Computed tomography angiography
| Computed tomography angiography | |
|---|---|
| Medical diagnostics | |
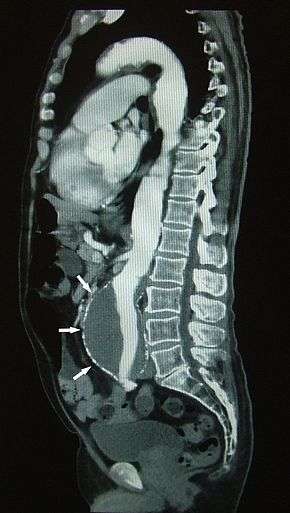 Sagittal thin slice of a computed tomography angiography abdominal aortic aneurysm (AAA) (arrows) | |
| OPS-301 code | 3-228 |
Computed tomography angiography (also called CT angiography or CTA) is a computed tomography technique used to visualize arterial and venous vessels throughout the body. This ranges from arteries serving the brain to those bringing blood to the lungs, kidneys, arms and legs.
Medical uses
CTA can be used to examine blood vessels in many key areas of the body, including the brain, kidneys, pelvis, and the lungs.
Coronary CT angiography
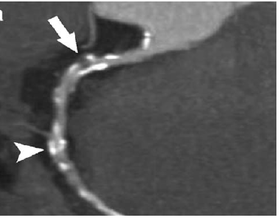
Coronary CT angiography (CTA) is the use of CT angiography to assess the coronary arteries of the heart. The subject receives an intravenous injection of radiocontrast and then the heart is scanned using a high speed CT scanner, allowing radiologists to assess the extent of occlusion in the coronary arteries, usually in order to diagnose coronary artery disease. CTA has not replaced invasive catheter coronary angiography. The procedure is able to detect narrowing of blood vessels in time for corrective therapy to be done. This method displays the anatomical detail of blood vessels more precisely than magnetic resonance imaging (MRI) or ultrasound. Today, many patients can undergo CTA in place of a conventional catheter angiogram. CTA is a useful way of screening for arterial disease because it is safer and much less time-consuming than catheter angiography and is a cost-effective procedure. There is also less discomfort because contrast material is injected into an arm vein rather than into a large artery in the groin.
Other uses
CTA is commonly used for the following purposes:
- CT pulmonary angiogram (CTPA) to examine the pulmonary arteries in the lungs, most commonly to rule out pulmonary embolism, a serious but treatable condition.
- Visualize blood flow in the renal arteries (those supplying the kidneys) in patients with high blood pressure and those suspected of having kidney disorders. Narrowing (stenosis) of a renal artery is a cause of high blood pressure (hypertension) in some patients and can be corrected. A special computerized method of viewing the images makes renal CT angiography a very accurate examination. Also done in prospective kidney donors.
- Identify aneurysms in the aorta or in other major blood vessels. Aneurysms are diseased areas of a weakened blood vessel wall that bulges out—like a bulge in a tire. Aneurysms are life-threatening because they can rupture.
- Identify dissection in the aorta or its major branches. Dissection means that the layers of the artery wall peel away from each other—like the layers of an onion. Dissection can cause pain and can be life-threatening.
- Identify a small aneurysm or arteriovenous malformation inside the brain that can be life-threatening.
- Detect atherosclerotic disease that has narrowed the arteries to the legs.
- Exclude coronary artery disease, especially in low to intermediate risk patients.
Technique
CT angiography is a contrast CT where images taken with a certain delay after injection of radiocontrast to result in a high radiodensity within the blood vessels of interest.
Risks
CT angiography should not be used to evaluate for pulmonary embolism when other tests indicate that there is a low probability of a person having this condition.[1] A D-dimer assay might be a preferred alternative to test for pulmonary embolism, and that test and a low clinical prediction score on the Wells test or Geneva score can exclude pulmonary embolism as a possibility.[1]
Harms of overuse of CT angiography include radiation exposure and the possibility of finding then seeking treatment for a clinically insignificant pulmonary embolism which ought not be treated.[1]
There is a risk of an allergic reaction, which may be serious, whenever contrast material containing iodine is injected. A patient with a history of allergy to x-ray dye may be advised to take special medication for 24 hours before CTA to lessen the risk of allergic reaction or to undergo a different exam that does not call for contrast material injection. CTA should be avoided in patients with kidney disease or severe diabetes, because x-ray contrast material can further harm kidney function. If a large amount of x-ray contrast material leaks out under the skin where the IV is placed, skin damage can result. Compared with other imaging modalities, CTA is associated with a significant dose of ionizing radiation. Depending on patient age and exam protocol, CTA may cause a considerable increase in lifetime cancer risk.[2] However, there are many clinical situations for which the benefits of performing the procedure outweigh this risk.
History
By 1994 CT angiography began to replace conventional angiography in diagnosing and characterizing most cardiovascular abnormalities.[3] Prior to this, conventional angiography had been in use for 70 years.[3]
See also
References
- 1 2 3 American College of Chest Physicians; American Thoracic Society (September 2013), "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation, American College of Chest Physicians and American Thoracic Society, retrieved 6 January 2013
, which cites
- Fesmire, FM; Brown, MD; Espinosa, JA; Shih, RD; Silvers, SM; Wolf, SJ; Decker, WW; American College of Emergency, Physicians (Jun 2011). "Critical issues in the evaluation and management of adult patients presenting to the emergency department with suspected pulmonary embolism". Annals of Emergency Medicine. 57 (6): 628–652.e75. doi:10.1016/j.annemergmed.2011.01.020. PMID 21621092.
- Qaseem, A; Snow, V; Barry, P; Hornbake, ER; Rodnick, JE; Tobolic, T; Ireland, B; Segal, J; Bass, E; Weiss, KB; Green, L; Owens, DK; Joint American Academy of Family Physicians/American College of Physicians Panel on Deep Venous Thrombosis/Pulmonary, Embolism (Jan–Feb 2007). "Current diagnosis of venous thromboembolism in primary care: a clinical practice guideline from the American Academy of Family Physicians and the American College of Physicians". Annals of Family Medicine. 5 (1): 57–62. doi:10.1370/afm.667. PMC 1783928. PMID 17261865.
- Torbicki, A; Perrier, A; Konstantinides, S; Agnelli, G; Galiè, N; Pruszczyk, P; Bengel, F; Brady, AJ; Ferreira, D; Janssens, U; Klepetko, W; Mayer, E; Remy-Jardin, M; Bassand, JP; ESC Committee for Practice Guidelines, (CPG) (Sep 2008). "Guidelines on the diagnosis and management of acute pulmonary embolism: the Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC)". European Heart Journal. 29 (18): 2276–315. doi:10.1093/eurheartj/ehn310. PMID 18757870.
- ↑ Einstein, A. J.; Henzlova, M. J.; Rajagopalan, S (2007). "Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography". JAMA. 298 (3): 317–23. doi:10.1001/jama.298.3.317. PMID 17635892.
- 1 2 Rubin, Geoffrey D.; Leipsic, Jonathon; Schoepf, U. Joseph; Fleischmann, Dominik; Napel, Sandy. "CT Angiography after 20 Years: A Transformation in Cardiovascular Disease Characterization Continues to Advance". Radiology. 271 (3): 633–652. doi:10.1148/radiol.14132232. PMC 4669887. PMID 24848958.