pressure, friction, and shear. It can contribute to maceration of surrounding skin thus potentially expanding the deleterious effects of pressure ulcers.
Risk Factors
There are over 100 risk factors for pressure ulcers.[4] Factors that may place a patient at risk include immobility, diabetes mellitus, peripheral vascular disease, malnutrition, cerebral vascular accident and hypotension.[4][5] Other factors are age of 70 years and older, current smoking history, dry skin, low body mass index, urinary and fecal incontinence, physical restraints, malignancy, and history of pressure ulcers.
Pathophysiology
Pressure ulcers may be caused by inadequate blood supply and resulting reperfusion injury when blood re-enters tissue. A simple example of a mild pressure sore may be experienced by healthy individuals while sitting in the same position for extended periods of time: the dull ache experienced is indicative of impeded blood flow to affected areas. Within 2 hours, this shortage of blood supply, called ischemia, may lead to tissue damage and cell death. The sore will initially start as a red, painful area. The other process of pressure ulcer development is seen when pressure is high enough to damage the cell membrane of muscle cells. The muscle cells die as a result and skin fed through blood vessels coming through the muscle die. This is the deep tissue injury form of pressure ulcers and begins as purple intact skin.
According to Centers for Medicare and Medicaid Services, pressure ulcers are one of the eight preventable iatrogenic illnesses. If a pressure ulcer is acquired in the hospital the hospital will no longer receive reimbursement for the person's care. Hospitals spend about $5 billion annually for treatment of pressure ulcers.[6]
Sites
Common pressure sore sites include the skin over the ischial tuberosity, the sacrum, the heels of the feet, over the heads of the long bones of the foot, buttocks, over the shoulder, and over the back of the head.[7]
Biofilm
Biofilm is one of the most common reasons for delayed healing in pressure ulcers. Biofilm occurs rapidly in wounds and stalls healing by keeping the wound inflamed. Frequent debridement and antimicrobial dressings are needed to control the biofilm. Infection prevents healing of pressure ulcers. Signs of pressure ulcer infection include slow or delayed healing and pale granulation tissue. Signs and symptoms of systemic infection include fever, pain, redness, swelling, warmth of the area, and purulent discharge. Additionally, infected wounds may have a gangrenous smell, be discolored, and may eventually produce more pus.
In order to eliminate this problem, it is imperative to apply antiseptics at once. Hydrogen peroxide (a near-universal toxin) is not recommended for this task as it increases inflammation and impedes healing.[8] Dressings with cadexomer iodine, silver, or honey have been shown to penetrate bacterial biofilms. Systemic antibiotics are not recommended in treating local infection in a pressure ulcer, as it can lead to bacterial resistance. They are only recommended if there is evidence of advancing cellulitis, bony infection, or bacteria in the blood.[9]
Diagnosis
Classification
The definitions of the four pressure ulcer stages are revised periodically by the National Pressure Ulcer Advisor Panel (NPUAP)[10] in the United States and the European Pressure Ulcer Advisor Panel (EPUAP) in Europe.[11] Briefly, they are as follows:[12][13]
- Stage I: Intact skin with non-blanchable redness of a localized area usually over a bony prominence. Darkly pigmented skin may not have visible blanching; its color may differ from the surrounding area. The area differs in characteristics such as thickness and temperature as compared to adjacent tissue. Stage 1 may be difficult to detect in individuals with dark skin tones. May indicate "at risk" persons (a heralding sign of risk).
- Stage II: Partial thickness loss of dermis presenting as a shallow open ulcer with a red pink wound bed, without slough. May also present as an intact or open/ruptured serum-filled blister. Presents as a shiny or dry shallow ulcer without slough or bruising. This stage should not be used to describe skin tears, tape burns, perineal dermatitis, maceration or excoriation.
- Stage III: Full thickness tissue loss. Subcutaneous fat may be visible but bone, tendon or muscle are not exposed. Slough may be present but does not obscure the depth of tissue loss. May include undermining and tunneling. The depth of a stage 3 pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have (adipose) subcutaneous tissue and stage 3 ulcers can be shallow. In contrast, areas of significant adiposity can develop extremely deep stage 3 pressure ulcers. Bone/tendon is not visible or directly palpable.
- Stage IV: Full thickness tissue loss with exposed bone, tendon or muscle. Slough or eschar may be present on some parts of the wound bed. Often include undermining and tunneling. The depth of a stage 4 pressure ulcer varies by anatomical location. The bridge of the nose, ear, occiput and malleolus do not have (adipose) subcutaneous tissue and these ulcers can be shallow. Stage 4 ulcers can extend into muscle and/or supporting structures (e.g., fascia, tendon or joint capsule) making osteomyelitis likely to occur. Exposed bone/tendon is visible or directly palpable. In 2012, the NPUAP stated that pressure ulcers with exposed cartilage are also classified as a stage 4.
- Unstageable: Full thickness tissue loss in which actual depth of the ulcer is completely obscured by slough (yellow, tan, gray, green or brown) and/or eschar (tan, brown or black) in the wound bed. Until enough slough and/or eschar is removed to expose the base of the wound, the true depth, and therefore stage, cannot be determined. Stable (dry, adherent, intact without erythema or fluctuance) eschar on the heels is normally protective and should not be removed.
- Suspected Deep Tissue Injury: A purple or maroon localized area of discolored intact skin or blood-filled blister due to damage of underlying soft tissue from pressure and/or shear. The area may be preceded by tissue that is painful, firm, mushy, boggy, warmer or cooler as compared to adjacent tissue. A deep tissue injury may be difficult to detect in individuals with dark skin tones. Evolution may include a thin blister over a dark wound bed. The wound may further evolve and become covered by thin eschar. Evolution may be rapid exposing additional layers of tissue even with optimal treatment.
Prevention
In the United Kingdom, the Royal College of Nursing has published guidelines in 'Pressure ulcer risk assessment and prevention' that call for identifying people at risk and taking preventative action;[14] the UK National Standards for Care Homes (UK) to do so as well.[15]
Internationally, the NPUAP, EPUAP and Pan Pacific Pressure Injury Alliance (Australia, New Zealand, Singapore and Hong Kong) published comprehensive evidence-based clinical practice guidelines[16] in 2014.[17] The guideline was developed by an international team of over 100 clinical specialists and updates the 2009 EPUAP and NPUAP clinical guidelines. The guideline includes recommendations on strategies to prevent pressure ulcers including the use of pressure redistributing support surfaces, repositioning and maintaining appropriate nutritional support.
Redistributing pressure
The most important care for a person at risk for pressure ulcers and those with bedsores is the redistribution of pressure so that no pressure is applied to the pressure ulcer.[18] In the 1940s Ludwig Guttmann introduced a program of turning paraplegics every two hours thus allowing bedsores to heal. Previously such individuals had a two-year life-expectancy, normally succumbing to blood and skin infections. Guttmann had learned the technique from the work of Boston physician Donald Munro.[19]
Nursing homes and hospitals usually set programs in place to avoid the development of pressure ulcers in those who are bedridden, such as using a routine time frame for turning and repositioning to reduce pressure. The frequency of turning and repositioning depends on the person's level of risk.
Support surfaces
A 2015 Cochrane review found that people who lay on high specification or high density foam mattresses were 60% less likely to develop new pressure ulcers compared to regular foam mattresses. Sheepskin overlays on top of mattresses were also found to prevent new pressure ulcer formation.[1] There is unclear research on the effectiveness of alternating pressure mattresses. Pressure-redistributive mattresses are used to reduce high values of pressure on prominent or bony areas of the body. There are several important terms used to describe how these support surfaces work. These terms were standardized through the Support Surface Standards Initiative of the NPUAP.[20] Many support surfaces redistribute pressure by immersing and/or enveloping the body into the surface. Some support surfaces, including antidecubitus mattresses and cushions, contain multiple air chambers that are alternately pumped.[21][22] Methods to standardize the products and evaluate the efficacy of these products have only been developed in recent years through the work of the S3I within NPUAP.[23] For individuals with paralysis, pressure shifting on a regular basis and using a wheelchair cushion featuring pressure relief components can help prevent pressure wounds.
Controlling the heat and moisture levels of the skin surface, known as skin microclimate management, also plays a significant role in the prevention and control of pressure ulcers.[24]
Nutrition
In addition, adequate intake of protein and calories is important. vitamin C has been shown to reduce the risk of pressure ulcers. People with higher intakes of vitamin C have a lower frequency of bed sores in those who are bedridden than those with lower intakes. Maintaining proper nutrition in newborns is also important in preventing pressure ulcers. If unable to maintain proper nutrition through protein and calorie intake, it is advised to use supplements to support the proper nutrition levels.[25] Skin care is also important because damaged skin does not tolerate pressure. However, skin that is damaged by exposure to urine or stool is not considered a pressure ulcer. These skin wounds should be classified as Incontinence Associated Dermatitis.
Treatment
Internationally, the NPUAP, EPUAP and Pan Pacific Pressure Injury Alliance (Australia, New Zealand, Singapore and Hong Kong) published updated evidence-based clinical practice guidelines[16] in 2014.[17] The guideline was developed by an international team of over 100 clinical specialists and updates the 2009 EPUAP and NPUAP clinical guidelines. The guideline includes recommendations on strategies to treat pressure ulcers, including the use of bed rest, pressure redistributing support surfaces, nutritional support, repositioning, wound care (e.g. debridement, wound dressings) and biophysical agents (e.g. electrical stimulation).[26] Reliable scientific evidence to support the use of many of these interventions, though, is lacking. More research is needed to assess how to best support the treatment of pressure ulcers, for example by repositioning.[27][28][29][30] Also, the benefit of using systemic or topical antibiotics in the management of pressure ulcer is still unclear.[31] A 2017 Cochrane review found that it was unclear whether one topical agent or dressing was better than another for treating pressure ulcers. Protease-modulating dressings, foam dressings or collagenase ointment may be better at healing than gauze.[32]
Debridement
Necrotic tissue should be removed in most pressure ulcers. The heel is an exception in many cases when the limb has an inadequate blood supply. Necrotic tissue is an ideal area for bacterial growth, which has the ability to greatly compromise wound healing. There are five ways to remove necrotic tissue.
- Autolytic debridement is the use of moist dressings to promote autolysis with the body's own enzymes and white blood cells. It is a slow process, but mostly painless, and is most effective in individuals with a properly functioning immune system.
- Biological debridement, or maggot debridement therapy, is the use of medical maggots to feed on necrotic tissue and therefore clean the wound of excess bacteria. Although this fell out of favor for many years, in January 2004, the FDA approved maggots as a live medical device.[33]
- Chemical debridement, or enzymatic debridement, is the use of prescribed enzymes that promote the removal of necrotic tissue.
- Mechanical debridement, is the use of debriding dressings, whirlpool or ultrasound for slough in a stable wound
- Surgical debridement, or sharp debridement, is the fastest method, as it allows a surgeon to quickly remove dead tissue.
Dressing
Some guidelines for dressing are:[34]
| Condition | Cover dressing |
|---|---|
| None to moderate exudates | Gauze with tape or composite |
| Moderate to heavy exudates | Foam dressing with tape or composite |
| Frequent soiling | Hydrocolloid dressing, film or composite |
| Fragile skin | Stretch gauze or stretch net |
Epidemiology
Pressure ulcers resulted in 29,000 deaths worldwide in 2013 up from 14,000 deaths in 1990.[2]
Each year, more than 2.5 million people in the United States develop pressure ulcers.[35] In acute care settings in the United States, the incidence of bedsores is 0.4% to 38%; within long-term care it is 2.2% to 23.9%, and in home care, it is 0% to 17%. Similarly, there is wide variation in prevalence: 10% to 18% in acute care, 2.3% to 28% in long-term care, and 0% to 29% in home care. There is a much higher rate of bedsores in intensive care units because of immunocompromised individuals, with 8% to 40% of those in the ICU developing bedsores.[36] However, pressure ulcer prevalence is highly dependent on the methodology used to collect the data. Using the European Pressure Ulcer Advisory Panel (EPUAP) methodology there are similar figures for pressure ulcers in acutely sick people in the hospital. There are differences across countries, but using this methodology pressure ulcer prevalence in Europe was consistently high, from 8.3% (Italy) to 22.9% (Sweden).[37] A recent study in Jordan also showed a figure in this range.[38] Some research shows differences in pressure-ulcer detection among white and black residents in nursing homes.[39]
References
- 1 2 McInnes, Elizabeth; Jammali-Blasi, Asmara; Bell-Syer, Sally E. M.; Dumville, Jo C.; Middleton, Victoria; Cullum, Nicky (2015-09-03). "Support surfaces for pressure ulcer prevention". The Cochrane Database of Systematic Reviews (9): CD001735. doi:10.1002/14651858.CD001735.pub5. ISSN 1469-493X. PMID 26333288.
- 1 2 GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385: 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- ↑ Grey, Joseph E; Harding, Keith G; Enoch, Stuart (2006-02-25). "Pressure ulcers". BMJ : British Medical Journal. 332 (7539): 472–475. doi:10.1136/bmj.332.7539.472. ISSN 0959-8138. PMC 1382548. PMID 16497764.
- 1 2 Lyder, Courtney H. (2003-01-08). "Pressure Ulcer Prevention and Management". JAMA. 289 (2). doi:10.1001/jama.289.2.223. ISSN 0098-7484.
- ↑ Berlowitz, D. R.; Wilking, S. V. (November 1989). "Risk factors for pressure sores. A comparison of cross-sectional and cohort-derived data". Journal of the American Geriatrics Society. 37 (11): 1043–1050. doi:10.1111/j.1532-5415.1989.tb06918.x. ISSN 0002-8614. PMID 2809051.
- ↑ Ebersole & Hess' Toward Healthy Aging. Missouri: Mosby. 2012.
- ↑ Bhat, Sriram (2013). Srb's Manual of Surgery, 4e. Jaypee Brother Medical Pub. p. 21. ISBN 9789350259443.
- ↑ "Dealing with Pressure Sores".
- ↑ American Family Physician. "Pressure Ulcers: Prevention, Evaluation, and Management". Retrieved 8 June 2012.
- ↑ "National Pressure Ulcer Advisory Panel (NPUAP)".
- ↑ "EPUAP – European Pressure Ulcer Advisory Panel".
- ↑ Edsberg, Laura E.; Black, Joyce M.; Goldberg, Margaret; McNichol, Laurie; Moore, Lynn; Sieggreen, Mary (2016). "Revised National Pressure Ulcer Advisory Panel Pressure Injury Staging System". Journal of Wound, Ostomy, and Continence Nursing. 43 (6): 585–597. doi:10.1097/WON.0000000000000281. ISSN 1071-5754. PMC 5098472. PMID 27749790.
- ↑ (U.S.), National Pressure Ulcer Advisory Panel. Prevention and treatment of pressure ulcers. Quick reference guide. Haesler, Emily., European Pressure Ulcer Advisory Panel., Pan Pacific Pressure Injury Alliance. (Second ed.). Perth, Western Australia. ISBN 9780957934368. OCLC 945954574.
- ↑ http://www.rcn.org.uk/__data/assets/pdf_file/0003/78501/001252.pdf
- ↑ Pressure Relief and Wound Care Independent Living (UK)
- 1 2 National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Clinical Practice Guideline. Emily Haesler (Ed.). Cambridge Media: Osborne Park, Western Australia; 2014.
- 1 2 "International Pressure Ulcer Clinical Practice Guideline".
- ↑ Reilly EF, Karakousis GC, Schrag SP, Stawicki SP (2007). "Pressure ulcers in the intensive care unit: The 'forgotten' enemy". OPUS 12 Scientist. 1 (2): 17–30.
- ↑ D.Whitteridge, ‘Guttmann, Sir Ludwig (1899–1980)’, rev. Oxford Dictionary of National Biography, Oxford University Press, 2004; online edn, May 2012
- ↑ See S3I at npuap.org
- ↑ Guy H (2004). "Preventing pressure ulcers: choosing a mattress". Professional Nurse. 20 (4): 43–46. PMID 15624622.
- ↑ "Antidecubitus Why?" (PDF). Antidecubitus Systems Matfresses Cushions. COMETE s.a.s. Retrieved 2009-10-02.
- ↑ Bain DS, Ferguson-Pell M (2002). "Remote monitoring of sitting behavior of people with spinal cord injury". J Rehabil Res Dev. 39 (4): 513–20. PMID 17638148.
- ↑ "Archived copy". Archived from the original on 2012-12-17. Retrieved 2012-10-17.
- ↑ NICHQ. "How To Guide Pediatric Supplement – Preventing Pressure Ulcers" (PDF). Retrieved 8 June 2012.
- ↑ National Pressure Ulcer Advisory Panel, European Pressure Ulcer Advisory Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of Pressure Ulcers: Quick Reference Guide (PDF). Perth, Australia: Cambridge Media. p. 19. ISBN 978-0-9579343-6-8. Retrieved 18 October 2016.
- ↑ Moore, ZE; van Etten, MT; Dumville, JC (17 October 2016). "Bed rest for pressure ulcer healing in wheelchair users". The Cochrane Database of Systematic Reviews. 10: CD011999. doi:10.1002/14651858.CD011999.pub2. PMID 27748506.
- ↑ Langer, G; Fink, A (12 June 2014). "Nutritional interventions for preventing and treating pressure ulcers". The Cochrane Database of Systematic Reviews (6): CD003216. doi:10.1002/14651858.CD003216.pub2. PMID 24919719.
- ↑ Moore, ZE; Cowman, S (5 January 2015). "Repositioning for treating pressure ulcers". The Cochrane Database of Systematic Reviews. 1: CD006898. doi:10.1002/14651858.CD006898.pub4. PMID 25561248.
- ↑ Moore, ZE; Cowman, S (28 March 2013). "Wound cleansing for pressure ulcers". The Cochrane Database of Systematic Reviews (3): CD004983. doi:10.1002/14651858.CD004983.pub3. PMID 23543538.
- ↑ Norman, G; Dumville, JC; Moore, ZE; Tanner, J; Christie, J; Goto, S (4 April 2016). "Antibiotics and antiseptics for pressure ulcers". The Cochrane Database of Systematic Reviews. 4: CD011586. doi:10.1002/14651858.CD011586.pub2. PMID 27040598.
- ↑ Westby, Maggie J.; Dumville, Jo C.; Soares, Marta O.; Stubbs, Nikki; Norman, Gill (22 June 2017). "Dressings and topical agents for treating pressure ulcers". The Cochrane Database of Systematic Reviews. 6: CD011947. doi:10.1002/14651858.CD011947.pub2. ISSN 1469-493X. PMID 28639707.
- ↑ "510(k)s Final Decisions Rendered for January 2004: DEVICE: MEDICAL MAGGOTS". FDA.
- ↑ DeMarco, Sharon. "Wound and Pressure Ulcer Management". Johns Hopkins Medicine. Johns Hopkins University. Retrieved 2014-12-25.
- ↑ Agency for Healthcare Research and Quality. "Preventing Pressure Ulcers in Hospitals". Retrieved 8 June 2012.
- ↑ "Pressure ulcers in America: prevalence, incidence, and implications for the future. An executive summary of the National Pressure Ulcer Advisory Panel monograph". Adv Skin Wound Care. 14 (4): 208–15. 2001. doi:10.1097/00129334-200107000-00015. PMID 11902346.
- ↑ Vanderwee K; Clark M; Dealey C; Gunningberg L; Defloor T (2007). "Pressure ulcer prevalence in Europe: a pilot study". Journal of Evaluation in Clinical Practice. 13 (2): 227–35. doi:10.1111/j.1365-2753.2006.00684.x. PMID 17378869.
- ↑ Tubaishat A, Anthony DM, Saleh M (2010). "Pressure ulcers in Jordan: A point prevalence study". Journal of Tissue Viability. 19 (4): 132–36. doi:10.1016/j.jtv.2009.11.006. PMID 20036124.
- ↑ Li Yue; Yin Jun; Cai Xueya; Temkin-Greener Jna; Mukamel Dana B (2011). "Association of Race and Sites of Care With Pressure Ulcers in High-Risk Nursing Home Residents". JAMA. 306 (2): 179–86. doi:10.1001/jama.2011.942. PMC 4108174.
Further reading
- Qaseem, Amir; Mir, Tanveer P.; Starkey, Melissa; Denberg, Thomas D. (3 March 2015). "Risk Assessment and Prevention of Pressure Ulcers: A Clinical Practice Guideline From the American College of Physicians". Annals of Internal Medicine. 162 (5): 359–69. doi:10.7326/M14-1567. PMID 25732278.
External links
| Classification | |
|---|---|
| External resources |