Sprain
| Sprain | |
|---|---|
 | |
| A sprained ankle with bruising. | |
| Classification and external resources | |
| Specialty | Sports medicine |
| ICD-10 | T14.3 |
| ICD-9-CM | 848.9 |
| MedlinePlus | 000041 |
| MeSH | D013180 |
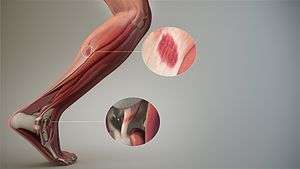
A sprain, also known as a torn ligament, is damage to one or more ligaments in a joint, often caused by trauma or the joint being taken beyond its functional range of motion. The severity of sprain ranges from a minor injury which resolves in a few days to a major rupture of one or more ligaments requiring surgical fixation and a period of immobilization. Sprains can occur in any joint but are most common in the ankle and wrist.[1]
Signs and symptoms
Causes
Sprains typically occur when the joint is taken beyond its functional range of motion.
There are certain factors which increase risk of sprains. Fatigue of muscles generally leads to sprains. When one suddenly starts to exercise after a sedentary lifestyle, sprains are quite common. While scientific studies are lacking, it is often thought that not 'warming up' is a common cause of sprains in athletes . 'Warming up' is thought to loosen the joint, increasing blood flow and making the joint more flexible .
Diagnosis
A diagnosis of a sprain can often be made with a good degree of certainty by physical examination based on the clinical presentation and method of injury. In some cases, X-rays are obtained to ensure that there is no fracture. In some cases, particularly if the injury is prolonged or does not appear to be resolving as expected, magnetic resonance imaging (MRI) is performed to look at surrounding soft tissues and the ligament.[2]
Classification
- First degree sprain (mild) – the fibres of the ligament are stretched but intact.
- Second degree sprain (moderate) – is a tear of part of a ligament, from a third to almost all its fibres.
- Third degree sprain (severe)– is a complete rupture of the ligament, sometimes avulsing a piece of bone.
Joints involved
Although any joint can experience a sprain, some of the more common include:
- The ankle. It is the most common, and has been said that sprains such as serious ankle sprains are more painful and take longer to heal than actually breaking the bones in that area.[3] See sprained ankle for more details.
- The knee. One of the more talked about sprains is that to the anterior cruciate ligament (ACL) of the knee. This is a disabling sprain common to athletes, especially in American football, football (soccer), basketball, pole vaulting, softball, baseball and some styles of martial arts. See Anterior cruciate ligament injury.
- Ligaments between the spinal vertebrae
- The fingers.
- The wrist.
- The toes.
Treatment
The first modality for a sprain can be remembered using the acronym RICE.[4] The treatment of sprains depends on the extent of injury and the joint involved. Medications like non-steroidal anti-inflammatory drugs can relieve pain. Topical NSAIDs appear to be as good as those taken by mouth.[5]
- Rest: The sprain should be rested. No additional force should be applied on site of the sprain. In case of, for example, a sprained ankle, walking should be kept to a minimum.[6]
- Ice: Ice should be applied immediately to the sprain to reduce swelling and pain. It can be applied for 10–15 minutes at a time (longer application of ice may cause damage instead of healing), 3-4 times a day. Ice can be combined with a wrapping to minimize swelling and provide support.[6]
- Compression: Dressings, bandages, or ace-wraps should be used to immobilize the sprain and provide support. When wrapping the injury, more pressure should be applied at the far end of the injury and decrease in the direction of the heart; the reason for this is that it more easily causes unnecessary fluid to be flushed back up the blood stream in order to be recycled. Compression should not cut off the circulation of the limb.[6]
- Elevation: Keeping the sprained joint elevated (in relation to the rest of the body) will also help minimize swelling.[6]
Ice and compression (cold compression therapy) will not completely stop swelling and pain, but will help to minimize them as the sprain begins to heal itself. Careful management of swelling is critical to the healing process as additional fluid may pool in the sprained area.
The joint should be exercised again fairly soon, in milder cases from 1 to 3 days after injury.[7] Special exercises are sometimes needed in order to regain strength and help reduce the risk of ongoing problems. The joint may need to be supported by taping or bracing, helping protect it from re-injury.[7]
Functional rehabilitation
Prolonged immobilization delays the healing of a sprain, as it usually leads to muscle atrophy and stiff joint. The components of an effective rehabilitation for all sprain injuries include increasing range of motion and progressive muscle strengthening exercise. These should be taken care of without delay.[8]
References
- ↑ Retrieved on 2010-02-16
- ↑ Strains and sprains information Mayo Clinic. Retrieved on 2010-01-26
- ↑ Holes Human Anatomy & Physiology, Shier, David, Jackie Butler, Ricki Lewis, McGraw Hill 2007, Eleventh Ed., p.157,160
- ↑ MedicalMnemonics.com: 235
- ↑ Derry, S; Moore, RA; Gaskell, H; McIntyre, M; Wiffen, PJ (11 June 2015). "Topical NSAIDs for acute musculoskeletal pain in adults". The Cochrane Database of Systematic Reviews. 6: CD007402. doi:10.1002/14651858.CD007402.pub3. PMID 26068955.
- 1 2 3 4 "Sprained Ankle". American Orthopedic Foot and Ankle Society. March 2005. Retrieved 2008-04-01.
- 1 2 Ankle Sprains: Healing and Preventing Injury Written by familydoctor.org editorial staff. American Academy of Family Physicians. Reviewed/Updated: 08/06. Created: 01/96
- ↑ Sprained ankle American academy of orthopedic surgeons. Retrieved on 2010-01-26
External links
- Questions and Answers about Sprains and Strains - US National Institute of Arthritis and Musculoskeletal and Skin Diseases