Chlortalidone
 | |
 | |
| Clinical data | |
|---|---|
| Trade names | Hygroton, Thalitone (Ciba-Geigy) |
| AHFS/Drugs.com | Consumer Drug Information |
| MedlinePlus | a682342 |
| Pregnancy category | |
| Routes of administration | Oral |
| ATC code | |
| Legal status | |
| Legal status |
|
| Pharmacokinetic data | |
| Protein binding | 75% |
| Elimination half-life | 40 hours |
| Excretion | Renal |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| ECHA InfoCard |
100.000.930 |
| Chemical and physical data | |
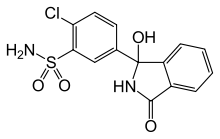
| Formula | C14H11ClN2O4S |
| Molar mass | 338.766 g/mol |
| 3D model (JSmol) | |
| Chirality | Racemic mixture |
| |
| |
| (verify) | |
Chlortalidone (INN/BAN) or chlorthalidone (USAN) is a diuretic medication used to treat hypertension (high blood pressure), enlargement of the main pumping chamber of the heart, edema ( fluid retention), and nephrogenic diabetes insipidus (inability of an injured kidney to produce concentrated urine) and to prevent calcium oxalate kidney stones and bone fracture due to osteopenia. It is a thiazide-like diuretic of the sulfonamide class.
Chlortalidone is more effective at lowering blood pressure than the similar medication, hydrochlorothiazide, particularly toward the end of the dosing interval. Chlortalidone and hydrochlorothiazide have a similar risk of causing low blood potassium levels and other adverse effects at the usual doses prescribed in routine clinical practice. Chlortalidone is sometimes used as the sole medication for treating high blood pressure.
It is also often used in combination with an angiotensin converting enzyme inhibitor or angiotensin II receptor blocker or other antihypertensive drugs for lowering blood pressure, and also as an adjuvant medication for treating edema caused by heart failure and kidney disorders, such as nephrotic syndrome. Chlortalidone has a long duration of action, 24 to 72 hours, and can be given once a day.
Chemistry
Chlortalidone is in the sulfamoylbenzamide class. As it lacks the benzothiadiazine structure of the thiazide-type diuretics, it is called a thiazide-like diuretic.[1] Chlortalidone is freely soluble in dimethylacetamide (DMA), dimethylformamide (DMF), dimethylsulfoxide (DMSO), and methanol; it is also soluble in warm ethanol.[2]
Mechanisms of action
Diuretic effect
Chlortalidone, reduces reabsorption of sodium and chloride primarily through inhibition of the Na+/Cl− symporter in the apical membrane of distal convoluted tubule cells in the kidney.[3] Some of chlortalidone's diuretic effect is also due to inhibition of carbonic anhydrase in the proximal tubule.[4] Chronic exposure to chlortalidone decreases the glomerular filtration rate. Chlortalidone's diuretic effect is diminished in persons with kidney impairment. By increasing the delivery of sodium to the distal renal tubule, chlortalidone indirectly increases potassium excretion via the sodium-potassium exchange mechanism (i.e. apical ROMK/Na channels coupled with basolateral Na+/K ATPases). This can result in a low blood concentration of potassium and chloride as well as a mild metabolic alkalosis; however, the diuretic effect of chlortalidone is not affected by the acid-base balance of the person being treated.
Blood pressure-lowering
There is uncertainty about the mechanism of the blood pressure-lowering effect that occurs during chronic exposure to chlortalidone.[5] Initially, diuretics lower blood pressure by decreasing cardiac output and reducing plasma and extracellular fluid volume. Eventually, cardiac output returns to normal, and plasma and extracellular fluid volume return to slightly less than normal, but a reduction in peripheral vascular resistance is maintained, thus resulting in an overall lower blood pressure. The reduction in intravascular volume induces an elevation in plasma renin activity and aldosterone secretion, further contributing to the potassium loss associated with thiazide diuretic therapy.
Chlortalidone has a modestly greater effect on blood pressure than hydrochlorothiazide[6] but the two medications have similar effects on lowering potassium.[7] The thiazide-like diuretics (chlortalidone and indapamide) are more effective than the thiazide-type diuretics (including hydrochlorothiazide) for reducing the risk of heart attack, stroke, and heart failure in persons with high blood pressure and the thiazide-like and thiazide-type diuretics have similar rates of adverse effects.[8]
Regression of Cardiac Left Ventricular Hypertrophy
Chlortalidone is superior to Angiotensin Converting Enzyme Inhibitors or Angiotensin II receptor blockers for inducing regression of enlargement of the left ventricle, which is the main pumping chamber of the heart.[9]
Kidney stone prevention
Chlorthalidone reduces the amount of calcium excreted in urine, reducing the risk of calcium oxalate kidney stones.[10] In patients who have had multiple episodes of calcium oxalate kidney stones, chlortalidone lowers the risk of having another episode of kidney stones.[11] Chlortalidone is more effective than hydrochlorothiazide for lowering urine calcium levels and is therefore probably more effective.[12]
Bone fracture prevention
Chlorthalidone decreases mineral bone loss by promoting calcium retention by the kidney, and by directly stimulating osteoblast differentiation and bone mineral formation.[13] A Cochrane collaborative systematic review and meta-analysis of observational studies concluded that thiazide exposure was associated with a reduced risk of hip fracture.[14] A secondary analysis of data from the ALLHAT study found that chlorthalidone reduced risk of hip and pelvis fracture.[15]
Reversal of nephrogenic diabetes insipidus
Chlorthalidone (or other thiazide medication) is a key component of treatment of nephrogenic diabetes insipidus. Nephrogenic diabetes insipidus occurs when the kidney is unable to produce concentrated urine because it has an inadequate response to vasopressin-dependent removal of free water from the renal tubular filtrate. By blocking sodium ion resorption in the distal convoluted tubule, chlortalidone induces an increase in excretion of sodium ion in urine (natriuresis). Giving chlorthalidone while simultaneously restricting dietary sodium intake causes mild hypovolemia (low intravascular volume), which induces isotonic reabsorption of solute from the proximal renal tubule, reducing solute delivery in the renal collecting tubule and renal medullary collecting duct. This reduced delivery of solute to the collecting tubule and medullary collecting duct allows increased water resorption and higher concentration of urine, which leads to reversal of nephrogenic diabetes insipidus by a means that is independent of vasopressin. [16]
Efficacy
A clinical trial (ALLHAT) in 2002 compared chlortalidone to doxazosin, lisinopril, and amlodipine in the treatment of high-risk hypertensive patients. In this study, the rate of fatal or nonfatal heart attack was the same for chlortalidone, lisinopril, and amlodipine. ALLHAT subjects treated with chlorthalidone had a lower rate of congestive heart failure than amlodipine or lisinopril or doxazosin. Also, compared to lisinopril subjects, chlortalidone subjects in ALLHAT had a lower risk of developing cardiovascular disease.[17]
Chlortalidone is a low ceiling diuretic (saluretic), which means that the total excretion of the filtered sodium ion load is less than 10% compared to about 30% for the high ceiling loop diuretics.[18] Unlike loop diuretics, chlortalidone's diuretic effect is markedly diminished in patients with certain kidney diseases (e.g. chronic kidney disease).
Adverse effects
Side effects are similar to those of thiazides:
- Hypokalemia, or low blood level of potassium occurs occasionally; the risk of hypokalemia is higher in persons who are magnesium deficient.[19]
- Hypomagnesemia, or low blood level of magnesium occurs occasionally, particularly in persons with diabetes mellitus who have low dietary magnesium intake.
- Hyponatremia (low sodium) is more likely in persons with certain genetic variants of the prostaglandin transporter SLCO2A1 associated with elevated urinary PGE2 and inappropriately low plasma ADH levels in the setting of low plasma osmolality.[20]
- Hypercalcemia (high calcium) is more likely to occur when persons who have sub-clinical hyperparathyroidism are exposed to chlortalidone.
- Hyperuricemia, high levels of uric acid in the blood
- Hyperglycemia, high blood sugar is more common in persons who are magnesium deficient.
- Hyperlipidemia, high cholesterol and triglycerides
- Headache
- Nausea/vomiting
- Photosensitivity
- Weight gain
- Gout
- Pancreatitis
The frequency and severity of these adverse effects is much reduced when chlortalidone is used at lower doses (e.g., 12.5 mg per day).
Banned for some sports
Chlortalidone is banned for some sports (including cricket) because it is a diuretic.[21]
See also
References
- ↑ National Center for Biotechnology Information. PubChem Compound Database; CID=2732, https://pubchem.ncbi.nlm.nih.gov/compound/2732 (accessed July 29, 2018).
- ↑ Singer, Jeff M., Michael J. O'Hare, Carl R. Rehm, and John E. Zarembo. "Chlorthalidone." In Analytical Profiles of Drug Substances, vol. 14, pp. 1-36. Academic Press, 1985. https://doi.org/10.1016/S0099-5428(08)60575-4
- ↑ Gamba G (October 2009). "The thiazide-sensitive Na+-Cl- cotransporter: molecular biology, functional properties, and regulation by WNKs". Am. J. Physiol. Renal Physiol. 297 (4): F838–48. doi:10.1152/ajprenal.00159.2009. PMC 3350128. PMID 19474192.
- ↑ Johnston MM, Li H, Mufson D (December 1977). "Chlorthalidone analysis using carbonic anhydrase inhibition". J Pharm Sci. 66 (12): 1735–8. PMID 411910.
- ↑ Shahin MH, Johnson JA (April 2016). "Mechanisms and pharmacogenetic signals underlying thiazide diuretics blood pressure response". Curr Opin Pharmacol. 27: 31–7. doi:10.1016/j.coph.2016.01.005. PMC 4915478. PMID 26874237.
- ↑ name=Roush2013>Roush GC, Buddharaju V, Ernst ME (July 2013). "Is chlorthalidone better than hydrochlorothiazide in reducing cardiovascular events in hypertensives?". Curr. Opin. Cardiol. 28 (4): 426–32. doi:10.1097/HCO.0b013e3283622075. PMID 23736816.
- ↑ name=Ernst>Ernst ME, Carter BL, Zheng S, Grimm RH (April 2010). "Meta-analysis of dose-response characteristics of hydrochlorothiazide and chlorthalidone: effects on systolic blood pressure and potassium". Am. J. Hypertens. 23 (4): 440–6. doi:10.1038/ajh.2010.1. PMID 20111008.
- ↑ Olde Engberink RH, Frenkel WJ, van den Bogaard B, Brewster LM, Vogt L, van den Born BJ (May 2015). "Effects of thiazide-type and thiazide-like diuretics on cardiovascular events and mortality: systematic review and meta-analysis". Hypertension. 65 (5): 1033–40. doi:10.1161/HYPERTENSIONAHA.114.05122. PMID 25733241.
- ↑ Roush GC, Abdelfattah R, Song S, Kostis JB, Ernst ME, Sica DA (June 2018). "Hydrochlorothiazide and alternative diuretics versus renin-angiotensin system inhibitors for the regression of left ventricular hypertrophy: a head-to-head meta-analysis". J. Hypertens. 36 (6): 1247–1255. doi:10.1097/HJH.0000000000001691. PMID 29465713.
- ↑ Pearle MS, Roehrborn CG, Pak CY (November 1999). "Meta-analysis of randomized trials for medical prevention of calcium oxalate nephrolithiasis". J. Endourol. 13 (9): 679–85. doi:10.1089/end.1999.13.679. PMID 10608521.
- ↑ Fink HA, Wilt TJ, Eidman KE, Garimella PS, MacDonald R, Rutks IR, Brasure M, Kane RL, Ouellette J, Monga M (April 2013). "Medical management to prevent recurrent nephrolithiasis in adults: a systematic review for an American College of Physicians Clinical Guideline". Ann. Intern. Med. 158 (7): 535–43. doi:10.7326/0003-4819-158-7-201304020-00005. PMID 23546565.
- ↑ Wolfgram DF, Gundu V, Astor BC, Jhagroo RA (August 2013). "Hydrochlorothiazide compared to chlorthalidone in reduction of urinary calcium in patients with kidney stones". Urolithiasis. 41 (4): 315–22. doi:10.1007/s00240-013-0568-5. PMID 23660825.
- ↑ Dvorak MM, De Joussineau C, Carter DH, et al. (2007). "Thiazide diuretics directly induce osteoblast differentiation and mineralized nodule formation by targeting a NaCl cotransporter in bone". J. Am. Soc. Nephrol. 18 (9): 2509–16. doi:10.1681/ASN.2007030348. PMC 2216427. PMID 17656470.
- ↑ Aung K, Htay T (October 2011). "Thiazide diuretics and the risk of hip fracture". Cochrane Database Syst Rev (10): CD005185. doi:10.1002/14651858.CD005185.pub2. PMID 21975748.
- ↑ Puttnam R, Davis BR, Pressel SL, Whelton PK, Cushman WC, Louis GT, Margolis KL, Oparil S, Williamson J, Ghosh A, Einhorn PT, Barzilay JI (January 2017). "Association of 3 Different Antihypertensive Medications With Hip and Pelvic Fracture Risk in Older Adults: Secondary Analysis of a Randomized Clinical Trial". JAMA Intern Med. 177 (1): 67–76. doi:10.1001/jamainternmed.2016.6821. PMID 27893045.
- ↑ Verbalis JG (May 2003). "Diabetes insipidus". Rev Endocr Metab Disord. 4 (2): 177–85. PMID 12766546.
- ↑ ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group (18 December 2002). "Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT)". JAMA. 288 (23): 2981–97. doi:10.1001/jama.288.23.2981. PMID 12479763.
- ↑ "Diuretic Agents", Kirk-Othmer Encyclopedia of Chemical Technology (5th ed.), 2001, doi:10.1002/0471238961.0409211803051822.a01
- ↑ DiNicolantonio JJ, O'Keefe JH, Wilson W (2018). "Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis". Open Heart. 5 (1): e000668. doi:10.1136/openhrt-2017-000668. PMC 5786912. PMID 29387426.
- ↑ Ware JS, Wain LV, Channavajjhala SK, Jackson VE, Edwards E, Lu R, Siew K, Jia W, Shrine N, Kinnear S, Jalland M, Henry AP, Clayton J, O'Shaughnessy KM, Tobin MD, Schuster VL, Cook S, Hall IP, Glover M (September 2017). "Phenotypic and pharmacogenetic evaluation of patients with thiazide-induced hyponatremia". J. Clin. Invest. 127 (9): 3367–3374. doi:10.1172/JCI89812. PMC 5669583. PMID 28783044.
- ↑ "Yasir Shah provisionally suspended after failed drugs test". BBC News. December 27, 2015.