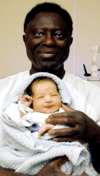
Neonatal withdrawal
| Neonatal Abstinence Syndrome | |
|---|---|
 | |
| Prematurity can accompany withdrawal | |
| Classification and external resources | |
| Specialty | pediatrics |
| ICD-10 | P96.1 |
| ICD-9-CM | 779.5 |
| DiseasesDB | 33462 |
| MedlinePlus | 007313 |
| eMedicine | ped/2760 |
| MeSH | D009357 |
Neonatal withdrawal or neonatal abstinence syndrome (NAS) is a withdrawal syndrome of infants after birth caused by in utero exposure to drugs of dependence. There are two types of NAS: prenatal and postnatal. Prenatal NAS is caused by discontinuation of drugs taken by the pregnant mother, while postnatal NAS is caused by discontinuation of drugs directly to the infant.[1][2]
Signs and symptoms
Symptoms often begin within one to three days after birth, but may take up to a week to appear. Because of this, the infant may need to stay in the hospital for observation and monitoring for up to a week. Withdrawing from different drugs, including prescribed medications, and nicotine from smoking, produces its own signs and symptoms in the infant. Neonatal abstinence syndrome may occur when a pregnant woman takes opioids such as heroin, codeine, oxycodone, methadone or buprenorphine. Benzodiazepines, barbiturates, and certain antidepressants (SSRIs) can cause dependence in the infant while in the womb.[3] The severity of the withdrawal symptoms in the neonate can be affected by the route of administration used by the mother. The metabolism and elimination of the drug from the mother's system, and the length of time that the drug was taken, will also impact the development of withdrawal symptoms in the newborn.[4] More severe findings may include acting irritable or jittery, feeding problems, and diarrhea. Symptoms vary depending on which substances were used.[3] A history of substance of abuse in the mother before the birth increases the likelihood that the infant will develop symptoms of withdrawal.
Generally, an infant going through withdrawal has a distinctive cry. It can be described as being high-pitched, non-stop and shrill. A newborn withdrawing from drugs or alcohol may be hypertonic and have convulsions. Seizures, increased Moro reflex, tremors, irritability, and disturbed sleep patterns can be observed.[4]
Respiratory symptoms of withdrawal include a temperature greater than normal, tachypnea, apnea, nasal congestion, nasal flaring, blotchy skin, and yawning.[4][3]
Withdrawal can produce gastro-intestinal symptoms such as poor appetite, regurgitation, vomiting and diarrhea. The sucking reflex can be incessant and uncoordinated.[4] Babies of mothers who use drugs of dependency throughout their pregnancies may have long-term problems.[3]
Methadone withdrawal
An infant withdrawing from methadone can have sleeping difficulties, seizures and a higher risk of dying from Sudden infant death syndrome.[4] Methadone withdrawal occurs after 7–14 days. If a child is premature they have a lower risk of severe symptoms. Those born < 35 weeks’ after gestation have lower CNS abstinence scores than term infants. It may be because preterm infants may have been exposed to less of the drug, possess an immature nervous system and lower adipose tissue.[5]
Heroin withdrawal
An infant born with heroin dependency is more likely to be premature and have meconium staining.[4] Heroin withdrawal is seen within 48–72 hours of the birth.[5]
Amphetamine withdrawal
An infant born with amphetamine dependency is more likely to be premature. It may also be small for gestational age. It may show signs of respiratory distress, infection, exaggerated startle reflex, sleep pattern disturbances. After the infant is born it may have poor weight gain, frequent infections, developmental delays and emotional problems.[4]
Alcohol withdrawal
Though the use of alcohol by the mother before birth can cause serious long-term effects in her newborn, the infant may also be born with a dependence on alcohol. Alcohol withdrawal in a newborn produces seizures, increased muscle tone, exaggerated startle reflex, irritability and jitteriness.[6]
Marijuana withdrawal
Withdrawal from marijuana can initiate a preterm birth and meconium staining.[4]
Lysergic acid diethylamide (LSD)
LSD use by the mother produces symptoms. Since polydrug abuse often accompanies the use of LSD the symptoms may be masked. Abnormal feeding, tremors and hypertonia can be seen in the infant.[5] Withdrawal symptoms manifest as hypertonia, tremors, poor feeding, and abnormal feeding patterns.
Caffeine and nicotine
Symptoms of nicotine withdrawal can become apparent as long as five days after delivery and last for months. The symptoms of nicotine withdrawal in the infant are excitability and hypertonicity. Vomiting, excessive crying and sleep difficulties can be seen in infants withdrawing from caffeine.[5]
Causes
The drugs involved may be, for example, opioids, selective serotonin reuptake inhibitors (SSRIs), ethanol and benzodiazepines.[3] Neonatal abstinence syndrome does not happen in prenatal cocaine exposure. Prematurity and exposure to other drugs may instead be the cause of symptoms.[7]
Mechanisms
Drugs and chemicals pass through the placenta that connects the baby to its mother in the womb. The baby becomes dependent on the drug along with the mother. If the mother continues to use the drugs within the week or so before delivery, the baby will be dependent on the drug at birth. Because the baby is no longer getting the drug after birth, withdrawal symptoms may occur as the drug is slowly cleared from the baby's system.[3] Nicotine, medications and alcohol have side effects related to unsafe higher dosages, but neonates may respond differently. Newborns are less able to metabolize drugs and therefore the substance stays in their system for a relatively longer length of time when compared to those who are older and have fully functioning livers and kidneys.[8]
Diagnosis
Confirming the presence of withdrawal in the neonate can be assessed from obtained a detailed medical history from the mother. In some cases neonatal drug withdrawal can be mistaken for central nervous system disorders.[5] Typically the tests that are ordered are CBC, hair analysis, drug screen (of mother and infant), thyroid levels, electrolytes, and blood glucose. Chest x-rays can confirm or infirm the presence of heart defects.[6][3] The diagnosis for babies with signs of withdrawal may be confirmed with drug tests of the baby's urine or stool. The mother's urine will also be tested.[3]
There are at least two different scoring systems for neonatal withdrawal syndrome. One difficulty with both is that were developed to assess opiate withdrawal. The Finnegan scoring system is more widely used.[5]
Prevention
Neonatal withdrawal is prevented by the mother abstaining from substance abuse. In some cases, a prescribed medication may have to be discontinued during the pregnancy to prevent addiction by the baby. Early pre-natal care can identify addictive behaviors in the mother and family system. Referrals to treatment centers is appropriate.[6] Some prescribed medicines should not be stopped without medical supervision, or harm may result. Women can discuss all medicines, and alcohol and tobacco use with their health care provider and get assistance to help stop drug use as soon as possible. Indications that a woman needs help if she is:
- Using drugs non-medically
- Using drugs not prescribed to her
- Using alcohol or tobacco[3]
If she is already pregnant and takes medicines or drugs not prescribed to her, she can talk to a health care provider about the best way to keep to keep the baby safe. Some medicines should not be stopped without medical supervision, or harm may result. Your health care provider will know how best to manage the risks.[3]
Treatment
Treatment depends on the drug involved, the infant's overall health, abstinence scores and whether the baby was born full-term or premature. Clinicians will watch the newborn carefully for up to a week after birth for signs of withdrawal, feeding problems, and weight gain. Babies who vomit or who are very dehydrated may need to get fluids through a vein (IV).
Some babies with severe symptoms need medicines such as methadone and morphine to treat withdrawal symptoms. These babies may need to stay in the hospital for weeks or months after birth. The goal of treatment is to prescribe the infant a drug similar to the one the mother used during pregnancy and slowly decrease the dose over time. This helps wean the baby off the drug and relieves some withdrawal symptoms.
If the symptoms are severe, especially if other drugs were used, a second medicine such as phenobarbital or clonidine may be added. Breastfeeding may also be helpful if the mother is in a methadone or buprenorphine treatment program without other drug use.
Babies with this condition often have severe diaper rash or other areas of skin breakdown. This requires treatment with special ointment or cream. Babies may also have problems with feeding or slow growth. These problems may require higher-calorie feedings that provide greater nutrition and smaller portions given more often.[3] Objectives of management are to minimize negative outcomes and promote normal development.[9]
Supportive
Non-medication based approaches to treat neonatal symptoms include swaddling the infant in a blanket, minimizing environmental stimuli, and monitoring sleeping and feeding patterns.[3] Breastfeeding promotes infant attachment and bonding and is associated with a decreased need for medication. These approaches may lessen the severity of NAS and lead to shorter hospital stays.[10]
Medication
Medication is used to relieve fever, seizures, and weight loss or dehydration.[9] When medication is use for opiate withdrawal in newborn babies is deemed necessary, opiates are the treatment of choice; they are slowly tapered down to wean the baby off opiates.[11] Phenobarbital is sometimes used as an alternative but is less effective in suppressing seizures; however, phenobarbital is superior to diazepam for neonatal opiate withdrawal symptoms. In the case of sedative-hypnotic neonatal withdrawal, phenobarbital is the treatment of choice.[12][13] Clonidine is an emerging add-on therapy.[14]
Opioids such as neonatal morphine solution and methadone are commonly used to treat clinical symptoms of opiate withdrawal, but may prolong neonatal drug exposure and duration of hospitalization.[15] A study demonstrated a shorter wean duration in infants treated with methadone compared to those treated with diluted tincture of opium. When compared to morphine, methadone has a longer half-life in children, which allows for less frequent dosing intervals and steady serum concentrations to prevent neonatal withdrawal symptoms.[16]
Epidemiology
A 2012 study from the University of Michigan and the University of Pittsburgh published in the Journal of the American Medical Association analyzed information on 7.4 million discharges from 4,121 hospitals in 44 states, to measure trends and costs associated with NAS over the past decade. The study indicated that between 2000 and 2009, the number of mothers using opiates increased from 1.19 to 5.63 per 1,000 hospital births per year. Newborns with NAS were 19% more likely than all other hospital births to have low birthweight and 30% more like to have respiratory complications. Between 2000 and 2009, total hospital charges for NAS cases, adjusted for inflation, are estimated to have increased from $190 million to $720 million.[17]
Neonatal abstinence syndrome in Canada are significant.[18][19]
Complications
Drug and alcohol use during pregnancy can lead to many health problems in the baby besides NAS. These may include:
- Birth defects
- Low birth weight
- Premature birth
- Small head circumference
- Sudden infant death syndrome (SIDS)
- Problems with development and behavior
Neonatal abstinence syndrome treatment can last from 1 week to 6 months. Even after medical treatment for NAS is over and babies leave the hospital, they may need continued treatment for weeks or months.[3]
References
- ↑ Neonatal Abstinence Syndrome on eMedicine
- ↑ Hall, RW.; Boyle, E.; Young, T. (Oct 2007). "Do ventilated neonates require pain management?". Semin Perinatol. 31 (5): 289–97. doi:10.1053/j.semperi.2007.07.002. PMID 17905183.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 "Neonatal abstinence Syndrome". MedlinePlus. US Library of Medicine. 5 July 2017. Retrieved 27 July 2017.

- 1 2 3 4 5 6 7 8 Henry, p. 183.
- 1 2 3 4 5 6 "Neonatal Abstinence Syndrome Clinical Presentations". Medscape. 27 November 2016. Retrieved 28 July 2017.
- 1 2 3 Henry, p. 184.
- ↑ Mercer, J (2009). "Claim 9: "Crack babies" can't be cured and will always have serious problems". Child Development: Myths and Misunderstandings. Thousand Oaks, Calif: Sage Publications, Inc. pp. 62–64. ISBN 1-4129-5646-3.
- ↑ Hamdan, Ashraf (December 20, 2017). "Neonatal Abstinence Syndrome". Medscape. Archived from the original on September 14, 2017. Retrieved July 25, 2018.
- 1 2 Longo, Dan L.; McQueen, Karen; Murphy-Oikonen, Jodie (22 December 2016). "Neonatal Abstinence Syndrome". New England Journal of Medicine. 375 (25): 2468–2479. doi:10.1056/NEJMra1600879.
- ↑ Pritham, Ursula A.; Paul, Jonathan A.; Hayes, Marie J. (March 2012). "Opioid Dependency in Pregnancy and Length of Stay for Neonatal Abstinence Syndrome". Journal of Obstetric, Gynecologic, & Neonatal Nursing. 41 (2): 180–190. doi:10.1111/j.1552-6909.2011.01330.x. PMC 3407283. PMID 22375882.
- ↑ Hudak, ML; Tan, R. C. (30 January 2012). "Neonatal Drug Withdrawal". Pediatrics. 129 (2): e540–e560. doi:10.1542/peds.2011-3212. PMID 22291123.
- ↑ Osborn, DA; Jeffery, HE; Cole, M (2010). Osborn, David A, ed. "Opiate treatment for opiate withdrawal in newborn infants". Cochrane Database Syst Rev (3): CD002059. doi:10.1002/14651858.CD002059.pub3. PMID 20927730.
- ↑ Osborn, DA; Jeffery, HE; Cole, MJ (2010). Osborn, David A, ed. "Sedatives for opiate withdrawal in newborn infants". Cochrane Database Syst Rev (3): CD002053. doi:10.1002/14651858.CD002053.pub3. PMID 20927729.
- ↑ Kraft, WK; van den Anker, JN (Oct 2012). "Pharmacologic management of the opioid neonatal abstinence syndrome". Pediatric clinics of North America. 59 (5): 1147–65. doi:10.1016/j.pcl.2012.07.006. PMC 4709246. PMID 23036249.
- ↑ Logan, Beth A.; Brown, Mark S.; Hayes, Marie J. (March 2013). "Neonatal Abstinence Syndrome: Treatment and Pediatric Outcomes". Clinical Obstetrics and Gynecology. 56 (1): 186–192. doi:10.1097/GRF.0b013e31827feea4. PMC 3589586. PMID 23314720.
- ↑ Johnson, Melissa R.; Nash, David R.; Martinez, Michael A. (July 2014). "Development and Implementation of a Pharmacist-Managed, Neonatal and Pediatric, Opioid-Weaning Protocol". The Journal of Pediatric Pharmacology and Therapeutics. 19 (3): 165–173. doi:10.5863/1551-6776-19.3.165. PMC 4187529. PMID 25309146.
- ↑ Patrick, SW; Schumacher, RE; Benneyworth, BD; Krans, EE; McAllister, JM; Davis, MM (May 9, 2012). "Neonatal abstinence syndrome and associated health care expenditures: United States, 2000-2009". JAMA: The Journal of the American Medical Association. 307 (18): 1934–40. doi:10.1001/jama.2012.3951. PMID 22546608.
- ↑ Dow, Ordean (2012). "Neonatal Abstinence syndrome clinical practice guidelines for Ontatio" (PDF). Journal of Population Therapeutics and Clinical Pharmacology. 19: 488–506.
- ↑ Leslie, K (2015). "Officials can't explain increase in North Bay babies born to addicted moms". CTV News.
Bibliography
Henry, Norma (2016). RN Maternal Newborn Nursing. Stilwell, KS: Assessment Technologies Institute. ISBN 9781565335691.