Male infertility crisis
The male infertility crisis is a term that has risen to prominence driven by the popular media in the 20th and 21st century. Subsequently, later having been adopted by the medical academic research in studying male infertility .[1] The term of male fertility crisis has now been adopted to become a study subject itself.[2] The male infertility crisis has been described as the ongoing rapid decrease in sperm quality and subsequent challenges in male infertility. The earliest indications of this decrease first emerged in the 1970s. From this period there has been a steady decline of 1.4% in sperm counts.[3][4] The matter is particularly relevant in the west in New Zealand, Australia, Europe & North America. A reduction in other parts of the world has yet to be observed.[5]
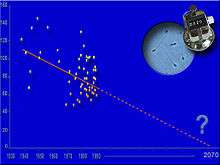 Declining trend in male sperm over the last 50 years | |
| Related | Male Infertility, Sub-replacement fertility, sperm quality, female infertility, Testicular infertility factors |
|---|---|
In its original form, it had begun as a study on male fertility. Evolving into a term used by journalists in the media as a common headline for the reporting for studies concerning sperm, infertility and declining male sexual performance.[2]
Hypotheses for the causes of the crisis is still subject to ongoing further research. From existing research cites lifestyle factors and the presence of hormone-disrupting chemicals in the environment.[5]
The effects and the issues caused are in the progress of development. As the understanding of the effects on individuals, family and society are ongoing subjects for further studies.
This topic has been subject to rigorous debate in regards to the nature and exact degree of crisis that is exhibited in male fertility. However, it has generally been accepted within the scientific community as a key issue of male health.[6] Their aim is to bring the issue to the forefront of media and to public attention.
As a consequence, responses to address the crisis have begun to occur with developments in frameworks to support those who are experiencing male infertility and academic research to remedy the issue.
Usage of the term
The first uses of the term being used stem as far back as the early 1970s with suggestions it may have emerged earlier in the 1960s.[7] However, significant traction for the issue as it becomes further highlighted by the 1990s when it became more commonly studied, thus subsequent attention is paid to the issue. The term has become a catch-all term as part of the discussion of the health issues of men. There is now ongoing media coverage on the issue often being used as a common headline driver.
Research analysis has found amongst a sample of British newspapers in the 1990s there had been a recognisable discourse in the tone of a crisis.[2] In recent years, there has been substantial growth in the frequency of media coverage often coinciding and in response with releases of studies. Mass media coverage is subject to significant controversy as the use of terms such as "crisis", "apocalypse" "timebomb" and "threat to human race" have led to arguments that it has given rise to clickbait or hysterical coverage elevating fears within the community.[7][8]
Various tabloid media agencies have published various pieces with headlines that have supported the notion of crisis. Examples include from GQ labelling it “the truth behind the shocking drop in sperm counts,” followed by a Newsweek front page cover “Who’s Killing America’s Sperm?” and with the New York Times stating it as “male infertility crisis is coming” [9][10][11]
Discussions of the usage of the terminology of male infertility crisis by the media have been evident through various comparisons. For the emphasis of the crisis, one example drew a time-series comparisons between the present-day generations and past generations i.e. fathers and grandfathers or geographic comparisons within countries or to other regions. Further stark comparisons include drawing similarities to other species notably rats and hamsters. [2] Some have compared the long term effects with the fertility collapse in dystopian fictional works such as Children of Men and The Handmaid’s Tale.[1][12]
Academia and the scientific community have agreed in consensus in favour of the use of the term.[7] Citing it as necessary to prompt preventative action to remedy the issue in the present time before it affects future generations on a greater scale. While others such as social commentators have argued the wide-ranging consequences that follow the male infertility crisis necessitate the use of crisis terminology.[13] Consequences include the subsequent inability to conceive a child. Thus, the effect of involuntary childlessness can be viewed as a crisis.[14]
Development and History
Beginning in the 1970s & 1980s, the first studies were published that observed declines in the sperm quality and later sperm quantities of men. One of the earliest studies in a paper published in 1974 by Nelson et al. had observed decreases in the sperm quality with lower concentrations and volumes in particular increase in the percentage of observations with abnormalities in sperm.[15] Often these earlier findings have been criticised in the conduct having been cited for various faults including issues of sampling selection and various other inaccuracies in the obtaining of data.[7] There were various reports published in the 1970s & 1980s that had not found similar declines. An example is a research paper by Niecheslag et al. in 1982 concluded no decline. Instead found no parameter changes in sperm.[16] However, the claims are not completely unfounded it reflected a general shift in societal patterns changes in sexual behaviour, the prevalence drugs, preferences for later marriages and fatherhood that brought the earliest signs to attention[17]
In 1980 the World Health Organisation published its first publication, a laboratory manual for semen analysis. This set the parameters for the worldwide measurement standards in sperm quality and normality.[18]

Limited research in the 1980s found the first signs behind the decline with links to general environmental degradation.[17]
The 1990s
This period saw a significant development in the research where results began to show the first signs of conclusive data to prove a true decline.A landmark 1992 Danish study commonly referred to as the Carlsen study after the principal author had reached following an analysis of a range of studies from 1938-1990 from a population described as healthy men had experienced a sharp decline during the aforementioned period.[10][19] Following this study, substantial funding is given to further studies which are conducted to support this thesis to attempt to find causes that have driven the decline.
In the late 1990s, the first studies on the social and psychological impact of the crisis are published.[20]
Towards the end of the 1990s, the earliest breakthrough in the development of remedies for the male infertility crisis is found with the use of the technique known as Intracytoplasmic sperm injection (ICSI).[21]
Recent developments
By the 2010s it had become very clear, there had been significant declines with a steady decrease in sperm quality and quantity. There had now been wide-ranging publications particularly in the beginnings of the causes for the decline. In one meta-analysis study published in 2017 by Hebrew University had concluded decreases in sperm concentrations up to 52.4% and similarly a decrease of 59.3% in total sperm numbers.[22] Two follow on studies in the year 2018 presented at the Scientific Congress of the American Society for Reproductive Medicine (ASRM) had observed similar findings to find sperm counts had reduced and lower mobility of sperm during the 2000s.[7]
A 2012 paper published by French researchers and the Institute for Public Health in the Journal of Human Reproduction studied French males between the period of 1989–2005. They concluded the sperm counts and the proportion of normal sperm fell by 32.2% and 8.1% respectively.[23][24]
Further research had supported evidence in the role of lifestyle factors and further impact of socioeconomic status. One of the latest studies published in February 2020 journal JAMA Network Open had investigated 4 varying diets using a sample of 2935 young Danish men. It came to the conclusion men who consumed a “western diet" composed of predominantly of red meat, fried food, and sugar-sweetened drinks and desserts had the worse outcome out of the 4 diets with a sperm count ranging from 109 million to 138 million. The study had found a prudent "healthy diet" composed of fish, chicken, fruit and vegetables. This diet had the highest sperm count with an average of 146 million to 183 million sperm. The co-author of the study stated the importance of diet citing it as "necessary for the production of healthy functioning sperm with high fertility potential” [25][26]
Discussions and controversy
The effects of the crisis are still being understood apart from the well-known correlated issue of directly affecting fertility rates and child birthing rates. The debate remains within the andrology community on the conclusive nature of the evidence to support the claims of crisis. Consequential reasoning for the causes of the crisis is still subject to controversy. Perspectives range on the issue with some viewing it from a biological viewpoint with the focus on causes and medical effects. The research-based in a clinical quantitative lab-based setting has been the traditional biological viewpoint.
Sociology perspective
Sociologists studying the topic focus on the effect on society and cultures. This domain seeks to be more based on human experiences with a focus on mental and emotional aspects in particular metrics of emotional wellbeing and stress.[27]Sociology studies are part of research seeking to broaden the perspectives on the matter bringing to focus other aspects of the fertility crisis. Traditionally the topic of fertility has been exclusively on women with men sidelined.[20]
Criticisms
Critics of the study of male infertility crisis have cited research that has in part led to the stigmatization of men. The infertility crisis has become conflated with other health-related matters particularly with mental health with the potential of trauma and worthlessness. Spillover effects into society to male vulnerability and perceived threats to male status. Direct evidence that supports claims of stigmatisation caused by men experiencing the fertility crisis is lacking, however.[28]
Various researchers in this area argue not enough research has been conducted and thus, lacks the extensive scientific database relative to other fields of medicine or female fertility. It may be part of the issue to find remedies or lead to remedies that are sub-optimal.[29]
There is a debate on the degree of the effect of the crisis with arguments about the impact of the rate of decline. Sperm has declined (99 million sperm per ml) in 1970 to (47 million sperm per mL) 2011.[30] It remains in a relatively normal range above the 15 million WHO considers below normal. The issue of most concern is the reduction in averages of abnormal sperm counts.
Health practitioners and fertility doctors who work in the field are sceptical of the notion of crisis in male fertility as they had not observed a dramatic decline from the first-hand experience. There is a disconnect between what has been studied in the published research and what is observed in public.[31]
Other Issues
The existing methods to attempt to remedy the issue of fertility that are most commonly used for example Assisted Reproductive Technology (ART) is known to have complications, it is often viewed as expensive and lacking effective access.[32]
Responses
There has been much academic research now focusing on attempts to remedy the issue. Proponents argue more needs to be done on causes, in particular, the role of lifestyle factors and a reduction of exposure to environmental chemicals.[33][6] The thought within the medical community that calls for the breaking down of the stigma that surrounds male fertility requiring a cultural shift to emphasize the importance of the issue as part of the continued decline in health outcomes.[27][34]
Advocates and proponents of the topic of male infertility have argued for modernization and reform of the health care system through improved practices and increased levels of funding. They argue the role of private health insurance and government to be potential leaders in this area.[35]
Social programs to alleviate the impact of the crisis have been implemented as part of a framework of men's reproductive health to address the crisis. Various awareness groups in male reproductive health now exist examples include Men's Health Week and international male health awareness program of Movember.[36][37]
Within Australia, the federal government established funding for the Healthy Male a program intended to support male reproductive health and fertility. Further efforts include an award of a grant in this area of approximately $3million to Andrology Australia.[38]
Other national government responses include advice provided by the UK National Health Service (NHS) recommending a healthy lifestyle and loose-fitting underwear to improve sperm thus fertility.[39]
Organisations in the medical field have been established to address the crisis. Most notably the Male Reproductive Health Initiative a group focused on male fertility in the attempts to foster and support reform and action to address the issue to enable improvements in outcomes.[6]
References
- McKie, Robin (2017-07-29). "The infertility crisis is beyond doubt. Now scientists must find the cause". The Guardian. Retrieved 2018-10-10.
- Gannon, Kenneth; Glover, Lesley; Abel, Paul (2004). "Masculinity, infertility, stigma and media reports". Social Science & Medicine. 59 (6): 1169–1175. doi:10.1016/j.socscimed.2004.01.015. PMID 15210089.
- Levine, Hagai; Jørgensen, Niels; Martino-Andrade, Anderson; Mendiola, Jaime; Weksler-Derri, Dan; Mindlis, Irina; Pinotti, Rachel; Swan, Shanna H (2017-07-25). "Temporal trends in sperm count: a systematic review and meta-regression analysis". Human Reproduction Update. 23 (6): 646–659. doi:10.1093/humupd/dmx022. ISSN 1355-4786. PMC 6455044. PMID 28981654.
- Davis, Nicola (2017-07-25). "Sperm counts among western men have halved in last 40 years – study". The Guardian. Retrieved 2018-10-10.
- Johnston, Ian (25 July 2017). "Western men's sperm counts plunge 60% in 40 years due to 'modern life'". The Independent. Retrieved 2018-10-10.
- De Jonge, C.; Barratt, C.L. R. (2019). "The present crisis in male reproductive health: an urgent need for a political, social, and research roadmap". Andrology. 7 (6): 762–768. doi:10.1111/andr.12673. ISSN 2047-2919. PMID 31241256.
- Fetters, Ashley (2018-10-12). "Sperm Counts Continue to Fall". The Atlantic. Retrieved 2020-05-28.
- Nieschlag, Eberhard; Lerchl, Alexander (2013). "Sperm crisis: what crisis?". Asian Journal of Andrology. 15 (2): 184–186. doi:10.1038/aja.2012.90. ISSN 1008-682X. PMC 3739166. PMID 23001441.
- Halpern, Daniel Noah. "What Happens If We Hit Sperm Count Zero?". GQ. Retrieved 2020-05-28.
- Walsh, Bryan (2017-09-12). "The male infertility crisis: Who's killing America's sperm?". Newsweek. Retrieved 2018-10-10.
- Inhorn, Marcia C. (October 21, 2017). "Opinion | A Male Infertility Crisis Is Coming. The Middle East Can Help". The New York Times. Retrieved 2018-10-10.
- "Why the male infertility crisis could be good news for women". New Scientist. Retrieved 2018-10-10.
- F, Fahami; Sh, Quchani; S, Ehsanpour; Az, Boroujeni (2010). "Lived Experience of Infertile Men With Male Infertility Cause". Iranian Journal of Nursing and Midwifery Research. 15 (Suppl 1): 265–71. PMC 3208938. PMID 22069398.
- Morse, Carol A.; Van Hall, Eylard V. (1987). "Psychosocial aspects of infertility: A review of current concepts". Journal of Psychosomatic Obstetrics & Gynecology. 6 (3): 157–164. doi:10.3109/01674828709019419. ISSN 0167-482X.
- Nelson, C.M. Kinloch; Bunge, Raymond G. (1974). "Semen Analysis: Evidence for Changing Parameters of Male Fertility Potential". Fertility and Sterility. 25 (6): 503–507. doi:10.1016/S0015-0282(16)40454-1. PMID 4835605.
- Kumar, Naina; Singh, AmitKant (2015). "Trends of male factor infertility, an important cause of infertility: A review of literature". Journal of Human Reproductive Sciences. 8 (4): 191. doi:10.4103/0974-1208.170370. ISSN 0974-1208. PMID 26752853.
- Bouton, Katherine (1982-06-13). "Fighting Male Infertility". The New York Times. ISSN 0362-4331. Retrieved 2020-05-28.
- "Aktuelles". Praxis. 92 (20): 978. 2003. doi:10.1024/0369-8394.92.20.978. ISSN 0369-8394.
- Carlsen, E.; Giwercman, A.; Keiding, N.; Skakkebaek, N. E. (1992-09-12). "Evidence for decreasing quality of semen during past 50 years". BMJ (Clinical Research Ed.). 305 (6854): 609–613. doi:10.1136/bmj.305.6854.609. ISSN 0959-8138. PMC 1883354. PMID 1393072.
- Webb, Russell E.; Daniluk, Judith C. (1999). "The End of the Line: Infertile Men's Experiences of Being Unable to Produce a Child". Men and Masculinities. 2 (1): 6–25. doi:10.1177/1097184X99002001002. ISSN 1097-184X.
- Endocrine disruptors : effects on male and female reproductive systems. Naz, Rajesh K. (2nd ed.). Boca Raton: CRC Press. 2005. ISBN 0-8493-2281-2. OCLC 55634444.CS1 maint: others (link)
- Levine, Hagai; Jørgensen, Niels; Martino-Andrade, Anderson; Mendiola, Jaime; Weksler-Derri, Dan; Mindlis, Irina; Pinotti, Rachel; Swan, Shanna H. (1 November 2017). "Temporal trends in sperm count: a systematic review and meta-regression analysis". Human Reproduction Update. 23 (6): 646–659. doi:10.1093/humupd/dmx022. ISSN 1460-2369. PMC 6455044. PMID 28981654.
- "Countdown". The Economist. ISSN 0013-0613. Retrieved 2020-05-28.
- Rolland, M.; Le Moal, J.; Wagner, V.; Royère, D.; De Mouzon, J. (2013). "Decline in semen concentration and morphology in a sample of 26 609 men close to general population between 1989 and 2005 in France". Human Reproduction. 28 (2): 462–470. doi:10.1093/humrep/des415. ISSN 1460-2350. PMID 23213178.
- Pattillo, Ali. "Study of 2,935 men reveals one diet may solve the "infertility crisis"". Inverse. Retrieved 2020-05-28.
- Nassan, Feiby L.; Jensen, Tina K.; Priskorn, Lærke; Halldorsson, Thorhallur I.; Chavarro, Jorge E.; Jørgensen, Niels (2020-02-21). "Association of Dietary Patterns With Testicular Function in Young Danish Men". JAMA Network Open. 3 (2): e1921610. doi:10.1001/jamanetworkopen.2019.21610. ISSN 2574-3805. PMC 7043196. PMID 32083688.
- Petok, William D. (2015). "Infertility counseling (or the lack thereof) of the forgotten male partner". Fertility and Sterility. 104 (2): 260–266. doi:10.1016/j.fertnstert.2015.04.040. PMID 26048155.
- Hanna, Esmée; Gough, Brendan (2015-12-23). "Experiencing Male Infertility: A Review of the Qualitative Research Literature". SAGE Open. 5 (4): 215824401561031. doi:10.1177/2158244015610319. ISSN 2158-2440.
- "Tackling the stigma around male infertility". Raconteur. 2018-04-23. Retrieved 2020-05-28.
- "expert reaction to meta-analysis of sperm count among men in Western countries | Science Media Centre". Retrieved 2020-05-28.
- Belluz, Julia (2018-09-17). "Sperm counts are falling. This isn't the reproductive apocalypse — yet". Vox. Retrieved 2020-05-28.
- Ravitsky, Vardit; Kimmins, Sarah (2019-11-21). "The forgotten men: rising rates of male infertility urgently require new approaches for its prevention, diagnosis and treatment". Biology of Reproduction. 101 (5): 872–874. doi:10.1093/biolre/ioz161. ISSN 0006-3363. PMID 31553040.
- Berry, Sarah (2017-07-26). "'We are not in crisis yet': 60 per cent drop in sperm count can be reversed". The Sydney Morning Herald. Retrieved 2020-05-28.
- Ravitsky, Vardit; Kimmins, Sarah (2019-11-21). "The forgotten men: rising rates of male infertility urgently require new approaches for its prevention, diagnosis and treatment". Biology of Reproduction. 101 (5): 872–874. doi:10.1093/biolre/ioz161. ISSN 0006-3363. PMC 6877781. PMID 31553040.
- "Opinion: Impending fertility crisis requires urgent action". Montreal Gazette. Retrieved 2020-05-28.
- "Home". Men's Health Week. Retrieved 2020-05-28.
- "Movember". Movember. Retrieved 2020-05-28.
- "$19.7 million National Men's Health Strategy". Greg Hunt MP. Retrieved 2020-05-28.
- "Why tomato puree might improve male fertility". BBC News. 2019-10-09. Retrieved 2020-05-28.