Contrast CT

Contrast CT is X-ray computed tomography (CT) using radiocontrast. Radiocontrasts for X-ray CT are, in general, iodine-based.[1] This is useful to highlight structures such as blood vessels that otherwise would be difficult to delineate from their surroundings. Using contrast material can also help to obtain functional information about tissues. Often, images are taken both with and without radiocontrast. CT images are called precontrast or native-phase images before any radiocontrast has been administrated, and postcontrast after radiocontrast administration.[2]
Bolus tracking
Bolus tracking is a technique used in computed tomography imaging to optimize timing of the imaging. A small bolus of radio-opaque contrast media is injected into a patient via a peripheral intravenous cannula. Depending on the vessel being imaged, the volume of contrast is tracked using a region of interest (abbreviated "R.O.I.") at a certain level and then followed by the CT scanner once it reaches this level. Images are acquired at a rate as fast as the contrast moving through the blood vessels.
This method of imaging is used primarily to produce images of arteries, such as the aorta, pulmonary artery, cerebral, carotid and hepatic arteries.
Washout
"Washout" is where tissue loads radiocontrast during arterial phase, but then returns to a rather hypodense state in venous or later phases. This is a property of for example hepatocellular carcinoma as compared to the rest of the liver parenchyma.[3]
Phases
Depending on the purpose of the investigation, there are standardized protocols for time intervals between intravenous radiocontrast administration and image acquisition, in order to visualize the dynamics of contrast enhancements in different organs and tissues.[4] The main phases thereof are as follows:[5]
| Phase | Time from injection[5] | Time from bolus tracking[5] | Targeted structures and findings[5] |
|---|---|---|---|
| Non-enhanced CT (NECT) | - | - |
|
| Pulmonary arterial phase | 6-13 sec[6] | - | |
| Pulmonary venous phase | 17-24 sec[6] | - | |
| Early systemic arterial phase | 15-20 sec | immediately |
|
| Late systemicarterial phase Sometimes also called "arterial phase" or "early venous portal phase" |
35-40 sec | 15-20 sec |
|
| Pancreatic phase | 30[7] or 40[8] - 50[8] sec | 20-30 sec |
|
| Hepatic (most accurate) or late portal phase | 70-80 sec | 50-60 sec |
|
| Nephrogenic phase | 100 sec | 80 sec |
|
| Systemic venous phase | 180 sec[9] | 160 sec |
|
| Delayed phase Sometimes called "wash out phase" or "equilibrium phase" |
6[5]-15[9] minutes | 6[5]-15[9] minutes |
|
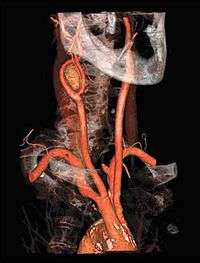
Angiography
CT angiography is a contrast CT taken at the location and corresponding phase of the blood vessels of interest, in order to detect vascular diseases. For example, an abdominal aortic angiography is taken in the arterial phase in the abdominal level, and is useful to detect for example aortic dissection.[10]
See also
References
- ↑ Webb, W. Richard; Brant, Wiliam E.; Major, Nancy M. (2014). Fundamentals of Body CT. Elsevier Health Sciences. p. 152. ISBN 9780323263580.
- ↑ Dahlman P, Semenas E, Brekkan E, Bergman A, Magnusson A (2000). "Detection and Characterisation of Renal Lesions by Multiphasic Helical Ct". Acta Radiologica. 41 (4): 361–366. doi:10.1080/028418500127345479. PMID 10937759.
- ↑ Choi, Jin-Young; Lee, Jeong-Min; Sirlin, Claude B. (2014). "CT and MR Imaging Diagnosis and Staging of Hepatocellular Carcinoma: Part II. Extracellular Agents, Hepatobiliary Agents, and Ancillary Imaging Features". Radiology. 273 (1): 30–50. doi:10.1148/radiol.14132362. ISSN 0033-8419. PMC 4263770. PMID 25247563.
- ↑ Bae, Kyongtae T. (2010). "Intravenous Contrast Medium Administration and Scan Timing at CT: Considerations and Approaches". Radiology. 256 (1): 32–61. doi:10.1148/radiol.10090908. ISSN 0033-8419.
- 1 2 3 4 5 6 Robin Smithuis. "CT contrast injection and protocols". Radiology Assistant. Retrieved 2017-12-13.
- 1 2 Page 584 in: Ákos Jobbágy (2012). 5th European Conference of the International Federation for Medical and Biological Engineering 14 - 18 September 2011, Budapest, Hungary. Volume 37 of IFMBE Proceedings. Springer Science & Business Media. ISBN 9783642235085.
- ↑ Raman SP, Fishman EK (2012). "Advances in CT Imaging of GI Malignancies". Gastrointest Cancer Res. 5 (3 Suppl 1): S4–9. PMC 3413036. PMID 22876336.
- 1 2 3 Otto van Delden and Robin Smithuis. "Pancreas - Carcinoma". Radiology Assistant. Retrieved 2017-12-15.
- 1 2 3 4 Dongqing Wang (2013). Selected Topics on Computed Tomography. ISBN 9789535111023. License: CC-BY-3.0. Chapter 1: "Computed Tomography in Abdominal Imaging: How to Gain Maximum Diagnostic Information at the Lowest Radiation Dose" by Kristie Guite, Louis Hinshaw and Fred Lee. DOI: 10.5772/55903
- ↑ Page 424 in: Stuart E. Mirvis, Jorge A Soto, Kathirkamanathan Shanmuganathan, Joseph Yu, Wayne S Kubal (2014). Problem Solving in Emergency Radiology E-Book. Elsevier Health Sciences. ISBN 9781455758395.