HeLa

_%2C_vimentin_(red)_and_DNA_(blue).jpg)
HeLa /ˈhiːlɑː/ (also Hela or hela) is an immortal cell line used in scientific research. It is the oldest and most commonly used human cell line.[1] The line was derived from cervical cancer cells taken on February 8, 1951[2] from Henrietta Lacks, a patient who died of cancer on October 4, 1951. The cell line was found to be remarkably durable and prolific which warrants its extensive use in scientific research.[3][4]
The cells from Lacks's cancerous cervical tumor were taken without her knowledge or consent.[5] Cell biologist George Otto Gey found that they could be kept alive,[6] and isolated one specific cell, multiplied it, and developed a cell line. (Before this, cells cultured from other human cells would only survive for a few days; scientists spent more time trying to keep the cells alive than performing actual research on them. Cells from Lacks's tumor behaved differently.) As was custom for Gey's lab assistant, she labeled the culture 'HeLa', the first two letters of the patient's first and last name; this became the name of the cell line.
These were the first human cells grown in a lab that were naturally "immortal", meaning that they do not die after a set number of cell divisions (i.e. cellular senescence).[7] These cells could be used for conducting a multitude of medical experiments — if the cells died, they could simply be discarded and the experiment attempted again on fresh cells from the culture. This represented an enormous boon to medical and biological research, as previously stocks of living cells were limited and took significant effort to culture.[4]
The stable growth of HeLa enabled a researcher at the University of Minnesota hospital to successfully grow polio virus, enabling the development of a vaccine,[8] and by 1952, Jonas Salk developed a vaccine for polio using these cells.[4][9] To test Salk's new vaccine, the cells were put into mass production in the first-ever cell production factory.[10]
In 1953, HeLa cells were the first human cells successfully cloned[11] and demand for the HeLa cells quickly grew in the nascent biomedical industry. Since the cells' first mass replications, they have been used by scientists in various types of investigations including disease research, gene mapping, effects of toxic substances on organisms, and radiation on humans.[9] Additionally, HeLa cells have been used to test human sensitivity to tape, glue, cosmetics, and many other products.[4]
Scientists have grown an estimated 50 tons of HeLa cells,[4][12] and there are almost 11,000 patents involving these cells.[4]
The HeLa cell lines are also notorious for invading other cell cultures in laboratory settings.[13] Some have estimated that HeLa cells have contaminated 10-20% of all cell lines currently in use.[14]
History
Origin
The cells were propagated by George Otto Gey shortly before Lacks died of her cancer in 1951. This was the first human cell line to prove successful in vitro, which was a scientific achievement with profound future benefit to medical research. Gey freely donated these cells along with the tools and processes that his lab developed to any scientist requesting them simply for the benefit of science. Neither Lacks nor her family gave permission to harvest the cells but, at that time, permission was neither required nor customarily sought.[15] The cells were later commercialized, although never patented in their original form. There was no requirement at that time (or at present) to inform patients or their relatives about such matters because discarded material or material obtained during surgery, diagnosis, or therapy was the property of the physician or the medical institution. This issue and Lacks' situation were brought up in the Supreme Court of California case of Moore v. Regents of the University of California. The court ruled that a person's discarded tissue and cells are not his or her property and can be commercialized.[16]
At first, the HeLa cell line was said to be named after a "Helen Lane" or "Helen Larson.”[4][17] Starting in the 1970s the Lacks family was contacted by researchers trying to find out why the HeLa cells had contaminated other cell lines in laboratories.[18] These cells are treated as cancer cells, as they are descended from a biopsy taken from a visible lesion on the cervix as part of Lacks' diagnosis of cancer.[19]
HeLa cells, like other cell lines, are termed "immortal" in that they can divide an unlimited number of times in a laboratory cell culture plate as long as fundamental cell survival conditions are met (i.e., being maintained and sustained in a suitable environment). There are many strains of HeLa cells as they continue to mutate in cell cultures, but all HeLa cells are descended from the same tumor cells removed from Lacks. The total number of HeLa cells that have been propagated in cell culture far exceeds the total number of cells that were in Henrietta Lacks' body.[20]
Use in research
HeLa cells were used by Jonas Salk to test the first polio vaccine in the 1950s. They were observed to be easily infected by poliomyelitis, causing infected cells to die.[21] This made HeLa cells highly desirable for polio vaccine testing since results could be easily obtained. A large volume of HeLa cells were needed for the testing of Salk's polio vaccine, prompting the National Foundation for Infantile Paralysis (NFIP) to find a facility capable of mass-producing HeLa cells.[22] In the spring of 1953, a cell culture factory was established at Tuskegee University to supply Salk and other labs with HeLa cells.[23] Less than a year later, Salk's vaccine was ready for human trials.[24]
HeLa cells were also the first human cells to be successfully cloned in 1953 by Theodore Puck and Philip I Marcus at the University of Colorado, Denver.[11] Since that time, HeLa cells have "continually been used for research into cancer, AIDS, the effects of radiation and toxic substances, gene mapping, and countless other scientific pursuits."[9] According to author Rebecca Skloot, by 2009, "more than 60,000 scientific articles had been published about research done on HeLa, and that number was increasing steadily at a rate of more than 300 papers each month."[16]
HeLa cells have been used in testing how parvo virus infects cells of humans, HeLa, dogs, and cats.[25] These cells have also been used to study viruses such as the oropouche virus (OROV). OROV causes the disruption of cells in culture, where cells begin to degenerate shortly after they are infected, causing viral induction of apoptosis.[26] HeLa cells have been used to study the expression of the papillomavirus E2 and apoptosis.[27] HeLa cells have also been used to study canine distemper virus' ability to induce apoptosis in cancer cell lines,[28] which could play an important role in developing treatments for tumor cells resistant to radiation and chemotherapy.[28] HeLa cells have also been used in a number of cancer studies, including those involving sex steroid hormones such as estradiol, estrogen, and estrogen receptors, along with estrogen-like compounds such as quercetin and its cancer reducing properties.[29] There have also been studies on HeLa cells, the effects of flavonoids and antioxidants with estradiol on cancer cell proliferation.
HeLa cells were used to investigate the phytochemical compounds and the fundamental mechanism of the anticancer activity of the ethanolic extract of mango peel (EEMP). EEMP was found to contain various phenolic compounds and to activate death of human cervical malignant HeLa cells through apoptosis, which suggests that EEMP may help to prevent cervical cancer as well as other types of cancers.[30]
In 2011, HeLa cells were used in tests of novel heptamethine dyes IR-808 and other analogs which are currently being explored for their unique uses in medical diagnostics, the development of theranostics, the individualized treatment of cancer patients with the aid of PDT, co-administration with other drugs, and irradiation.[31][32] HeLa cells have been used in research involving fullerenes to induce apoptosis as a part of photodynamic therapy, as well as in in vitro cancer research using cell lines.[33] Further HeLa cells have also been used to define cancer markers in RNA, and have been used to establish an RNAi Based Identification System and Interference of Specific Cancer Cells.[34]
HeLa was shown in 2014 to be viable cell line for tumor xenografts in C57BL/6 nude mice,[35] and was subsequently used to examine the in vivo effects of Fluoxetine and cisplatin on cervical cancer.
Analysis
Telomerase
The HeLa cell line was derived for use in cancer research. These cells proliferate abnormally rapidly, even compared to other cancer cells. Like many other cancer cells,[36] HeLa cells have an active version of telomerase during cell division,[37] which prevents the incremental shortening of telomeres that is implicated in aging and eventual cell death. In this way, the cells circumvent the Hayflick limit, which is the limited number of cell divisions that most normal cells can undergo before becoming senescent.
Chromosome number
Horizontal gene transfer from human papillomavirus 18 (HPV18) to human cervical cells created the HeLa genome, which is different from Henrietta Lacks' genome in various ways, including its number of chromosomes. HeLa cells are rapidly dividing cancer cells, and the number of chromosomes varied during cancer formation and cell culture. The current estimate (excluding very tiny fragments) is a "hypertriploid chromosome number (3n+)" which means 76 to 80 total chromosomes (rather than the normal diploid number of 46) with 22–25 clonally abnormal chromosomes, known as HeLa signature chromosomes."[38][39][40][41] The signature chromosomes can be derived from multiple original chromosomes, making challenging summary counts based on original numbering. Researchers have also noted how stable these aberrant karyotypes can be:[38]
Human papillomaviruses (HPVs) are frequently integrated into the cellular DNA in cervical cancers. We mapped by FISH five HPV18 integration sites: three on normal chromosomes 8 at 8q24 and two on derivative chromosomes, der(5)t(5;22;8)(q11;q11q13;q24) and der(22)t(8;22)(q24;q13), which have chromosome 8q24 material. An 8q24 copy number increase was detected by CGH. Dual-color FISH with a c-MYC probe mapping to 8q24 revealed colocalization with HPV18 at all integration sites, indicating that dispersion and amplification of the c-MYC gene sequences occurred after and was most likely triggered by the viral insertion at a single integration site. Numerical and structural chromosomal aberrations identified by SKY, genomic imbalances detected by CGH, as well as FISH localization of HPV18 integration at the c-MYC locus in HeLa cells are common and representative for advanced stage cervical cell carcinomas. The HeLa genome has been remarkably stable after years of continuous cultivation; therefore, the genetic alterations detected may have been present in the primary tumor and reflect events that are relevant to the development of cervical cancer.[38]
Complete genome sequence
The complete genome of the HeLa cells was sequenced and published on 11 March 2013[39][42] without the Lacks family's knowledge.[43] Concerns were raised by the family, so the authors voluntarily withheld access to the sequence data.[43] Jay Shendure led a HeLa sequencing project at the University of Washington which produced a paper that had been accepted for publication in March 2013 — but that was also put on hold while the Lacks family's privacy concerns were being addressed.[44] On August 7, 2013, NIH director Francis Collins announced a policy of controlled access to the cell line genome based on an agreement reached after three meetings with the Lacks family.[45] A data-access committee will review requests from researchers for access to the genome sequence under the criteria that the study is for medical research and the users will abide by terms in the HeLa Genome Data Use Agreement, which includes that all NIH-funded researchers will deposit the data into a single database for future sharing. The committee consists of six members including representatives from the medical, scientific, and bioethics fields, as well as two members of the Lacks family.[45] In an interview, Collins praised the Lacks family's willingness to participate in this situation that was thrust upon them. He described the whole experience with them as "powerful", saying that it brought together "science, scientific history and ethical concerns" in a unique way.[46]
Contamination
HeLa cells are sometimes difficult to control because of their adaptation to growth in tissue culture plates. Through improper maintenance, they have been known to contaminate other cell cultures in the same laboratory, interfering with biological research and forcing researchers to declare many results invalid. The degree of HeLa cell contamination among other cell types is unknown because few researchers test the identity or purity of already established cell lines. It has been demonstrated that a substantial fraction of in vitro cell lines are contaminated with HeLa cells; estimates range from 10% to 20%. Stanley Gartler (1967) and Walter Nelson-Rees (1975) were the first to publish on the contamination of various cell lines by HeLa.[22]
Science writer Michael Gold wrote about the HeLa cell contamination problem in his book A Conspiracy of Cells. He describes Nelson-Rees's identification of this pervasive worldwide problem — affecting even the laboratories of the best physicians, scientists, and researchers, including Jonas Salk — and many possibly career-ending efforts to address it. According to Gold, the HeLa contamination problem almost led to a Cold War incident. The USSR and the USA had begun to cooperate in the war on cancer launched by President Richard Nixon, only to find that the exchanged cells were contaminated by HeLa. Gold contends that the HeLa problem was amplified by emotions, egos, and a reluctance to admit mistakes. Nelson-Rees explains:
It's all human — an unwillingness to throw away hours and hours of what was thought to be good research ... worries about jeopardizing another grant that's being applied for, the hurrying to come out with a paper first. And it isn't limited to biology and cancer research. Scientists in many endeavors all make mistakes, and they all have the same problems.[47]
Rather than focus on how to resolve the problem of HeLa cell contamination, many scientists and science writers continue to document this problem as simply a contamination issue — caused not by human error or shortcomings but by the hardiness, proliferating, or overpowering nature of HeLa.[48] Recent data suggest that cross-contaminations are still a major ongoing problem with modern cell cultures.[3][49] Taken directly from the International Cell Line Authentication Committee (ICLAC) webpage:
Regrettably, cross-contamination and misidentification are still common within the research community. Many cell lines were cross-contaminated during establishment; this means that all work using those cell lines has incorrectly used the contaminant – which may come from a different species or a different tissue. ... A cell line is considered to be misidentified if it no longer corresponds to the individual from whom it was first established. Many cases of misidentification are caused by cross-contamination, where another, faster growing, cell line is introduced into that culture.[50]
New species proposal
| HeLa cells | |
|---|---|
| Scientific classification | |
| Kingdom: | incertae sedis |
| Phylum: | incertae sedis |
| Class: | incertae sedis |
| Order: | incertae sedis |
| Family: | Helacytidae |
| Genus: | Helacyton |
| Species: | H. gartleri |
| Binomial name | |
| Helacyton gartleri | |
HeLa was described by Leigh Van Valen as an example of the contemporary creation of a new species, dubbed Helacyton gartleri, due to their ability to replicate indefinitely, and their non-human number of chromosomes. The species was named after Stanley M. Gartler, whom van Valen credits with discovering "the remarkable success of this species."[51] His argument for speciation depends on these points:
- The chromosomal incompatibility of HeLa cells with humans.
- The ecological niche of HeLa cells.
- Their ability to persist and expand well beyond the desires of human cultivators.
- HeLa can be defined as a species as it has its own clonal karyotype.[52]
Van Valen proposed the new family Helacytidae and the genus Helacyton, as well as proposing a new species for HeLa cells in the same paper.[53]
However, this proposal has not been taken seriously by other prominent evolutionary biologists, nor by scientists in other disciplines. Van Valen's argument of HeLa being a new species does not fulfill the criteria for an independent unicellular asexually reproducing species because of the notorious instability of HeLa's karyotype and their lack of a strict ancestral-descendant lineage.[54]
Additional images
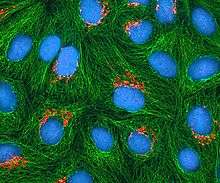
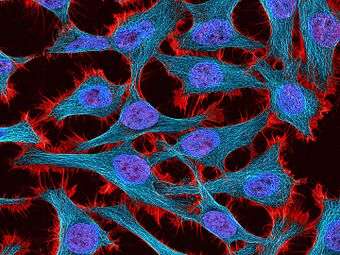 Multiphoton fluorescence image of HeLa cells stained with the actin binding toxin phalloidin (red), microtubules (cyan) and cell nuclei (blue). Nikon RTS2000MP custom laser scanning microscope.
Multiphoton fluorescence image of HeLa cells stained with the actin binding toxin phalloidin (red), microtubules (cyan) and cell nuclei (blue). Nikon RTS2000MP custom laser scanning microscope.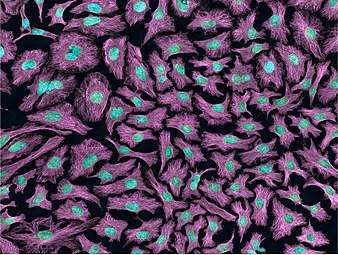 Multiphoton fluorescence image of HeLa cells with cytoskeletal microtubules (magenta) and DNA (cyan). Nikon RTS2000MP custom laser scanning microscope.
Multiphoton fluorescence image of HeLa cells with cytoskeletal microtubules (magenta) and DNA (cyan). Nikon RTS2000MP custom laser scanning microscope.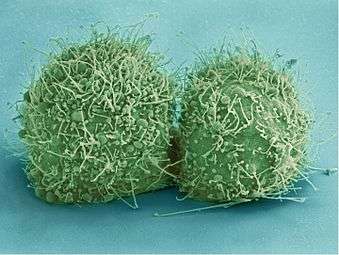 Scanning electron micrograph of just-divided HeLa cells. Zeiss Merlin HR-SEM.
Scanning electron micrograph of just-divided HeLa cells. Zeiss Merlin HR-SEM.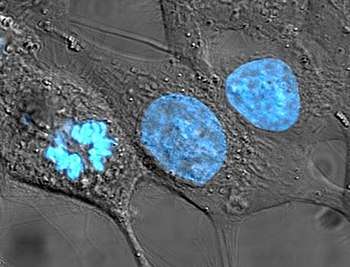 HeLa cells stained with Hoechst 33258
HeLa cells stained with Hoechst 33258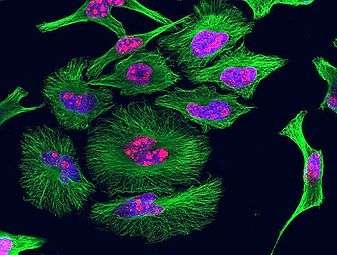 HeLa cells grown in culture and stained with antibody to tubulin (green), antibody to Ki-67 (red) and the blue DNA binding dye DAPI. The tubulin antibody shows the distribution of microtubules and the Ki-67 antibody is expressed in cells about to divide. Preparation, antibodies and image courtesy of EnCor Biotechnology.
HeLa cells grown in culture and stained with antibody to tubulin (green), antibody to Ki-67 (red) and the blue DNA binding dye DAPI. The tubulin antibody shows the distribution of microtubules and the Ki-67 antibody is expressed in cells about to divide. Preparation, antibodies and image courtesy of EnCor Biotechnology.
In print
HeLa was the subject of a book by Rebecca Skloot, The Immortal Life of Henrietta Lacks, investigating the historical context of the cell line and how the Lacks family was involved its use.[55]
In film
The 1997 documentary The Way of All Flesh by Adam Curtis explains the history of HeLa and its implications in medicine and society.[56]
The 2017 HBO film "The Immortal Life of Henrietta Lacks" starring Oprah Winfrey, Sylvia Grace Crim, Rocky Carroll & Renee Elise Goldsberry as Henrietta Lacks. The movie is based on the book, of the same name, written by Rebecca Skloot.[57]
See also
- Clonally transmissible cancer
- Moore v. Regents of the University of California, case that set precedent for discarded tissue
- List of contaminated cell lines
- WI-38
References
- ↑ Rahbari R, Sheahan T, Modes V, Collier P, Macfarlane C, Badge RM (2009). "A novel L1 retrotransposon marker for HeLa cell line identification". BioTechniques. 46 (4): 277–284. doi:10.2144/000113089. PMC 2696096. PMID 19450234.
- ↑ Scherer, W.F.; Syverton, J.T.; Gey, G.O. (1953). "Studies on the propagation in vitro of poliomyelitis viruses. IV. Viral multiplication in a stable strain of human malignant epithelial cells (strain HeLa) derived from an epidermoid carcinoma of the cervix". Journal of Experimental Medicine. 97 (5): 695–710. doi:10.1084/jem.97.5.695. PMC 2136303. PMID 13052828.
- 1 2 Capes-Davis A, Theodosopoulos G, Atkin I, Drexler HG, Kohara A, MacLeod RA, Masters JR, Nakamura Y, Reid YA, Reddel RR, Freshney RI (2010). "Check your cultures! A list of cross-contaminated or misidentified cell lines". Int. J. Cancer. 127 (1): 1–8. doi:10.1002/ijc.25242. PMID 20143388.
- 1 2 3 4 5 6 7 Batts DW (2010-05-10). "Cancer cells killed Henrietta Lacks – then made her immortal". The Virginian-Pilot. pp. 1, 12–14. Retrieved 2012-03-17. ; Note: Some sources report her birthday as August 2, 1920, vice August 1, 1920.
- ↑ Ron Claiborne; Sydney Wright, IV (2010-01-31). "How One Woman's Cells Changed Medicine". ABC World News. Retrieved 2012-08-19.
- ↑ "Henrietta Lacks's cells were priceless, but her family can't afford a hospital". The Guardian. Retrieved 18 July 2017.
- ↑
- ↑ Scherer, William F.; Syverton, Jerome T.; Gey, George O. (1953). "Studies on the Propagation in Vitro of Poliomyelitis Viruses". J Exp Med (published May 1, 1953). 97 (5): 695–710. doi:10.1084/jem.97.5.695. PMC 2136303. PMID 13052828.
- 1 2 3 Smith, Van (April 17, 2002). "Wonder Woman: The Life, Death, and Life After Death of Henrietta Lacks, Unwitting Heroine of Modern Medical Science". Baltimore City Paper. Archived from the original on August 14, 2004. Retrieved 2 March 2017.
- ↑ Skloot 2010, p. 96
- 1 2 Puck, T.T.; Marcus, P.I. (1955). "A rapid method for viable cell titration and clone production with Hela cells in tissue culture: The use of X-irradiated cells to supply conditioning factors". Proceedings of the National Academy of Sciences of the United States of America (published July 15, 1955). 41 (7): 432–437. Bibcode:1955PNAS...41..432P. doi:10.1073/pnas.41.7.432. PMC 528114. PMID 16589695.
- ↑ Margonelli, Lisa (February 5, 2010). "Eternal Life". New York Times. New York. Retrieved 23 April 2014.
- ↑ Lucey, B. P; Nelson-Rees, W. A; Hutchins, G. M (2009). "Henrietta Lacks, HeLa cells, and cell culture contamination". Archives of Pathology & Laboratory Medicine. 133 (9): 1463–7. doi:10.1043/1543-2165-133.9.1463 (inactive 2018-09-23). PMID 19722756.
- ↑
- ↑ Washington, Harriet "Henrietta Lacks: An Unsung Hero", Emerge Magazine, October 1994
- 1 2 Skloot, Rebecca (2010). The Immortal Life of Henrietta Lacks. New York: Crown/Random House. ISBN 978-1-4000-5217-2.
- ↑ Zielinski, Sarah (2010-01-02). "Cracking the code of the human genome – Henrietta Lacks' 'immortal' cells". Smithsonian. Retrieved 2017-05-27.
- ↑ Ritter, Malcolm (August 7, 2013). "Feds, family reach deal on use of DNA information". Seattle Times. Retrieved 2017-05-27.
- ↑ del Carpio, Alexandra (April 27, 2014). "The Good, the Bad, and the HeLa". Berkeley Science Review. Retrieved 2017-05-27.
- ↑ Sharrer T (2006). ""HeLa" Herself". The Scientist. 20 (7): 22.
- ↑ Scherer, W.F.; Syverton, J.T.; Gey, G.O. (1953). "Studies on the Propagation in Vitro of Poliomyelitis Viruses: Iv. Viral Multiplication in a Stable Strain of Human Malignant Epithelial Cells (Strain HeLa) Derived from an Epidermoid Carcinoma of the Cervix". Journal of Experimental Medicine. 97 (5): 695–710. doi:10.1084/jem.97.5.695. PMC 2136303. PMID 13052828.
- 1 2 Masters, John R. (2002). "HeLa cells 50 years on: The good, the bad and the ugly". Nature Reviews Cancer. 2 (4): 315–319. doi:10.1038/nrc775. PMID 12001993.
- ↑ Turner, Timothy (2012). "Development of the Polio Vaccine: A Historical Perspective of Tuskegee University's Role in Mass Production and Distribution of HeLa Cells". Journal of Health Care for the Poor and Underserved. 23 (4a): 5–10. doi:10.1353/hpu.2012.0151. PMC 4458465. PMID 23124495.
- ↑ Brownlee, K. A. (1955). "Statistics of the 1954 Polio Vaccine Trials*". Journal of the American Statistical Association. 50 (272): 1005–1013. doi:10.1080/01621459.1955.10501286.
- ↑ Parker, J; Murphy W; Wang D; O'Brien S; Parrish C (2001). "Canine and feline parvoviruses can use human or feline transferrin receptors to bind, enter, and infect cells". Journal of Virology. 75 (8): 3896–3902. doi:10.1128/JVI.75.8.3896-3902.2001. PMC 114880. PMID 11264378.
- ↑ Acrani, G.O.; Gomes, R.; Proença-Módena, J.L.; da Silva, A.F.; Carminati, P.O.; Silva, M.L.; Santos, R.I.; Arruda, E. (2010). "Apoptosis induced by Oropouche virus infection in HeLa cells is dependent on virus protein expression". Virus Research. 149 (1): 56–63. doi:10.1016/j.virusres.2009.12.013. PMID 20080135.
- ↑ Hou, S.Y.; Wu, S.; Chiang, C. (2002). "Transcriptional activity among high and low risk human papillomavirus E2 proteins correlates with E2 DNA binding". The Journal of Biological Chemistry. 277 (47): 45619–45629. doi:10.1074/jbc.M206829200. PMID 12239214.
- 1 2 del Puerto, H.L.; Martins, A.S.; Milsted, A.; Souza-Fagundes, E.M.; Braz, G.F.; Hissa, B.; Andrade, L.O.; Alves, F.; Rajão, D.S.; Leite, R.C.; Vasconcelos, A.C. (2011). "Canine distemper virus induces apoptosis in cervical tumor derived cell lines". Virol. J. 8 (1): 334. doi:10.1186/1743-422X-8-334. PMC 3141686. PMID 21718481.
- ↑ Pamela Bulzomi; Paola Galluzzo; Alessandro Bolli; Stefano Leone; Filippo Acconcia; Maria Marino (2012). "The pro-apoptotic effect of quercetin in cancer cell lines requires ERβ-dependent signals". Journal of Cellular Physiology. 227 (5): 1891–1898. doi:10.1002/jcp.22917. PMID 21732360.
- ↑ Hyeonji Kim; Hana Kim; Ashik Mosaddik; Rajendra Gyawali; Kwang Seok Ahn; Somi Kim Cho (2012). "Induction of apoptosis by ethanolic extract of mango peel and comparative analysis of the chemical consists of mango peel and flesh". Food Chemistry. 133 (2): 416–422. doi:10.1016/j.foodchem.2012.01.053. PMID 25683414.
- ↑ Tan X, Luo S, Wang D, Su Y, Cheng T, Shi C (2011). "A NIR heptamethine Dye with intrinsic cancer targeting, imaging and photosynthesizing properties". Journal of Biomaterials China. 33 (7): 2230–2239. doi:10.1016/j.biomaterials.2011.11.081. PMID 22182749.
- ↑ Pene, F.; Courtine, E.; Cariou, A.; Mira, J.P. (2009). "Toward theranostics". Crit Care Med. 37 (1 Suppl): S50–S58. doi:10.1097/CCM.0b013e3181921349. PMID 19104225.
- ↑ Briiuner., Thomas; Dieter F. Hulser (1990). "Tumor Cell Invasion and Gap Junctional Communication" (PDF). Invasion Metastasis. 10: 31–34. Retrieved 3 April 2012.
- ↑ Xie, Z.; Wroblewska, L.; Prochazka, L.; Weiss, R.; Benenson, Y. (2011). "Multi-Input RNAi-Based Logic Circuit for Identification of Specific Cancer Cells" (PDF). Science. 333 (6047): 1307–1311. Bibcode:2011Sci...333.1307X. doi:10.1126/science.1205527. PMID 21885784.
- ↑ Arjomandnejad, M; et al. (2014). "HeLa cell line xenograft tumor as a suitable cervical cancer model: growth kinetic characterization and immunohistochemistry array" (PDF). Archives of Iranian Medicine. 17 (4): 273–277.
- ↑ The Nobel Prize in Physiology or Medicine 2009 on nobelprize.org
- ↑ Ivanković M, Cukusić A, Gotić I, Skrobot N, Matijasić M, Polancec D, Rubelj I (2007). "Telomerase activity in HeLa cervical carcinoma cell line proliferation". Biogerontology. 8 (2): 163–72. doi:10.1007/s10522-006-9043-9. PMID 16955216.
- 1 2 3 Macville M, Schröck E, Padilla-Nash H, Keck C, Ghadimi BM, Zimonjic D, Popescu N, Ried T (1999). "Comprehensive and definitive molecular cytogenetic characterization of HeLa cells by spectral karyotyping". Cancer Res. 59 (1): 141–50. PMID 9892199.
- 1 2 Landry JJ, Pyl PT, Rausch T, Zichner T, Tekkedil MM, Stütz AM, Jauch A, Aiyar RS, Pau G, Delhomme N, Gagneur J, Korbel JO, Huber W, Steinmetz LM (2013). "The genomic and transcriptomic landscape of a HeLa cell line". G3: Genes, Genomes, Genetics. 3 (8): 1213–24. doi:10.1534/g3.113.005777. PMC 3737162. PMID 23550136.
- ↑ Bottomley, R.H.; Trainer, A.L.; Griffin, M.J. (1969). "Enzymatic and chromosomal characterization of HeLa variants". J. Cell Biol. 41 (3): 806–15. doi:10.1083/jcb.41.3.806. PMC 2107821. PMID 5768876.
- ↑ Andrew Adey; Joshua N. Burton; Jacob O. Kitzman; Joseph B. Hiatt; Alexandra P. Lewis; Beth K. Martin; Ruolan Qiu; Choli Lee; Jay Shendure (2013). "The haplotype-resolved genome and epigenome of the aneuploid HeLa cancer cell line". Nature (published August 8, 2013). 500 (7461): 207–211. Bibcode:2013Natur.500..207A. doi:10.1038/nature12064. PMC 3740412. PMID 23925245.
- ↑ Callaway, Ewen (March 15, 2013). "Most popular human cell in science gets sequenced". Nature. doi:10.1038/nature.2013.12609. Retrieved 8 August 2013.
- 1 2 Callaway, Ewen (March 27, 2013). "HeLa publication brews bioethical storm". Nature. doi:10.1038/nature.2013.12689. Retrieved 8 August 2013.
- ↑ Callaway, Ewen (August 7, 2013). "Deal done over HeLa cell line". Nature. 500 (7461): 132–133. Bibcode:2013Natur.500..132C. doi:10.1038/500132a. PMID 23925220. Retrieved 8 August 2013.
- 1 2 "NIH, Lacks family reach understanding to share genomic data of HeLa cells". The National Institutes of Health. August 7, 2013. Retrieved 8 August 2013.
- ↑ Callaway, Ewen (August 7, 2013). "NIH director explains HeLa agreement". Nature. doi:10.1038/nature.2013.13521.
- ↑ Gold, Michael (1986). A Conspiracy of Cells: One Woman's Immortal Legacy and the Medical Scandal It Caused. ISBN 978-0-88706-099-1.
- ↑ Wang H, Huang S, Shou J, Su EW, Onyia JE, Liao B, Li S (2006). "Comparative analysis and integrative classification of NCI60 cell lines and primary tumors using gene expression profiling data". BMC Genomics. 7 (1): 166. doi:10.1186/1471-2164-7-166. PMC 1525183. PMID 16817967.
- ↑ Nardone, R.M. (2007). "Eradication of cross-contaminated cell lines: A call for action" (PDF). Cell Biology and Toxicology. 23 (6): 367–372. CiteSeerX 10.1.1.432.8581. doi:10.1007/s10565-007-9019-9. PMID 17522957. Archived from the original (PDF) on 2008-12-17.
- ↑ "ATCC® Standards Development Organization: The International Cell Line Authentication Committee (ICLAC)". Standards.atcc.org. Retrieved 2013-06-27.
- ↑ http://www.mn.uio.no/cees/english/services/evolutionary-theory/volume-10/vol-10-no-2-pages-71-74-l-van-valen-and-v-c-mairorana-hela-a-new-microbial-species.pdf
- ↑ Duesberg, P; Mandrioli, D; McCormack, A; Nicholson, JM (2011). "Is carcinogenesis a form of speciation?". Cell Cycle. Georgetown, Texas. 10 (13): 2100–2114. doi:10.4161/cc.10.13.16352. PMID 21666415.
- ↑ van Valen, L.M.; Maiorana, V.C. (1991). "HeLa, a new microbial species". Evolutionary Theory & Review. 10: 71–74. ISSN 1528-2619.
- ↑ Cohan, FM (2002). "What are bacterial species?". Annu. Rev. Microbiol. 56 (1): 457–487. doi:10.1146/annurev.micro.56.012302.160634. PMID 12142474.
- ↑
- ↑ "Modern Times: The Way of All Flesh - BBC Two England - 19 March 1997". BBC Genome. BBC.
- ↑ "About The Immortal Life of Henrietta Lacks". Rebecca Skloot. Retrieved 24 April 2018.
Further reading
- Hannah Landecker (2000). "Immortality, In Vitro: A History of the HeLa Cell Line". In Brodwin, Paul. Biotechnology and culture: bodies, anxieties, ethics. Bloomington: Indiana University Press. pp. 53–74. ISBN 978-0-253-21428-7.
- Rebecca Skloot (2010). The Immortal Life of Henrietta Lacks.
External links
| Wikimedia Commons has media related to HeLa cells. |
- HeLa (CCL-2 Cells) in the ATCC database
- HeLa Cells at the US National Library of Medicine Medical Subject Headings (MeSH)
- HeLa Transfection and Selection Data for HeLa Cells
- Rebecca Skloot, The Immortal Life of Henrietta Lacks book website with additional features (photo/video/audio)
- The Henrietta Lacks Foundation, a foundation established to, among other things, help provide scholarship funds and health insurance to Henrietta Lacks's family.
- Rebecca Skloot, Cells That Save Lives are a Mother's Legacy, New York Times
- "Wonder Woman: The Life, Death, and Life After Death of Henrietta Lacks, Unwitting Heroine of Modern Medical Science" by Van Smith
- "What's Left of Henrietta Lacks?" by Anne Enright
- "Culturing Life: How Cells Became Technologies" a book by Hannah Landecker about HeLa and the history of tissue culture.
- Discussion about the taxonomic effect of creating the new taxon Helacyton.
- Cell Centered Database – HeLa cell
- Audio Interview with Rebecca Skloot about her book "The Immortal Life of Henrietta Lacks"
- Cellosaurus entry for HeLa
- The Legacy of Henrietta Lacks