Giardiasis
| Giardiasis | |
|---|---|
| Synonyms | Beaver fever, giardia |
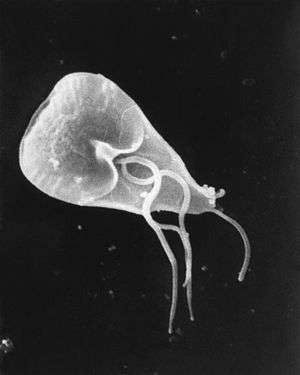 | |
| Giardia cell, SEM | |
| Specialty | Infectious disease |
| Symptoms | Diarrhea, abdominal pain, weight loss[1] |
| Usual onset | 1 to 3 weeks after exposure[2] |
| Causes | Giardia lamblia[1] |
| Diagnostic method | Stool testing[1] |
| Differential diagnosis | Irritable bowel syndrome[1] |
| Prevention | Improved sanitation[1] |
| Medication | Tinidazole, metronidazole[1] |
| Frequency | Up to 7% (developed world), up to 30% (developing world)[1] |
Giardiasis, popularly known as beaver fever,[3] is a parasitic disease caused by Giardia lamblia.[4] About 10% of those infected have no symptoms.[1] When symptoms occur they may include diarrhea, abdominal pain, and weight loss.[1] Vomiting, blood in the stool, and fever are less common.[1] Symptoms usually begin 1 to 3 weeks after exposure and without treatment may last up to six weeks.[2]
Giardia usually spreads when Giardia lamblia cysts within feces contaminate food or water which is then eaten or drunk.[1] It may also spread between people and from other animals.[1] Risk factors include travel in the developing world, changing diapers, eating food without cooking it, and owning a dog.[1] Cysts may survive for nearly three months in cold water.[1] Diagnosis is via stool tests.[1]
Prevention is typically by improved hygiene.[1] Those without symptoms do not usually need treatment.[1] When symptoms are present treatment is typically with either tinidazole or metronidazole.[1] People who are not already lactose intolerant may become so temporarily after an infection and therefore it is often recommended milk be avoided for a few weeks.[1] Resistance to treatment may occur.[1]
Giardia is one of the most common parasitic human diseases globally.[4] In 2013, there were about 280 million people worldwide with symptomatic giardiasis.[4] Rates are as high as 7% in the developed world and 30% in the developing world.[1] The World Health Organization classified it as a neglected disease.[1]
Signs and symptoms
Symptoms vary from none to severe diarrhea with poor absorption of nutrients.[5] Symptoms typically develop 9–15 days after exposure,[6] but may occur as early as one day.[5]
The most common and prominent symptom is chronic diarrhea which can occur for weeks or months if untreated.[7][8] Diarrhea is often greasy and foul-smelling, with a tendency to float.[7][9] This characteristic diarrhea is often accompanied by a number of other symptoms, including gas, abdominal cramps, and nausea or vomiting.[9][7] Some people also experience itchy skin, hives, and swelling of the eyes and joints, although these are less common.[9]
Prolonged disease is often characterized by diarrhea along with malabsorption of nutrients in the intestine.[7] This malabsorption results in fatty stools, substantial weight loss, and fatigue.[7] Additionally, those suffering from giardiasis often have difficulty absorbing lactose, vitamin A, folate, and vitamin B12.[8][9] In children, prolonged giardiasis can cause failure to thrive and may impair mental development.[8][7]
Symptomatic infections are well recognized as causing lactose intolerance,[10] which, while usually temporary, may become permanent.[11][12]
Cause
Giardiasis is caused by the protozoan Giardia lamblia.[13] The infection occurs in many animals including beavers (hence its nickname), as well as cows, other rodents, and sheep.[13] Animals are believed to play a role in keeping infections present in an environment.[13]
G. duodenalis has been sub-classified into eight genetic assemblages (designated A–H). Genotyping of G. duodenalis isolated from various hosts has shown that assemblages A and B infect the largest range of host species, and appear to be the main (or possibly only) G. duodenalis assemblages that undeniably infect humans.[14]
Risk factors
According to the CDC, "Those at greatest risk are travelers to countries where giardiasis is common, people in child care settings, those who are in close contact with someone who has the disease, people who swallow contaminated drinking water, backpackers or campers who drink untreated water from lakes or rivers, people who have contact with animals who have the disease, and men who have sex with men."[15]
In the United States, giardiasis occurs more often during the summer. This is believed to be due to a greater amount of time spent on outdoor activities and traveling in the wilderness.[13]
Transmission
Giardiasis is transmitted via the fecal-oral route with the ingestion of cysts.[6] Primary routes are personal contact and contaminated water and food.[6] The cysts can stay infectious for up to three months in cold water.[13]
Many people with Giardia infections have no or few symptoms.[16] They may, however, still spread the disease.[16]
Pathophysiology
Giardia are flagellated protozoans that cause decreased expression of brush border enzymes, morphological changes to the microvillus, and programmed cell death of small intestinal epithelial cells. There is no invasion of giardia trophozoites, and small intestinal morphology may appear normal in light microscopy.
The attachment of trophozoites causes villus flattening and inhibition of enzymes that break down disaccharide sugars in the intestines. Ultimately, the community of microorganisms that lives in the intestine may overgrow and may be the cause of further symptoms, though this idea has not been fully investigated. The alteration of the villi leads to an inability of nutrient and water absorption from the intestine, resulting in diarrhea, one of the predominant symptoms. In the case of asymptomatic giardiasis, there can be malabsorption with or without histological changes to the small intestine. The degree to which malabsorption occurs in symptomatic and asymptomatic cases is highly varied.
The species Giardia intestinalis uses enzymes that break down proteins to attack the villi of the brush border and appears to increase crypt cell proliferation and crypt length of crypt cells existing on the sides of the villi. On an immunological level, activated host T lymphocytes attack endothelial cells that have been injured in order to remove the cell. This occurs after the disruption of proteins that connect brush border endothelial cells to one another. The result is heavily increased intestinal permeability.
There appears to be a further increase in programmed cell death by Giardia intestinalis, which further damages the intestinal barrier and increases permeability. There is significant upregulation of the programmed cell death cascade by the parasite, and, furthermore, substantial downregulation of the anti-apoptotic protein Bcl-2 and upregulation of the proapoptotic protein Bax. These connections suggest a role of caspase-dependent apoptosis in the pathogenesis of giardiasis.
Giardia protects its own growth by reducing the formation of the gas nitric oxide by consuming all local arginine, which is the amino acid necessary to make nitric oxide. Arginine starvation is known to be a cause of programmed cell death, and local removal is a strong apoptotic agent.[17]
Diagnosis
- According to the CDC, detection of antigens on the surface of organisms in stool specimens is the current test of choice for diagnosis of giardiasis and provides increased sensitivity over more common microscopy techniques.[18]
- A trichrome stain of preserved stool is another method used to detect giardia.[19]
- Microscopic examination of the stool for motile trophozoites or for the distinctive oval G.lamblia cysts can be performed.
- The entero-test uses a gelatin capsule with an attached thread. One end is attached to the inner aspect of the patient's cheek, and the capsule is swallowed. Later, the thread is withdrawn and shaken in saline to release trophozoites which can be detected with a microscope.
- Immunologic enzyme-linked immunosorbent assay (ELISA) testing is now available. These tests are capable of a 90% detection rate or more.[20]
- Because Giardia lamblia is difficult to detect, this often leads to a delay in diagnosis or misdiagnosis; several tests should be conducted over a one-week period.[21]
Although hydrogen breath tests indicate poorer rates of carbohydrate absorption in those asymptomatically infected, such tests are not diagnostic of infection.[22]
Prevention
The CDC recommends hand-washing and avoiding potentially contaminated food and untreated water.[23]
Boiling suspect water for one minute is the surest method to make water safe to drink and kill disease-causing microorganisms such as Giardia lamblia if in doubt about whether water is infected.[24] Chemical disinfectants or filters may be used.[25][26]
Although the evidence linking the drinking of water in the North American wilderness and giardiasis has been questioned, a number of studies raise concern.[27] Most if not all CDC verified backcountry giardiasis outbreaks have been attributed to water. Surveillance data (for 2013 and 2014) reports six outbreaks (96 cases) of waterborne giardiasis contracted from rivers, streams or springs[28] and less than 1% of reported giardiasis cases are associated with outbreaks.[29]
Person-to-person transmission accounts for the majority of Giardia infections and is usually associated with poor hygiene and sanitation. Giardia is found on the surface of the ground, in the soil, in undercooked foods, and in water, and on hands without proper cleaning after handling infected feces.[30] Water-borne transmission is associated with the ingestion of contaminated water. In the U.S., outbreaks typically occur in small water systems using inadequately treated surface water. Venereal transmission happens through fecal-oral contamination. Additionally, diaper changing and inadequate hand washing are risk factors for transmission from infected children. Lastly, food-borne epidemics of Giardia have developed through the contamination of food by infected food-handlers.[31]
Treatment
Treatment is not always necessary as the infection usually resolves on its own. However, if the illness is acute or symptoms persist and medications are needed to treat it, a nitroimidazole medication is used such as metronidazole, tinidazole, secnidazole or ornidazole.[6]
The World Health Organization and Infectious Disease Society of America recommend metronidazole as first line therapy.[32][33] The US CDC lists metronidazole, tinidazole, and nitazoxanide as effective first-line therapies;[34] of these three, only nitazoxanide and tinidazole are approved for the treatment of giardiasis by the US FDA.[35][36][37] A meta-analysis done by the Cochrane Collaboration found that compared to the standard of metronidazole, albendazole had equivalent efficacy while having fewer side effects, such as gastrointestinal or neurologic issues.[38] Other meta-analyses have reached similar conclusions.[39] Both medications need a five to 10 day long course; albendazole is taken once a day, while metronidazole needs to be taken three times a day. The evidence for comparing metronidazole to other alternatives such as mebendazole, tinidazole or nitazoxanide was felt to be of very low quality.[38] While tinidazole has side effects and efficacy similar to those of metronidazole, it is administered with a single dose.[16]
Resistance has been seen clinically to both nitroimidazoles and albendazole, but not nitazoxanide, though nitazoxanide resistance has been induced in research laboratories so is theoretically possible.[40] The exact mechanism of resistance to all of these medications is not well understood.[40] In the case of nitroimidazole-resistant strains of Giardia, other drugs are available which have showed efficacy in treatment including quinacrine, nitazoxanide, bacitracin zinc, furazolidone and paromomycin.[16]
During pregnancy, paromomycin is the preferred treatment drug because of its poor intestinal absorption, and thus less exposure to the fetus.[41] Alternatively, metronidazole can be used after the first trimester as there has been wide experience in its use for trichomonas in pregnancy.[42][43]
Epidemiology
In some developing countries Giardia is present in 30% of the population.[13] In the United States it is estimated that it is present in 3–7% of the population.[13]
According to the Center For Disease Control in 2011, the total number of reported cases was 16,784. In the U.S. in 2012, the number of reported cases totaled 15,197. In the United States during that time period, all states that classify giardiasis as a notifiable disease had cases of giardiasis. Mississippi, North Carolina, Oklahoma, Tennessee, Texas, and Kentucky do not notify the Center for Disease Control regarding giardiasis cases. The states with the highest prevalence of giardiasis from 2011-2012 were New York State, Minnesota, Ohio, Florida, Washington, and California, according to the Center for Disease Control. There are seasonal trends associated with giardiasis. July, August, and September are the months with the highest prevalence of giardiasis in the United States.[44]
Giardia has an international distribution with a global prevalence of roughly 30 percent. It has been classified as endemic in many developing countries and can be linked to hindered child development. In the ECDC's (European Centre for Disease Prevention Control) annual epidemiological report containing 2014 data, 17,278 confirmed giardiasis cases were reported by 23 of the 31 countries that are members of the EU/EEA. Germany reported the highest number at 4,011 cases. Following Germany, the UK reported 3,628 confirmed giardiasis cases. Together, this accounts for 44% of total reported cases.[45]
Research
Some intestinal parasitic infections may play a role in irritable bowel syndrome[46] and other long-term sequelae.[47]
Other animals
In cats, giardiasis responds to metronidazole, although this should not be administered to pregnant cats as it can cause developmental malformations. An alternative and effective drug is febendazole.[48]
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 Minetti, C; Chalmers, RM; Beeching, NJ; Probert, C; Lamden, K (27 October 2016). "Giardiasis". BMJ (Clinical research ed.). 355: i5369. doi:10.1136/bmj.i5369. PMID 27789441.
- 1 2 "Parasites - Giardia". CDC. 21 July 2015. Archived from the original on 17 November 2016. Retrieved 17 November 2016.
- ↑ "Giardiasis (beaver fever)". New York State Department of Health. October 2011. Archived from the original on 11 May 2015. Retrieved 21 June 2015.
- 1 2 3 Esch KJ, Petersen CA (January 2013). "Transmission and epidemiology of zoonotic protozoal diseases of companion animals". Clin Microbiol Rev. 26 (1): 58–85. doi:10.1128/CMR.00067-12. PMC 3553666. PMID 23297259.
- 1 2 "Giardiasis". cdc.gov. November 29, 2013. Archived from the original on January 15, 2016. Retrieved 1 Jan 2016.
- 1 2 3 4 Barry MA, Weatherhead JE, Hotez PJ, Woc-Colburn L (2013). "Childhood parasitic infections endemic to the United States". Pediatr Clin North Am. 60 (2): 471–85. doi:10.1016/j.pcl.2012.12.011. PMID 23481112.
- 1 2 3 4 5 6 Despommier DD, Griffin DO, Gwadz RW, Hotez PJ, Knirsch CA. "III. Eukaryotic Parasites". Parasitic Diseases (6 ed.). NY: Parasites Without Borders. pp. 11–17. Retrieved 11 July 2018.
- 1 2 3 Robertson LJ, Hanevik K, Escobedo AA, Morch K, Langeland N (2010). "Giardiasis - why do the symptoms sometimes never stop?". Trends in Parasitology. 26 (2): 75–82. doi:10.1016/j.pt.2009.11.010.
- 1 2 3 4 "Giardia - Illness & Symptoms". CDC. Retrieved 11 July 2018.
- ↑ Pettoello Mantovani M, Guandalini S, Ecuba P, Corvino C, di Martino L (1989). "Lactose malabsorption in children with symptomatic Giardia lamblia infection: feasibility of yogurt supplementation". J. Pediatr. Gastroenterol. Nutr. 9 (3): 295–300. doi:10.1097/00005176-198910000-00006. PMID 2614615.
- ↑ Wolfe MS (1975). "Giardiasis". JAMA. 233 (13): 1362–5. doi:10.1001/jama.233.13.1362. PMID 1174208.
- ↑ Vega-Franco L, Meza C, Romero JL, Alanis SE, Meijerink J (1987). "Breath hydrogen test in children with giardiasis". J. Pediatr. Gastroenterol. Nutr. 6 (3): 365–8. doi:10.1097/00005176-198705000-00010. PMID 3430245.
- 1 2 3 4 5 6 7 Auerbach, Paul S. (2012). Wilderness medicine (6th ed.). Philadelphia, PA: Elsevier/Mosby. pp. Chapter 68. ISBN 9781437716788.
- ↑ Heyworth, Martin F. (2016). "Giardia duodenalis genetic assemblages and hosts". Parasite. 23: 13. doi:10.1051/parasite/2016013. ISSN 1776-1042. Archived from the original on 2017-09-10.

- ↑ CDC (July 15, 2015). "Sources of Infection & Risk Factors". Parasites – Giardia. Archived from the original on September 7, 2017.
- 1 2 3 4 Gardner, TB; Hill, DR (Jan 2001). "Treatment of giardiasis". Clinical Microbiology Reviews. 14 (1): 114–28. doi:10.1128/CMR.14.1.114-128.2001. PMC 88965. PMID 11148005.
- ↑ Muhkerjee, Sandeep. "Giardiasis". Medscape Reference. Archived from the original on 17 November 2012. Retrieved 21 November 2012.
- ↑ "Archived copy". Archived from the original on 2017-06-17. Retrieved 2017-09-09.
- ↑ "Archived copy". Archived from the original on 2014-10-29. Retrieved 2014-10-29.
- ↑ Rosenblatt, John E. (May–June 1993). "Evaluation of an enzyme-linked immunosorbent assay for the detection of Giardia lamblia in stool specimens". Diagnostic Microbiology and Infectious Disease. 16 (4): 337–341. doi:10.1016/0732-8893(93)90086-M. PMID 8495591. Retrieved 28 February 2015.
- ↑ Center for Disease Control—Parasite division—Giardia
- ↑ Moya-Camarena SY, Sotelo N, Valencia ME (2002). "Effects of asymptomatic Giardia intestinalis infection on carbohydrate absorption in well-nourished Mexican children" (PDF). Am. J. Trop. Med. Hyg. 66 (3): 255–9. PMID 12139217. Archived from the original on 2008-07-06.
- ↑ "Parasites - Giardia, Prevention & Control". Centers for Disease Control and Prevention. CDC. Archived from the original on 30 April 2015. Retrieved 26 April 2015.
- ↑ "Emergency Disinfection of Drinking Water". United State Envirinment Protection Agency. Archived from the original on 23 June 2015. Retrieved 21 June 2015. Retrieved 24 February 2011
- ↑ Betancourt, WQ; Rose, JB (2004). "Drinking water treatment processes for removal of Cryptosporidium and Giardia". Veterinary parasitology. 126 (1–2): 219–34. doi:10.1016/j.vetpar.2004.09.002. PMID 15567586.
- ↑ Exner, M; Gornik, V (2004). "Parasitic zoonoses transmitted by drinking water. Giardiasis and cryptosporidiosis". Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz. 47 (7): 698–704. doi:10.1007/s00103-004-0863-y. PMID 15254826.
- ↑ Painter, Julia E. (2015). "Giardiasis Surveillance—United States, 2011–2012". CDC MMWR Surveill Summ. 64 (Suppl 3): 15-25. Retrieved 31 March 2018.
- ↑ McClung, R. Paul; Roth, David M.; Vigar, Marissa; Roberts, Virginia A.; Kahler, Amy M.; Cooley, Laura A.; Hilborn, Elizabeth D.; Wade, Timothy J.; Fullerton, Kathleen E.; Yoder, Jonathan S.; Hill, Vincent R. (2017). "Waterborne Disease Outbreaks Associated With Environmental and Undetermined Exposures to Water — United States, 2013–2014". MMWR. Morbidity and Mortality Weekly Report. 66 (44): 1222–1225. doi:10.15585/mmwr.mm6644a4. ISSN 0149-2195.
- ↑ "Giardiasis Surveillance — United States, 2009–2010". www.cdc.gov.
- ↑ CDC Giardia 2011
- ↑ Giardiasis at eMedicine
- ↑ Guerrant RL, Van Gilder T, Steiner TS, Thielman NM, Slutsker L, Tauxe RV, Hennessy T, Griffin PM, DuPont H, Sack RB, Tarr P, Neill M, Nachamkin I, Reller LB, Osterholm MT, Bennish ML, Pickering LK (January 30, 2001). "Practice Guidelines for the Management of Infectious Diarrhea" (PDF). Clinical Infectious Diseases. 32: 331–51. doi:10.1086/318514. PMID 11170940. Archived (PDF) from the original on February 10, 2016.
- ↑ "Chapter 7.5.4 Continuing Diarrhoea | ICHRC". www.ichrc.org. Archived from the original on 2016-01-29. Retrieved 2016-01-09.
- ↑ "Giardia: Treatment". United States Centers for Disease Control and Prevention. 21 July 2015. Archived from the original on 24 December 2015. Retrieved 10 January 2016.
Several drugs can be used to treat Giardia infection. Effective treatments include metronidazole, tinidazole, and nitazoxanide1. Alternatives to these medications include paromomycin, quinacrine, and furazolidone1,2.
- ↑ "Nitazoxanide Prescribing Information" (PDF). Romark Pharmaceuticals. August 2013. pp. 1–5. Archived (PDF) from the original on 16 January 2016. Retrieved 3 January 2016.
- ↑ "Metronidazole Prescribing Information" (PDF). United States Food and Drug Administration. Pfizer. June 2015. pp. 6–7. Archived (PDF) from the original on 4 March 2016. Retrieved 10 January 2016.
- ↑ "Tinidazole Prescribing Informatiuon" (PDF). United States Food and Drug Administration. Mission Pharma. May 2007. p. 1. Archived (PDF) from the original on 4 March 2016. Retrieved 10 January 2016.
- 1 2 Granados, Carlos E; Reveiz, Ludovic; Uribe, Luis G; Criollo, Claudia P (2012-12-12). Drugs for treating giardiasis. John Wiley & Sons, Ltd. doi:10.1002/14651858.cd007787.pub2. Archived from the original on 2017-07-28.
- ↑ Solaymani-Mohammadi, S; Genkinger, JM; Loffredo, CA; Singer, SM (May 11, 2010). Keiser, Jennifer, ed. "A meta-analysis of the effectiveness of albendazole compared with metronidazole as treatments for infections with Giardia duodenalis". PLOS Neglected Tropical Diseases. 4 (5): e682. doi:10.1371/journal.pntd.0000682. PMC 2867942. PMID 20485492.
- 1 2 Leitsch, David (2015-07-07). "Drug Resistance in the Microaerophilic Parasite Giardia lamblia". Current Tropical Medicine Reports. 2 (3): 128–135. doi:10.1007/s40475-015-0051-1. ISSN 2196-3045. PMC 4523694. PMID 26258002.
- ↑ Farthing, Michael JG (2005). "Treatment Options for the Eradication of Intestinal Protozoa". Nature Clinical Practice Gastroenterology & Hepatology. 3: 436–445. doi:10.1038/ncpgasthep0557. PMID 16883348. Archived from the original on 21 June 2015. Retrieved 21 June 2015.
- ↑ Gardner, Timothy B.; Hill, David R. (2001-01-01). "Treatment of Giardiasis". Clinical Microbiology Reviews. 14 (1): 114–128. doi:10.1128/CMR.14.1.114-128.2001. ISSN 0893-8512. PMC 88965. PMID 11148005. Archived from the original on 2017-09-10.
- ↑ Workowski, Kimberly A.; Bolan, Gail A. (2015-06-05). "Sexually transmitted diseases treatment guidelines, 2015". MMWR. Recommendations and reports: Morbidity and Mortality Weekly Report. Recommendations and reports / Centers for Disease Control. 64 (RR-03): 1–137. ISSN 1545-8601. PMID 26042815.
- ↑ Yoder, Gargano, Wallace, Beach. "Giardiasis Surveillance-United States, 2009-2010". Center for Disease Control and Prevention. Centers of Disease Control and Prevention. Retrieved 30 November 2017.
- ↑ "Giardiasis- Annual Epidemiological Report 2016". European Centre for Disease Prevention and Control. European Centre for Disease Prevention and Control. Retrieved 30 November 2017.
- ↑ Stark D, van Hal S, Marriott D, Ellis J, Harkness J (January 2007). "Irritable bowel syndrome: a review on the role of intestinal protozoa and the importance of their detection and diagnosis". Int. J. Parasitol. 37 (1): 11–20. doi:10.1016/j.ijpara.2006.09.009. PMID 17070814.
- ↑ Quote: "for unclear reasons, chronic sequelae, including post-infectious irritable bowel syndrome, chronic fatigue [..], malnutrition [..], cognitive impairment [..], and extra-intestinal manifestations (such as food allergy, urticaria, reactive arthritis, and inflammatory ocular manifestations), can develop and possibly persist beyond detectable parasite shedding". Quoted from: Bartelt LA, Sartor RB (2015). "Advances in understanding Giardia: determinants and mechanisms of chronic sequelae". F1000Prime Reports (Review). 7: 62. doi:10.12703/P7-62. PMC 4447054. PMID 26097735.
- ↑ Eldredge, Debra M. (2008). Cat Owner's Home Veterinary Handbook. Howell Book House. p. 67.
Further reading
- Kathleen Meyer, How to Shit in the Woods: An Environmentally Sound Approach to a Lost Art, Ten Speed Press (1989). A practical guide to wilderness waste disposal to prevent giardiasis.
External links
| Classification | |
|---|---|
| External resources |