Tafamidis
Tafamidis, sold under the brand names Vyndaqel and Vyndamax among others,[2] is a medication used to delay loss of peripheral nerve function in adults with familial amyloid polyneuropathy (FAP).[3] It works by stabilizing the protein transthyretin.[3] In people with FAP these strands separate and form clumps that harm nerves. It is also used for the treatment of heart disease (cardiomyopathy) caused by transthyretin mediated amyloidosis (ATTR-CM).[4]
 | |
| Clinical data | |
|---|---|
| Trade names | Vyndaqel, Vyndamax, others |
| AHFS/Drugs.com | Monograph |
| License data | |
| Routes of administration | By mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.246.079 |
| Chemical and physical data | |
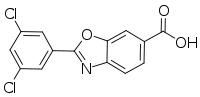
| Formula | C14H7Cl2NO3 |
| Molar mass | 308.11 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
The medication was approved for medical use in Europe in 2011, and in Japan in 2013.[3][5] It was initially rejected in the United States in 2012, then approved in 2019.[4] In the United States two preparations, tafamidis meglumine and tafamidis, were approved for the treatment of transthyretin mediated cardiomyopathy (ATTR-CM).[4][6][7] The two preparations have the same active moiety, tafamidis, but they are not substitutable on a milligram to milligram basis.[4]
Medical use
Tafamidis is used to delay impairment of peripheral nerve function in adults with familial amyloid polyneuropathy (FAP).[1][8][2] It is taken by mouth.[1][2] It is also used for the treatment of the heart disease (cardiomyopathy) caused by transthyretin mediated amyloidosis (ATTR-CM).[4]
Women should not get pregnant while taking it and should not breast feed while taking it. People with FAP who have received a liver transplant should not take it.[1]
Adverse effects
More than 10% of people in clinical trials had one or more of urinary tract infections, vaginal infections, upper abdominal pain, or diarrhea.[1]
Interactions
Tafamidis does not appear to interact with cytochrome P450 but does inhibit BCRP, so is likely to affect availability of drugs including methotrexate, rosuvastatin, and imatinib, and inhibits OAT1 and OAT3 so is likely to interact with NSAIDs and other drugs that rely on those transporters.[1]
Pharmacology
Tafamidis is a pharmacological chaperone that stabilizes the correctly folded tetrameric form of the transthyretin (TTR) protein by binding in one of the two thyroxine-binding sites of the tetramer.[8] In people with FAP, the individual monomers fall away from the tetomer, misfold, and aggregate; the aggregates harm nerves.[8]
The maximum plasma concentration is achieved around two hours after dosing; in plasma it is almost completely bound to proteins. Based on preclinical data, it appears to be metabolized by glucuronidation and excreted via bile; in humans, around 59% of a dose is recovered in feces, and approximately 22% in urine.[1]
Chemistry
The chemical name of tafamidis is 2-(3,5-dichlorophenyl)-1,3-benzoxazole-6-carboxylic acid. The molecule has two crystalline forms and one amorphous form; it is manufactured in one of the possible crystalline forms. It is marketed as a meglumine salt. It is slightly soluble in water.[9]
History
The laboratory of Jeffery W. Kelly began looking for ways to inhibit TTR fibril formation in the 1990s.[10]:210 Tafamidis was eventually discovered by Kelly's team using a structure-based drug design strategy; the chemical structure was first published in 2003.[11][12] In 2003, Kelly co-founded a company called FoldRx with Susan Lindquist of MIT and the Whitehead Institute[12][13] and FoldRx developed tafamidis up through submitting an application for marketing approval in Europe in early 2010.[11] FoldRx was acquired by Pfizer later that year.[11]
Tafamidis was approved by the European Medicines Agency (EMA) in November 2011, to delay peripheral nerve impairment in adults with transthyretin-related hereditary amyloidosis.[8] The U.S. Food and Drug Administration (FDA) rejected the application for marketing approval in 2012, on the basis that the clinical trial did not show efficacy based on a functional endpoint, and the FDA requested further clinical trials.[14] In May 2019, the FDA approved two tafamidis preparations, Vyndaqel (tafamidis meglumine) and Vyndamax (tafamidis), for the treatment of transthyretin mediated cardiomyopathy (ATT-CM).[4] The drug was approved in Japan in 2013; regulators there made the approval dependent on further clinical trials showing better evidence of efficacy.[5]
The FDA approved tafamidis meglumine based primarily on evidence from a clinical trial (NCT01994889) of 441 adult patients.[7] The trial was conducted at 60 sites in Belgium, Brazil, Canada, Czech Republic, Spain, France, Greece, Italy, Japan, Netherlands, Sweden, Great Britain, and the United States.[7]
There was one trial that evaluated the benefits and side effects of tafamidis for the treatment of ATTR-CM.[7] In the trial, patients with ATTR‑CM were randomly assigned to receive either tafamidis (either 20 or 80 mg) or placebo for 30 months.[7] About 90% of patients in the trial were taking other drugs for heart failure (consistent with the standard of care).[7]
The EMA designated tafamidis an orphan medicine[3] and the FDA designated tafamidis meglumine an orphan drug.[15]
References
- "Vyndaqel 20 mg soft capsules - Summary of Product Characteristics". Electronic Medicines Compendium. Retrieved 2 April 2018.
- "Vyndaqel- tafamidis meglumine capsule, liquid filled Vyndamax- tafamidis capsule, liquid filled". DailyMed. 30 August 2019. Retrieved 24 November 2019.
- "Vyndaqel EPAR". European Medicines Agency (EMA). 16 October 2019. Retrieved 24 November 2019.
- "FDA approves new treatments for heart disease caused by a serious rare disease, transthyretin mediated amyloidosis". U.S. Food and Drug Administration (FDA). 14 September 2019. Archived from the original on 14 September 2019. Retrieved 24 November 2019.

- "Report on the Deliberation Results" (PDF). Evaluation and Licensing Division, Pharmaceutical and Food Safety Bureau Ministry of Health, Labour and Welfare. 2 September 2013.
- "Drug Approval Package: Vyndaquel & Vyndamax". U.S. Food and Drug Administration (FDA). 13 June 2019. Retrieved 24 November 2019.

- "Drug Trial Snapshots: Vyndaqel/Vyndamax". U.S. Food and Drug Administration (FDA). 28 May 2019. Archived from the original on 19 December 2019. Retrieved 18 December 2019.

- Said, G; Grippon, S; Kirkpatrick, P (1 March 2012). "Tafamidis". Nature Reviews. Drug Discovery. 11 (3): 185–6. doi:10.1038/nrd3675. PMID 22378262.
- "Assessment report: Vyndaqel tafamidis meglumine Procedure No.: EMEA/H/C/002294" (PDF). EMA. 2011. See EMA index page for updates.
- Labaudiniere, Richard (2014). "Chapter 9: Discovery and Development of Tafamidis for the Treatment of TTR Familial Amyloid Polyneuropathy". In Pryde, David C; Palmer, Michael J (eds.). Orphan Drugs and Rare Diseases. RSC Drug Discovery Series No. 38. Royal Society of Chemistry. ISBN 978-1-84973-806-4.
- Jones, Dan (29 October 2010). "Modifying protein misfolding". Nature Reviews Drug Discovery. 9 (11): 825–827. doi:10.1038/nrd3316.
- Borman, Stu (25 January 2010). "Attacking Amyloids". Chemical & Engineering News. 88 (4): 30–32. doi:10.1021/cen-v088n004.p030.
- Breznitz, Shiri M.; O'Shea, Rory P.; Allen, Thomas J. (March 2008). "University Commercialization Strategies in the Development of Regional Bioclusters". Journal of Product Innovation Management. 25 (2): 129–142. doi:10.1111/j.1540-5885.2008.00290.x.
- Grogan, Kevin (19 June 2012). "FDA rejects Pfizer rare disease drug tafamidis". Pharma Times.
- "Tafamidis meglumine Orphan Drug Designation and Approval". U.S. Food and Drug Administration (FDA). 3 May 2019. Archived from the original on 19 December 2019. Retrieved 18 December 2019.

Further reading
- Adams D (March 2013). "Recent advances in the treatment of familial amyloid polyneuropathy". Ther Adv Neurol Disord. 6 (2): 129–39. doi:10.1177/1756285612470192. PMC 3582309. PMID 23483184.
- Coelho T, Maia LF, Martins da Silva A, et al. (August 2012). "Tafamidis for transthyretin familial amyloid polyneuropathy: a randomized, controlled trial". Neurology. 79 (8): 785–92. doi:10.1212/WNL.0b013e3182661eb1. PMC 4098875. PMID 22843282.
External links
- "Tafamidis". Drug Information Portal. U.S. National Library of Medicine.
- "Tafamidis meglumine". Drug Information Portal. U.S. National Library of Medicine.